Translate this page into:
The Palliative Care Knowledge Questionnaire-Basic (PCKQ-B): Development and Validation of a Tool to Measure Knowledge of Health Professionals about Palliative Care in India
*Corresponding author: Megha Pruthi, S 804, Omaxe twin tower, F block, Sector 50, Noida, Uttar Pradesh, India. dr.meghapruthi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pruthi M, Bhatnagar S, Indrayan A, Chanana G. The palliative care knowledge questionnaire-basic (PCKQ-B): Development and validation of a tool to measure knowledge of health professionals about palliative care in India. Indian J Palliat Care 2022;28:180-91.
Abstract
Objectives:
A well-educated and aware staff are the needed to overcome barriers to palliative care provision in the face of ever-increasing needs of palliative care in developing countries like India. Lack of a standardised and locally validated need assessment tool is felt as one of the important requirements for any successful educational program. This project is to develop and validate a basic palliative care knowledge needs assessment questionnaire.
Materials and Methods:
Development of Palliative Care Knowledge Questionnaire-Basic (PCKQ-B) for Indian nurses working in a tertiary care hospital in Delhi-NCR, India was undertaken with four basic processes, that is, item generation, content validity, pilot testing and field testing. Literature search helped us to find appropriate domains and items; content validity obtained with a panel of seven experts, pilot testing and finally field testing was done on 102 nurses working in 6 branches of Max Super Specialty Hospital, Delhi-NCR, India. The field study data were used to do item analyses including item difficulty, item discrimination and calculate reliability indicators including test-retest correlation and KR-20.
Results:
Content Validity index (CVI) of all the items was >0.78 (except 1 item) and Scale-CVI was 0.98 (excellent content validity). Items were selected on the basis of item difficulty index of 0.1 to 0.9 and an item discrimination index greater than 0.2. A total of 25 questions were selected that elicited KR-20 value of 0.65 and intra class correlation (test-retest reliability) of 0.52.
Conclusion:
Overall, PCKQ-B is a 25 item questionnaire with a moderate reliability. Although validated for nurses in tertiary care hospitals, this tool might find utility in education of primary health workers, community health workers, social workers, or physiotherapists in palliative care teams.
Keywords
Palliative care
Nurse
Awareness
Knowledge
Evaluation
INTRODUCTION
The horizon of palliative care is ever expanding with the ongoing paradigm shift in epidemiology of diseases in developing countries. The chronic diseases and injuries are taking lead as causes of disability and mortality.[1] With this dramatic surge in chronic diseases, ageing population and incidence of cancer, it is indubitable that the need of palliative care in our society is on rise. According to the 2nd edition of white paper published by The Economist Intelligence Unit of The Economist and Lien Foundation in Singapore in 2015, India ranked 67th of 80 countries in the quality of death index (a slight improvement over the 1st edition in 2010, when India ranked last out of 40 countries).[2,3]
India’s deficient performance is a result of lack of knowledge, awareness, inadequate availability of opioids and ‘defensive practice of medicine’ because of ambiguous legal stance on End of life care.[4] Our medical and nursing schools have little or none to teach about palliative medicine and end of life care.[5-7] Thus creating a huge gap between need and knowledge of palliative care among health professionals in our country. Empowering nurses with knowledge is pivotal to development of palliative care.
There are many knowledge assessment questionnaires for nurses, two of these validated questionnaires, Palliative Care Quiz for Nursing (PCQN) (Canada, 1996),[8] and Palliative Care Knowledge Test (PCKT) (Japan, 2009)[9] are commonly used. Among others are Palliative Care Survey (PCS), Knowledge regarding Palliative Care Consultation Services Inventory (K-PCCSI), etc., validated in other parts of the world.[10,11] However, there are certain differences in working conditions and role in health care system that make nurses in Indian context somewhat different from western world. A ‘doctor centred health system’[12] where nurse’s principal role is to passively carry out the instructions given by the doctors.[12] Differences in basic training and the fact they usually do not prescribe or administer medicines on their own, (except in few conditions where they are specially trained to do so for e.g. certain home care teams) leads to limited knowledge about drugs.[12] Moreover, religious, cultural and ethical factors differentiate Indian nurses from nurses in other populations.[13,14]
There is paucity of any standardised and validated palliative care knowledge questionnaire for Indian nurses, hence need of a complete questionnaire, that is concise, covers most or all aspects of palliative care and gives a clear picture of the present state of nurse’s knowledge was realised. In addition to be needs assessment tool, the questionnaire is also intended to bring out misconceptions and myths about palliative care and opioids and to stimulate discussions over importance of palliative care among the staff nurses, educators and administrators. When utilised as pre-test, it will generate more interest, increase receptivity in educational activity by the participants and willingness to discuss and interact.
Aims and objectives of the study
The aim of the study was to develop and validate a tool (Palliative Care Knowledge Questionnaire-Basic, [PCKQ-B]) to assess current level of knowledge of palliative care among nurses working in tertiary care hospitals in India.
MATERIALS AND METHODS
An advisory committee of palliative care physicians and a statistician provided direction through the entire process of development. Literature search was performed using Medline via PubMed, CINAHL and Google scholar to find the available tools used to assess basic palliative care knowledge amongst nurses or other health-care professionals in India and across the world. The final search strategy for PubMed was ((((((knowledge OR understanding OR education OR comprehension OR awareness OR philosophy))) AND ((nurs* OR ‘registered nurs*’ OR ‘staff nurs*’ OR ‘nurse practitioners’))) AND ((‘Palliative care’ OR ‘hospice care’ OR ‘palliative medicine’ OR ‘terminal care’ OR ‘end of life care’ OR ‘supportive care’ OR ‘supportive oncology’))) AND ((‘Surveys and Questionnaires’ OR quiz OR instrument OR scale))) AND English [lang].
