Translate this page into:
To Study the Barriers in Palliative Care to Nonmalignant Cases in COVID-19 Crisis in a Tertiary Health-Care Center
Address for correspondence: Dr. Roopesh Jain, DK-5/105, Danish Kunj Colony, Kolar Road, Bhopal - 462 042, Madhya Pradesh, India. E-mail: drroopeshjain@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
COVID-19, the new pandemic faced by the world, is a novel betacoronavirus causing severe respiratory coronavirus syndrome. Elderly patients, people with underlying chronic illnesses, cancer patients, and those who are immunocompromised are at higher risk and account for higher mortality rate. Unfortunately, there is no approved medication for treatment, till date, thereby supporting triage management and difficult decision-making. Thus, there should be a substantial increase in the palliative care in times of pandemic. There should be an increase in the availability of palliative care services in different care settings. Due to a surge in the number of cases of COVID-19, it has been reported on how palliative care is being delayed, discontinued, or deprioritized.
Aim:
The aim of this study is to evaluate the barriers occurring in providing the palliative care to the patients with nonmalignant illness.
Methodology:
A questionnaire was designed after studying previous work over palliative care and pandemic crisis and was distributed among the physicians, surgeons, and the residents; a total of 95 health-care workers were involved. The survey was done through mails. The response then was evaluated and analyzed.
Results:
As seen by the responses we got from the health-care workers, the main issue is the nonavailability of the personal protective equipment during this pandemic. Keeping the current scenario in mind, regarding COVID-19, the patients are at fear of coming to the hospital at first place, and even if they come then the fear of being alone haunts them. One of the biggest fears of the patient is dying alone, without being in contact with their loved ones.
Conclusion:
Palliative care should be an essential part of any health-care service in any humanitarian crisis, including the COVID-19 pandemic. Thus, effort should be made to remove the barriers and provide palliative care to the patient.
Keywords
Barriers
COVID-19
health-care professionals
pandemic
INTRODUCTION
COVID-19, the new pandemic faced by the world, is a novel betacoronavirus causing severe respiratory coronavirus syndrome, emerged in Wuhan, China, in December 2019. On March 11, 2020, COVID-19 was declared as a pandemic by the World Health Organization (WHO). The global mortality has been estimated to be 3.4% by the WHO.[1] Elderly patients, people with underlying chronic illnesses, cancer patients, and those who are immunocompromised are at higher risk and account for higher mortality rate.[2] Unfortunately, there is no approved medication for treatment, till date.
Palliative care is supportive care for terminally ill and for those patients which do not have curative treatment such as those of cancer, liver and kidney failure, decompensated liver disease, neurodegenerative brain and spine diseases, heart diseases, and decompensated heart diseases. It is considered to be an essential component of health care among nonmalignant cases in the pandemic, providing psychological, physical, emotional, spiritual support to the patient, relatives, and health-care professionals, thereby supporting triage management and difficult decision-making.
Thus, there should be a substantial increase in the palliative care in times of pandemic. There should be an increase in the availability of palliative care services in different care settings as in the intensive care units (ICUs), hospital wards, emergency departments, and in settings where we consider higher risk patients to be residing. The core of palliative care is considered to be the shared decision-making between the clinicians and the patients, regarding the process of end of life. However, during the pandemic this decision regarding the prolongation of life decision or location of death has been severely restricted due to public health directives as well as due to limited resources. Furthermore, due to visitor and travel restrictions, the patients could face isolation during this pandemic. Furthermore, due to increase workload on the health-care professionals, they are unable to spend time at the bedside or physically examine the patient regularly, which could have a negative effect on the care of the patient.[34]
Due to a surge in the number of cases of COVID-19, it has been reported on how palliative care is being delayed, discontinued, or deprioritized. The causes which could be interpreted for disruption are concern about patients' susceptibility to the serious risk of COVID-19 infection, understaffed due to the redeployment of the health-care workers, bed and equipment to the COVID-19 wards or ICU, and undersupplied with medications. Thus, there is an urgent need for palliative care to be continued.
This single-center study highlights the possible barriers occurring in providing the palliative care in the COVID-19 era in our hospital.
METHODOLOGY
This study was conducted at L. N. Medical College, Bhopal, after taking approval from the Institutional Research Committee. A questionnaire was developed by reviewing the previous studies. A mail-based survey was done where this questionnaire was distributed to the physicians and the surgeons including the residents of our hospital. Those who gave consent and were working in the hospital with terminally ill patients were included in the study. The received answers were analyzed.