In a similar way, CINAHL database was interrogated by access provided via EBSCO. Finally, Google scholar search (first 100 hits, sorted by relevance) proved to be useful to access unpublished academic research from conference proceedings and some relevant articles from non-indexed journals.
[Figure 1] summarises the of selection of retrieved articles from all the sources.
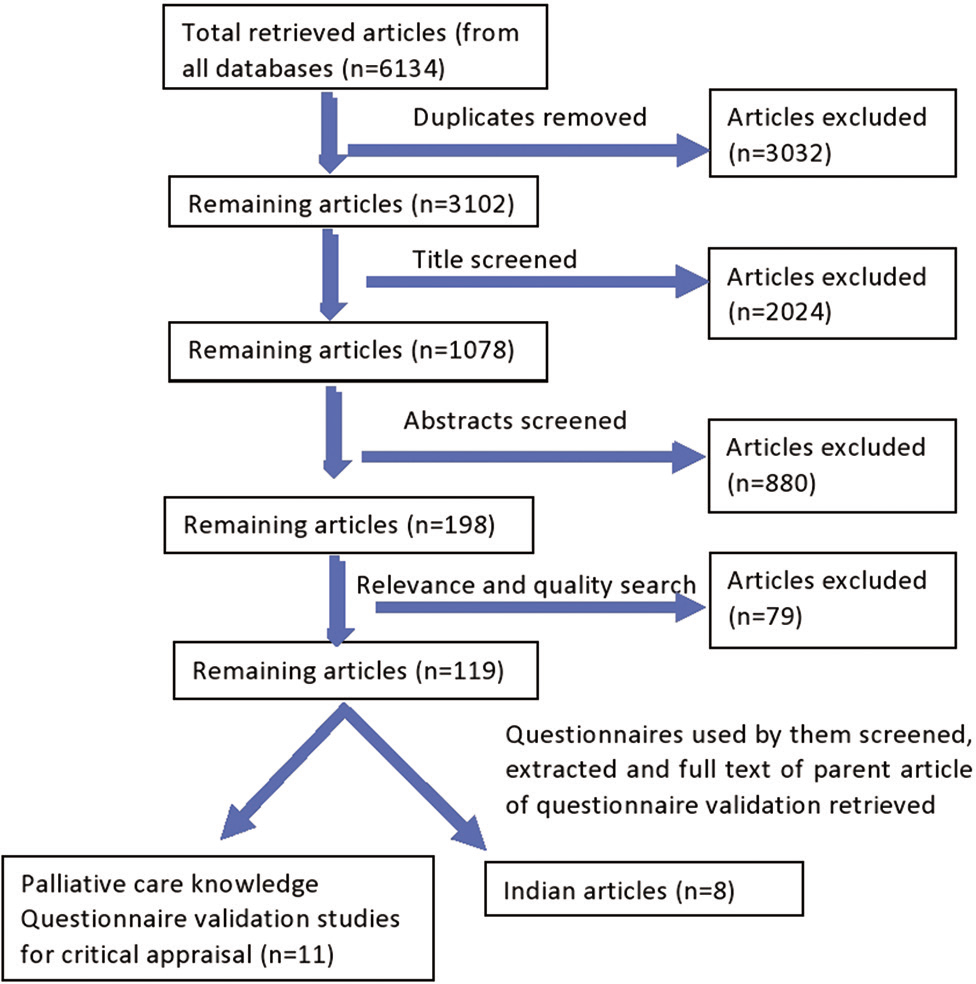
- Summary of selection of retrieved articles.
The questionnaires used by 119 articles were extracted. The parent articles for validation of these questionnaires were noted from their reference list and searched for full text. Non-validated, self-developed questionnaires based on teaching modules of the respective countries (non-Indian) were excluded from the study. Indian studies were preferably included for full text critical review to find the questions used by the different authors, even if the article was established not to be of appropriate quality as per the Specialist Unit for Review Evidence.[15]
At the end if this exercise, there were a total of 19 articles, out of which 11 were palliative care knowledge questionnaire or similar validation studies and eight were studies conducted in different parts of India to assess palliative care knowledge amongst nurses or general physicians. All of these 19 articles were critically appraised and a palliative care knowledge question bank was prepared. A palliative care knowledge question bank thus created was reviewed considering Indian nursing context and basic national palliative care teaching module.
Primary principles that were kept in mind while developing this questionnaire were: development of a brief, self-administered tool, using simple English language and the content to cover most of the basic aspects of palliative care and be relevant to nursing practice.
Development of PCKQ-B is inspired by 4 phases as used by Yun et al. for development of Quality Care Questionnaire-Palliative Care: [16]
Item generation
Content validity
Pilot testing
Field testing.
Phase 1: Item generation
Five questionnaires were found especially useful to derive items for PCKQ-B. Some of the items were taken from these questionnaires without any changes (unmodified), while others were inspired (modified) from the items used by these authors. These five questionnaires were as follows:
PCQN[8]
PCKT[9]
Self-developed, 27 items (true/false/don’t know) Knowledge of home palliative cancer care questionnaire by Shimizu et al.[17]
Self-developed 39-point (true/false/don’t know) questionnaire by Sadhu et al.[5]
Self-developed 20-point (multiple choice questions) questionnaire used by Butola among general practitioner doctors working in border security forces.[18]
14 questions were self-developed based on the present basic teaching module in India [Figure 2]. These selected 69 questions were sub-divided under 14 domains that were identified to be relevant based on literature review. Based on discussion with advisory committee, informal discussion with four palliative care physicians, working in different tertiary care centres across India; and with senior colleagues and friends, some items were reviewed, merged and language modified and minor revisions were made based on their inputs. Hence PCKQ-B (Version 1) consisted of 12 domains and total 48 items. This was sent to experts for content validity.

- Summary of item generation.
Phase 2: Content validity
Content validity is defined as ‘the degree to which an instrument has an appropriate sample of items for the construct being measured’[19] This is computed by asking a panel of experts to rate all the items on a scale of 1–4 on the basis of their relevance to the construct.
1: not relevant, 2: somewhat relevant, 3: quite relevant and 4: highly relevant.[20]
Item Content Validity Index (I-CVI) is calculated as:
Number of experts giving a rating of either 3 or 4 ÷ total number of experts.[20]
Acceptability criteria being I-CVI more than 0.78.[20]
Scale Content Validity Index (S-CVI) is calculated as proportion of total items judged content valid, that is, I-CVI >0.78.[21]
The preliminary PCKQ-B was sent to seven consenting palliative care physicians and nursing experts through e-mail. Comments were also invited on clarity (appropriate use of words) and accuracy of individual questions; length, content and format of the questionnaire; any area that seemed left out and ideas to make it better and more complete.
I-CVI was found to be 1.0 for 23 items and 0.85 for 24 items. Only one item was found to have I-CVI of 0.71, which was marginally lower than the set acceptable level. The same was discussed in advisory committee and it was decided to retain the question in further analysis as it was deemed important edumetrically. Scale CVI was calculated and was found to be 0.98.
All the comments given by the experts were discussed with advisory committee. Addition, removal and rephrasing of the domains and questions based on expert comments led to PCKQ-B (Version 2) consisting of 13 domains and 52 questions (Yes/No/Don‘t know answer type).
Phase 3: Pilot testing
PCKQ-B (Version 2) was administered to ten nurses from a tertiary care hospital after written informed consent. They were asked to respond to and debrief the questionnaire. The debriefing included comments about any questions being offending, misleading, difficult to understand or needing further clarification; if they found the format of questionnaire engaging and font size appropriate to read.
The average time taken to complete the questionnaire was 13.5 min, minimum being 8 min and maximum 17 min. They found the questionnaire engaging and fonts appropriate. However, there was difficulty in understanding three terms ‘terminally ill,’ ‘dying care’ and ‘placebo’. Based on pilot testing modifications were made in ‘participant information sheet’ with addition of these definitions; however, there were no changes in the PCKQ-B (Version 2).
Phase 4: Field testing
Minimum sample size was estimated as 92. Field testing was conducted as pre-test during Continuing Nursing Education (CNE) symposium on Palliative Care where 102 nurses filled the pre-test. For test-retest reliability, the questionnaire was administered twice to 13 nurses (who had not participated in the CNE) at 1 week interval.
RESULTS
Analysis for validation of questionnaire
Responses to all the items of the PCKQ-B (Version 2) (13 domains and 52 questions, Yes/No/Don’t know answer type) were determined to be correct or incorrect. The ‘don’t know’ response was marked as incorrect. Responses were entered as codes 1 for correct and 0 for incorrect answers in an Excel spread sheet. Participants who answered more than 90% of the questions i.e. more than 47 out of 52 were included in analysis to decrease the effect of missing data on further interpretations. Hence, out of the total 102 pre-tests collected, analysis was performed on 99 participants.
Item analysis
1. Item difficulty, - was calculated using the formula:[22]
Where i is the item, n is the number of participants who responded to the item i and nCorrect,i is the number of participants who answered the item correctly. A range criterion of 0.1 to 0.9 (also used by authors of PCKT[9]) was accepted for inclusion in the final questionnaire. 3 items (or questions) with P < 0.1 and 1 item with >0.9 were removed from further item analysis.
2. Item Discrimination Index, d- was calculated as:
d = Proportion of correct answers in participants who had total scores in upper quartile - Proportion of correct answers in participants who had total scores in lower quartile.[8]
The items with d < 0.2 were excluded from the study.[23] A total of 23 items had to be excluded with d < 0.2. Among the remaining 25 items, eight had d > 0.4 (highly discriminating), five items had d value between 0.3 and 0.39 (moderately discriminating) and 12 items had d value between 0.2 and 0.29 (fairly discriminating).
This left us with 25 questions that were subjected to reliability analyses.
Reliability
1. Test-retest reliability: Test-retest reliability was calculated as Intra Class Correlation (ICC) with two-way mixed effects model using a consistency definition. It was found to be 0.52 for PCKQ-B, which is a fair correlation according to Cicchetti’s criterion,[24]
2. Kuder-Richardson Formula (KR 20): was calculated as:
where k = number of items, pi = proportion of correct responses to test item i (item difficulty index), qi = proportion of incorrect responses to test item i, = variance of the total scores of all the examinees.
KR 20 value can range from 0 to 1.[25] Many authors have used a cut off >0.7 for an instrument to be reliable,[8,9,26] however, KR 20 > 0.5 might be considered acceptable for early research purposes.[25] KR-20 index value for PCKQ-B was found to be 0.65.
Overall, PCKQ-B in its present form is a 25 item tool with a moderate reliability or homogeneity.
Most frequent misconception
The two most commonly incorrectly answered questions were found to be ‘Use of placebos is appropriate in some types of pain’ and ‘Oxygen supplementation may help in last difficult breaths’ which was answered correctly only by 14% and 16% of the participants, respectively.
[Figure 3] depicts summary of development and validation of PCKQ-B. The final PCKQ-B, participant information sheet and the key to PCKQ-B are given as [Appendix 1-3] respectively.

- Development and validation of PCKQ-B. PCKQ-B: Palliative care knowledge questionnaire-basic, S-CVI: Scale content validity index, p: Item difficulty, d: Item discrimination, ICC: Intra class correlation, KR-20: Kuder-Richardson 20.
Demographic characteristics: (n = 99)
The participants came from all the six centres of Max Super Specialty Hospital across Delhi-NCR. Maximum participation was from institute in Vaishali, Ghaziabad, NCR (n = 34) and from South Delhi branch (n = 27) (there is a palliative care consultant in these 2 branches, hence more participation). Many of the participants did not respond to some of the items in demographic data [Table 1]. Nursing still being the female dominated profession, 79 (82.3%) out of 96 who answered the gender column were females. Mean age of the participants was 25.68 years, 64.4% of the participants were in the age group 21–25 years (n = 58, out of 90 who had filled the age column). All the nurses were RNs (Registered nurses with state nursing council having the qualification of BSc (Nursing) or GNM) as was the inclusion criterion for the study. About 14% also held a post graduate degree, but none in field of oncology. 34.4% (n = 33) nurses were working in oncology. This included chemotherapy day care, oncology OPD and wards. About 20.8% (n = 20) were critical care nurses and 39.6% (n = 38) were from other wards. About 90.6% (n = 87) of the study nurses were staff nurses, while 3.1% (n = 3) were nursing supervisors and 6.3% (n = 6) were nursing educators. 30.3 % (n = 27) had never cared for any cancer patient and 40.9 % (n = 36) had never cared for a terminally ill cancer patient. Education regarding palliative care in the institutes is so sparse that only 12 out of 99 nurses had participated in some educational activity related to palliative care. Seven out of them being in-hospital 1–2 h session on palliative care, one nurse had completed her Certificate Course in Essentials of Palliative Care from All India Institute of Medical Sciences Delhi, India; another was trained in ELNEC (End of Life Nursing Education Consortium) workshop and three others had attended 1–3 day workshops elsewhere. Hence, curriculum-based teaching was scarce in this sample of nurses. Two of the nurses had 1-year experience in palliative care each. Further details of the demographic profile are outlined in [Table 1].
| Characteristic | n | % | Missing data, n |
|---|---|---|---|
| Age (years) | |||
| 21–25 | 58 | 64.4 | 9 |
| 26–30 | 20 | 22.2 | |
| 30+ | 12 | 13.3 | |
| Total | 90 | 100.0 | |
| Gender | |||
| F | 79 | 82.3 | 3 |
| M | 17 | 17.7 | |
| Total | 96 | 100.0 | |
| Marital status | |||
| Single | 66 | 71.7 | 7 |
| Married | 26 | 28.3 | |
| Total | 92 | 100.0 | |
| Education | |||
| Bachelor’s degree | 88 | 85.8 | 1 |
| PG | 14 | 14.3 | |
| Total | 98 | 100.0 | |
| Job position | |||
| SN | 87 | 90.6 | 3 |
| Ed | 6 | 6.3 | |
| Sup | 3 | 3.1 | |
| Total | 96 | 100.0 | |
| Department of work | |||
| Ward | 38 | 39.6 | 3 |
| Oncology | 33 | 34.4% | |
| ICU | 20 | 20.8 | |
| Others | 5 | 5.2 | |
| Total | 96 | 100.0 | |
| Clinical experience (years) | |||
| 0 - Less than 2 | 45 | 52.9 | 14 |
| 2 - Less than 4 | 27 | 31.8 | |
| 4 and above | 13 | 15.3 | |
| Total | 85 | 100.0 | |
| Number of terminally ill patients ever cared for | |||
| None | 36 | 40.9 | 11 |
| 1–10 | 24 | 27.3 | |
| 10–50 | 14 | 15.9 | |
| 50 and above | 14 | 15.9 | |
| Total | 88 | 100.0 | |
| Number of cancer patients ever cared for | |||
| None | 27 | 30.3 | 10 |
| 1–10 | 22 | 24.7 | |
| 10–50 | 17 | 19.1 | |
| 50–100 | 9 | 10.1 | |
| >100 | 14 | 15.7 | |
| Total | 89 | 100.0 | |
F: Female, M: Male, PG: Post Graduate, Ed: nursing Educator, Sup: nursing Supervisor, SN: Staff Nurse, ICU: Intensive Care Unit, W: Ward
DISCUSSION
PCKQ-B is the first palliative care knowledge assessment tool for Indian nurses that has been tested extensively for its psychometric properties and is found to have a moderately satisfactory reliability and internal consistency.
The domains covered range from philosophy of palliative care to non-oncology palliative care. It covers the breadth of palliative care in terms of main symptoms like pain, breathlessness, myths surrounding morphine and colostomy care, in addition to embodying questions on resuscitation, communication, psycho-social needs and bereavement care. This broad coverage of scope of palliative care makes the questionnaire all the more unique when compared to already existing available validated tools (from other countries).[8,9,17]
Although non-oncology palliative care may not form a part of basic palliative care, questions were included with a thought that this would intrigue the nurses and initiate discussion about this topic. Moreover, being a self-administered tool, easy to use and analyse, with short answering time (average time 13.5 min), would add further to its usefulness.
PCKQ-B has an internal consistency KR-20 value of 0.65 which is moderately significant and similar to the estimated KR-20 value of PCQN-F (0.60).[27] While some of the very robust questionnaires including PCQN had KR-20 of 0.78,[8] PCKT had KR-20 value of 0.81[9] and Palliative care Emphasis program on symptom management and Assessment for Continuous medical Education – Questionnaire (PEACE-Q), was found to have KR-20 of 0.87.[28] Test-retest correlation for PCKQ-B was estimated as 0.52, which implies a fair correlation and was comparable to PCQN (0.56),[8] but less than PCKT (0.88)[9] and PEACE-Q (0.84).[28] Psychometric properties were compared to other palliative care knowledge/ attitude questionnaires like Spanish version of Palliative Care Quiz for Nurses (PCQN-SV),[26] Palliative Care Self-reported Practices Scale (PCPS)[28] and Palliative Care Difficulties Scale (PDCS) developed in Japan,[29] Palliative care attitude and knowledge (PCAK) questionnaire, by Al-Ansari et al., developed in Kuwait,[30] Undergraduate Nursing Palliative Care Knowledge Survey (UNPCKS), by Davis A et al. in USA in 2020.[31]
Comparison of other item analysis and reliability values is presented in [Table 2].
| Questionnaire (Reference) | p | d | KR-20 | Cronbach’s α | Test-Retest (ICC) | Known-Group | Factor Analysis |
|---|---|---|---|---|---|---|---|
| PCKQ-B | 0.1–0.9 | >0.2 | 0.65 | 0.52 | |||
| PCQN[8] | 0.2–0.8 | >0.5 | 0.78 | 0.56 | |||
| PCQN-F[27] | 0.2–0.8 | +ve | 0.6 | ||||
| PCQN-SV[26] | 0.55 (average) | >0.2(except 6 items) | 0.72 | 0.67* | |||
| PCKT[9] | IRT, −2.9–3.09 | IRT, 0.33–2.25 | 0.81 | 0.88 | P<0.001 in all domains | ||
| PCPS[29] | 0.8–0.91 each domain | ICC each domain 0.64–0.74 | P<0.05 in all domains | Exploratory factor analysis with promax rotation | |||
| PCDS[29] | 0.85–0.93 each domain | ICC each domain 0.61–0.69 | P<0.05 in all domains | Exploratory factor analysis with promax rotation | |||
| PEACE-Q[28] | IRT, −2.76– 0.29 | IRT, 0.69–2.67 | 0.87 | 0.84 | |||
| Home Palliative Care Knowledge Test (Shimizu et al.)[17] | IRT, −3.24– 1.05 | IRT, 0.56–3.06 | 0.87* | ||||
| PCS[10] | 0.27–0.99 | 0.81* | Exploratory factor analysis with varimax rotation | ||||
| K-PCCSI[11] | 0.90 | ||||||
| PCAK[30] | 0.636–0.824 | 0.95 | |||||
| UNPCKS[31] | 0.7 | Exploratory factor analysis |
Despite its apparent practical usefulness, PCKQ-B has certain limitations that deserve mentioning. The field testing was done on a small sample of nurses from a chain of tertiary care hospital, with major representation from east and south zones; hence, the results cannot be directly generalised to other government or smaller institutes. Known group validity could not be performed as we did not have an appropriately similar group of trained palliative care nurses. Use of open-ended questions might have added to the quality and probably quantity of information yielded. Although we did try to cover a wide range of aspects of palliative care, the present legal stance in India and ethical dilemmas (which are major barrier for palliative care interventions) have still been missing.
PCKQ-B would still prove to be a good starting point for any educational activity for nurses in palliative care (needs assessment), during implementation of an ongoing educational program to see if we get desired results over time and immediately after an educational activity (pre- and post-test) to find changes in knowledge.
As the government of India is now focussing on promoting palliative care at community level and primary health centres to improve coverage of rural population, another possible realm where its utility might be explored is knowledge needs assessment amongst community health workers (commonly known as ASHA workers in India), primary health workers, general physicians (non-specialist palliative care), social workers or physiotherapists working in palliative care teams. This might be useful even for the individuals as an objective tool to discover their own areas that need improvement. It could be translated it into regional languages to cater to different parts of India. Considering its advantages of short answering time and simplicity to administer, answer and evaluate, we believe that it will be feasible to be used in large cohorts too.
CONCLUSION
PCKQ-B definitely holds promise to fill the gap between teaching and assessments in Indian context. It is also expected to assist in developing more focused training programs and discussions. It would support palliative care physicians in corporate hospitals who constantly struggle with nursing care of their patients, by providing them with a direction to initiate nursing teaching programs in their hospitals. The nursing educators would be able to better assess educational needs of the nursing staff and the quality of nursing education provided. It is expected that regional versions of PCKQ-B could be used as a standardised tool all over India for educational evaluation, just like Japan uses PCKT[9,32] and Taiwan uses KAP PCCSI.[11,33,34] This would be a significant step towards overall improvement in palliative care provision in India and would bring significant changes in quality of life and quality of death of patients suffering with life-limiting and life-threatening diseases and their families.
Acknowledgment
We would like to acknowledge contribution of our experts Dr Naveen Salins, Dr Jeremy Johnson, Dr Savita Butola, Dr Shiv Pratap Rana, Dr. Sr. Vijaya Puthusseril, Dr. Sr Sandhya Gupta, Mrs. Aditi Prashant Sinha for their expert comments.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The Quality of Death: Ranking End-of-Life Care Across the World In: A Report Commissioned by the Lien Foundation. 2010.
- [Google Scholar]
- The 2015 Quality of Death Index: Ranking Palliative Care Across the World London: The Economist Intelligence Unit; 2015.
- [Google Scholar]
- End of life care policy for the dying: Consensus position statement of Indian association of palliative care. Indian J Palliat Care. 2014;20:171-81.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative care awareness among Indian undergraduate health care students: A needs-assessment study to determine incorporation of palliative care education in undergraduate medical, nursing and allied health education. Indian J Palliat Care. 2010;16:154-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of 'palliative care information booklet' in enhancing nurses' knowledge. Indian J Palliat Care. 2010;16:164-7.
- [CrossRef] [PubMed] [Google Scholar]
- End-of-life care policy: An integrated care plan for the dying. Indian J Crit Care Med. 2014;18:615-35.
- [CrossRef] [PubMed] [Google Scholar]
- The palliative care quiz for nursing (PCQN): The development of an instrument to measure nurses' knowledge of palliative care. J Adv Nurs. 1996;23:126-37.
- [CrossRef] [PubMed] [Google Scholar]
- The palliative care knowledge test: Reliability and validity of an instrument to measure palliative care knowledge among health professionals. Palliat Med. 2009;23:754-66.
- [CrossRef] [PubMed] [Google Scholar]
- A measure of palliative care in nursing homes. J Pain Symptom Manage. 2011;41:57-67.
- [CrossRef] [PubMed] [Google Scholar]
- Path modeling of knowledge, attitude and practice toward palliative care consultation service among Taiwanese nursing staff: A cross-sectional study. BMC Palliat Care. 2017;16:42.
- [CrossRef] [PubMed] [Google Scholar]
- Enhancing the autonomy of Indian nurses. Indian J Med Ethics. 2017;2:275-81.
- [CrossRef] [PubMed] [Google Scholar]
- Attitudes of nurses towards care of the dying patient in India. Int J Palliat Nurs. 2017;23:558-66.
- [CrossRef] [PubMed] [Google Scholar]
- Maria Cecilia Sepulveda Bermedo. Global Atlas of Palliative Care at the End of Life. In: World Palliative Care Alliance. Geneva: World Health Organization; 2014.
- [Google Scholar]
- Questions to Assist with the Critical Appraisal of Cross-Sectional Studies. 2018. Available from: http://www.cardiff.ac.uk/insrv/libraries/sure/checklists.htm. [Last accessed on 2021 Sep 20]
- [Google Scholar]
- Development and validation of the quality care questionnaire-palliative care (QCQ-PC): Patient-reported assessment of quality of palliative care. BMC Palliat Care. 2018;17:40.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of scales for attitudes, self-reported practices, difficulties and knowledge among home care nurses providing palliative care. Eur J Oncol Nurs. 2016;22:8-22.
- [CrossRef] [PubMed] [Google Scholar]
- A study on knowledge, attitude, and practices regarding palliative care among doctors in border security force. Prog Palliat Care. 2014;22:272-9.
- [CrossRef] [Google Scholar]
- The content validity index: Are you sure you know what's being reported? Critique and recommendations. Res Nurs Health. 2006;29:489-97.
- [CrossRef] [PubMed] [Google Scholar]
- Determination and Quantification of Content Validity. Nurs Res. 1986;35:382-5.
- [CrossRef] [PubMed] [Google Scholar]
- Content validity ratio In: Frey BB, ed. The SAGE Encyclopedia of Educational Research, Measurement, and Evaluation. Thousand Oaks: SAGE Publications; 2018. p. :397-8.
- [Google Scholar]
- Item analysis In: Frey BB, ed. The SAGE Encyclopedia of Educational Research, Measurement, and Evaluation. Thousand Oaks: SAGE Publications; 2018. p. :887-91.
- [Google Scholar]
- Item discrimination indices. Rasch Meas Trans. 2002;16:883-4. Available from: https://www.rasch.org/rmt/rmt163a.htm. [Last accessed on 2021 Sep 20]
- [Google Scholar]
- Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6:284-90.
- [CrossRef] [Google Scholar]
- KR-20 In: Frey BB, ed. The SAGE Encyclopedia of Educational Research, Measurement, and Evaluation. Thousand Oaks: SAGE Publications; 2018. p. :933-6.
- [Google Scholar]
- An instrument to measure nurses' knowledge in palliative care: Validation of the Spanish version of palliative care quiz for nurses. PLoS One. 2017;12:e0177000.
- [CrossRef] [PubMed] [Google Scholar]
- The French version of the palliative care quiz for nursing (PCQN-F): Development and evaluation. J Palliat Care. 2005;21:27-34.
- [CrossRef] [PubMed] [Google Scholar]
- The palliative care knowledge questionnaire for PEACE: Reliability and validity of an instrument to measure palliative care knowledge among physicians. J Palliat Med. 2013;16:1423-8.
- [CrossRef] [PubMed] [Google Scholar]
- The palliative care self-reported practices scale and the palliative care difficulties scale: Reliability and validity of two scales evaluating self-reported practices and difficulties experienced in palliative care by health professionals. J Palliat Med. 2010;13:427-37.
- [CrossRef] [PubMed] [Google Scholar]
- Development of palliative care attitude and knowledge (PCAK) questionnaire for physicians in Kuwait. BMC Palliat Care. 2019;18:49.
- [CrossRef] [PubMed] [Google Scholar]
- Development of a new undergraduate palliative care knowledge measure. J Prof Nurs. 2020;36:47-52.
- [CrossRef] [PubMed] [Google Scholar]
- A Japanese region-wide survey of the knowledge, difficulties and self-reported palliative care practices among nurses. Jpn J Clin Oncol. 2014;44:718-28.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term effectiveness of two educational methods on knowledge, attitude, and practice toward palliative care consultation services among nursing staff: A longitudinal follow-up study. Clin Nurs Res. 2018;27:483-96.
- [CrossRef] [PubMed] [Google Scholar]
- Associations among knowledge, attitudes, and practices toward palliative care consultation service in healthcare staffs: A cross-sectional study. PLoS One. 2019;14:e0223754.
- [CrossRef] [PubMed] [Google Scholar]
Appendix 1:
Palliative Care Knowledge Questionnaire -Basic (PCKQ-B).
| Palliative Care Knowledge Questionnaire-Basic (PCKQ-B) | ||||
|---|---|---|---|---|
| Yes | No | Don’t know | ||
| 1. Taking care of caregiver is equally important as patient’s care. | ||||
| When do you think palliative care is needed? | ||||
| 2. Care of patients with advanced cancer | ||||
| 3. Total care of chronically ill patients | ||||
| 4. HIV/AIDS patients | ||||
| 5. Chronic non-malignant diseases such as end-stage heart failure | ||||
| 6. Palliative care should start at the time of diagnosis of a life-threatening illness | ||||
| Pain in palliative care: | ||||
| 7. Is pain a vital sign? | ||||
| 8. Severity of pain determines method of pain treatment. | ||||
| 9. Most effective drug for cancer pain is fortwin+phenargan. | ||||
| 10. Use of placebos is appropriate in some types of pain. | ||||
| 11. A patient on morphine does not need NSAIDs (e.g. diclofenac)/ paracetamol. | ||||
| Morphine in palliative care: | ||||
| 12. Causes addiction in terminally ill patients | ||||
| 13. Causes death in all dying patients | ||||
| 14. Always causes nausea/vomiting | ||||
| 15. Patient with lung metastasis having breathlessness must be intubated (in palliative care) | ||||
| 16. Are you aware of problems and practical care of patient with colostomy? | ||||
| 17. Oxygen supplementation may help in last difficult breaths. | ||||
| Communication of prognosis: | ||||
| 18. Prognosis should always be clearly communicated | ||||
| 19. Prognosis should only be informed to family members | ||||
| Resuscitation in cancer patients: | ||||
| 20. Resuscitation must always be performed if a patient is crashing irrespective of advanced metastatic cancer. | ||||
| 21. Patients (if possible) and relatives both should always be involved in ‘Do Not Attempt Resuscitation (DNAR/DNR)’ decision making. | ||||
| Psycho-socio-spiritual issues: | ||||
| 22. Role of nurses is to take care of physical aspect of disease only, psychological issues must be dealt by psychiatrist or other professionals. | ||||
| 23. Role of nurses is to take care of physical aspect of disease only, social issues must be dealt by social worker or other professionals. | ||||
| Bereavement care: | ||||
| 24. Do you know what bereavement is? | ||||
| 25. Are you aware of concept of bereavement care? | ||||
PCKQ-B: Palliative Care Knowledge Questionnaire -Basic
| Demographic Data |
|---|
| Age |
| Gender : Male Female Others |
| Marital status Single/married/other |
| Education B. Sc. GNM Post-graduation Other |
| Clinical experience (after graduation) |
| Place of work |
| Job position |
| Department of work |
| Duration of working in the institution |
| Any experience in palliative care |
| Number of terminally ill cancer patients ever cared for |
| None 1 to 10 10 to 50 50 to 100 ˃100 |
| Number of cancer patients ever cared for |
| None 1 to 10 10 to 50 50 to 100 ˃100 |
| Participation in educational activities related to palliative care. Yes/No. If Yes, name and duration of course/CME: |
| Is there a palliative care physician in your institute? |
Appendix 2:
Participant Information Sheet
Participant Information Sheet
Instructions to fill the questionnaire:
There are a total of 25 questions in the questionnaire. All the questions need to be answered as Yes/No/ Don’t know. Kindly respond to the best of your knowledge. The option of ‘Don’t know’ is provided in case you are not sure for the response. Definitions/meanings of terms used in questionnaire:
‘Terminally ill’ patient is defined as the one suffering from an irreversible or incurable disease condition from which death is expected in the foreseeable future. ‘Dying care:’ care provided during the hours or days preceding imminent death during which time the patient’s physiological functions wane. Placebo: A substance containing no medication and prescribed to reinforce a patient’s expectation to get well. For e.g. normal saline given as a painkiller to a patient who is continuously complaining of pain. When used for needs assessment: The questionnaire is anonymous and your identity will not be revealed at any point during the study. This is not an assessment and you will not be marked for the same. It is a needs assessment study, so participants should be as true to their present knowledge as possible so that we can come out with better and more reliable results. You may ask for any clarification for any question from one of the team members. It will be used to create a modified learning module that will be more appropriate to your needs. It will also help us to know your strengths so that we can utilise them in more appropriate way for benefit of our patients. The confidentiality of records will be maintained throughout the study. The records will be accessible only to authorised persons involved in the study. You are free to participate or to withdraw from research at any time without penalty or loss of benefits to which you are otherwise entitled.
Appendix 3:
Palliative Care Knowledge Questionnaire-Basic (PCKQ-B) key
1. Taking care of caregiver is equally important as patient’s care.-------------YES
According to WHO definition of Palliative Care Palliative care is ‘an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.’
When do you think palliative care is needed?
2. Care of patients with advanced cancer------------------------------------------YES
3. Total care of chronically ill patients-----------------------------------------------YES
4. HIV/AIDS patients----------------------------------------------------------------------YES
5. Chronic nonmalignant diseases like end stage heart failure-----------------YES
6. Palliative care should start at the time of diagnosis of a life-threatening illness.--YES
According to the WHO definition of Palliative Care Palliative care is needed for all life-threatening illness including cancer, end stage renal, liver or heart failure, senility, HIV/AIDS patients and it works by prevention and relief of suffering, hence palliative care should start at the time of diagnosis.
Pain in palliative care:
7. Is pain a vital sign? ----------------------------------------------------------------------YES
The idea of evaluating Pain as a vital sign was first presented by Dr. James Campbell in his 1995 Presidential Address to the American Pain Society and the idea was rapidly adopted by Joint Commission on Accreditation of Healthcare Organisations (JCAHO, now The Joint Commission(JCAHO Standard PE1.4, 2000)) and since then Pain is considered as the 5th vital sign.
8. Severity of pain determines method of pain treatment. -----------------------------YES
According to WHO Analgesic Ladder ‘Analgesics must be prescribed according to pain intensity as evaluated by a scale of pain severity.’
It is not the extent of disease that determines the method of treatment, for e.g. even if a patient with localised disease has severe pain, he or she may need step 3 analgesics while a patient with extensive metastatic disease might be well settled with step 1 analgesics. Now, we are moving towards ‘Mechanism based management of pain,’ rather than solely depending on intensity or severity of pain.
9. Most effective drug for cancer pain is fortwin+phenargan. -----------------------------NO
Fortwin +phenargan (Pentazocine + Promethazine), a combination of opioid analgesic and antihistaminic has been used extensively for severe pain in acute setting like gynaecology and other wards as it gives some pain relief and puts the patient to sleep, however, it is not an effective way of managing cancer pain due to short duration of action and side effects like dysphoria.
10. Use of placebos is appropriate in some types of pain. -----------------------------NO
Practically (especially in palliative care) there is no role of placebos in any type of pain. However, there are psychological and neurological theories of placebo effects that are being studied and applied in trials related to chronic pain.
11. A patient on morphine does not need NSAIDs (e.g. diclofenac)/paracetamol. -------NO
Cancer pain is best managed based on severity and mechanism of pain with Morphine being the gold standard opioid analgesic for severe cancer pain along with other step 1 analgesics like acetaminophen or NSAIDs (if not contraindicated or considered high risk) and adjuvant analgesics like anti-neuropathic agents.
Step 1 analgesics must continue with strong opioids in view of their supplementary analgesic action and opioid sparing effect.
Morphine in palliative care:
12. Causes addiction in terminally ill patients------------------------------------------------NO
For all practical purposes in a patient with advanced cancer, with appropriate use of morphine or any strong opioid the possibility of any addiction is remote.
13. Causes death in all dying patients------------------------------------------------NO
Morphine does not disturb function of any vital organ to cause premature death. It is absolutely safe and effective when used appropriately, monitored and reviewed by an expert regularly. However, the same medication can have serious side effects if given without due caution.
14. Always causes nausea/vomiting------------------------------------------------NO
When started on morphine or any strong opioid, 1/3rd of the patients complain of nausea or vomiting and hence we always prescribed a round the clock dose of prokinetic (like domperidone or metoclopramide) for 3 -4 days and then PRN basis.
15. Patient with lung metastasis having breathlessness must be intubated (in palliative care) ----------------------------------------------------------------------------------NO
Intubation of trachea and artificial ventilation are temporary measures to sustain breathing while the underlying pathology is being taken care of (for example with antibiotics for infection), however, if the underlying pathology is not curable, artificial ventilation may not help the patient and rather increase the suffering. In such cases, it would be better to manage breathlessness conservatively with medications and non-pharmacological techniques than intubation. However, the treatment plan may need to be individualized depending on the condition of the patient.
16. Are you aware of problems and practical care of patient with colostomy?------ YES
This is a Yes/No question to be answered if the participant is aware or not aware.
17. Oxygen supplementation may help in last difficult breaths.--------------NO
Oxygen may not help in last difficult breaths, unless patient is hypoxic. Despite optimal medical management, patient may experience last difficult breaths. Use of air (hand held fan or table fan) is equivalent to oxygen in such cases. Communication of prognosis:
18. Prognosis should always be clearly communicated.--------------------------YES
Yes, Prognosis should always be clearly communicated in an empathetic and compassionate way.
19. Prognosis should only be informed to family members.--------------------NO
It is patient’s right to know his disease and prognosis so as to make appropriate choices for his/her treatment and life. However, if where the family members do not want the prognosis to be told to patient, such cases should be handled carefully and sensitively with the help of an expert.
Resuscitation in cancer patients:
20. Resuscitation must always be performed if a patient is crashing irrespective of advanced metastatic cancer.--------------------------------------------------NO
Resuscitation or CPR is a temporary measure to sustain circulation or breathing to buy time to manage the underlying pathology (for example in case of acute myocardial infarction or ventricular fibrillation), however, if the underlying pathology is not curable, resuscitation may not help the patient and rather increase the suffering. In such cases, it would be better to forego any form of resuscitation in an event of cardiac or respiratory arrest.
21. Patients (if possible) and relatives both should always be involved in ‘Do Not Attempt Resuscitation (DNAR/DNR)’ decision making.------------------------------YES
Yes, DNAR is always a shared decision making with the patient (whenever patient is in a condition to take decision), close relatives and a team of doctors. Psycho-socio-spiritual issues:
22. Role of nurses is to take care of physical aspect of disease only, psychological issues must be dealt by psychiatrist or other professionals.----------------------------NO
Nurses play a crucial role in management of psychological issues as they spend maximum time with the patient and patients tend to share their stories with them more openly. They may engage in conversations while changing the fluids or providing them with medications. The gentle touch and compassionately providing comfortable position may help them ease their psychological distress. However, to manage complex psychological issues, psychiatrist or other professionals may be involved.
23. Role of nurses is to take care of physical aspect of disease only, social issues must be dealt by social worker or other professionals.------------------------------------NO
Nurses play a crucial role in management of social issues as they spend maximum time with the patient and patients tend to share their stories with them more openly. They may engage in conversations while changing the fluids or providing them with medications. However, to manage complex social issues, social worker or other professionals may be involved.
Bereavement care:
24. Do you know what bereavement is?------------------------------------------YES
This is a Yes/No question to be answered if the participant is aware or not aware.
25. Are you aware of concept of bereavement care?-------------------------YES
This is a Yes/No question to be answered if the participant is aware or not aware.