RESULTS
A total of 95 health-care professionals participated in the study. The study was done over the period of March 15, 2020–May 15, 2020. During this time, patient load of around 18 in number had been reported [Tables 1 and 2].
| Characteristic | Number (percentage of total) |
|---|---|
| Gender | |
| Male | 71 (75) |
| Female | 24 (25) |
| Post | |
| Consultant | 43 (45) |
| Resident doctor | 52 (55) |
| Specialization | |
| Anesthesia/critical care | 25 (26) |
| Medicine | 35 (37) |
| Surgery | 35 (37) |
| Age | |
| 26-35 | 43 (45) |
| 36-45 | 15 (15) |
| 46-55 | 19 (20) |
| 56-65 | 09 (10) |
| >65 | 09 (10) |
| Years of experience | |
| <1-4 | 43 (45) |
| 5-10 | 19 (20) |
| 11-20 | 19 (20) |
| >20 | 15 (15) |
| Current percentage clinical time | |
| 5-19 | 24 (25) |
| 20-49 | 37 (40) |
| 50-75 | 19 (20) |
| >75 | 15 (15) |
| Number (percentage of total) | |
|---|---|
| Do you know about palliative care? | |
| Yes | 70 (74) |
| No | 25 (26) |
| Do you know about COVID-19 pandemic? | |
| Yes | 95 (100) |
| No | 0 |
| Are you in contact with the terminally ill patients? | |
| Yes | 66 (70) |
| No | 29 (30) |
| Do you consider each and every patient coming to the hospital to be a suspect of COVID-19? | |
| Yes | 90 (95) |
| No | 5 (5) |
| Are you aware of the latest guidelines regarding palliative care in COVID-19 pandemic? | |
| Yes | 54 (57) |
| No | 41 (43) |
| According to you is the most appropriate use of PPE? | |
| According to guidelines given | 60 (63) |
| According to the ward you are working | 20 (21) |
| You decide yourself | 5 (5) |
| According to the availability | 10 (11) |
| Do you consider availability of PPE is the major concern for reduced palliative care? | |
| NO, nonavailability is not the issue | 12 (13) |
| YES, nonavailability is what draws me back | 45 (47) |
| Depend on the patient condition | 15 (16) |
| Can work with limited resources | 23 (24) |
| Do you think palliative care is important during this pandemic? | |
| Yes, it is the right of the patient | 63 (66) |
| Maybe, according to the condition of the patient | 20 (21) |
| No, it is risk for the health-care professional | 12 (13) |
| Does the fear of patient being immunocompromised restrict your actions? | |
| No, with the use of PPE, no harm can be done | 54 (57) |
| No, with limited resources also no fear is there | 5 (5) |
| Yes, with the use of PPE, the harm can be decreased only | 16 (17) |
| Yes, limited resources are the cause of restriction | 20 (21) |
| From the patients’ point of view, what can be the barrier in providing palliative care? | |
| Fear of being alone in the hospital | 21 (22) |
| Fear of getting infected by health-care professionals | 15 (16) |
| Patient not ready to come to the hospital | 10 (11) |
| Fear of dying alone | 49 (51) |
| From the relatives’ point of view, what can be the barrier in providing palliative care? | |
| Fear of getting infected by the patient himself | 20 (21) |
| Fear of getting infected by the doctors | 45 (47) |
| Relatives not ready to bring patient to the hospital | 7 (8 ) |
| Fear of losing the loved one alone | 23 (24) |
| Due to health ministry directives, any change occurs in palliative care? | |
| Patient being left alone | 5 (5) |
| Not able to contact the relatives | 3 (3) |
| Decision-making is all based on health-care professionals | 20 (21) |
| All of the options | 67 (71) |
| Is the decision-making process now difficult? | |
| Yes, it does not involve view of the patient | 20 (21) |
| Yes, it does not involve view of the relatives | 28 (29) |
| Relatives consider your decision to be irrational | 42 (45) |
| No, decision-making is being easier | 5 (5) |
| Do you want to change the visiting policies? | |
| No, it should be according to the guidelines | 70 (73) |
| Yes, relax the policy when patients are dying | 5 (5) |
| Allow relative to stay within the area but not return once left | 10 (11) |
| Completely closed to the visitors | 10 (11) |
| What are the admission criteria for your hospital? | |
| Telephone triage system before admission | 59 (62) |
| Open to any patient who so ever comes | 14 (15) |
| Open to COVID-negative patients only | 1 (1) |
| Decreased number of admission by proper counseling | 21 (22) |
| What is the impact of pandemic on the workforce? | |
| Nursing staff is in fear | 5 (5) |
| Doctors are in fear | 7 (7) |
| Overburdened due to work | 8 (9) |
| All the options | 75 (79) |
| What do you think is the most common barrier for not providing palliative care? | |
| Nonavailability of PPE | 68 (73) |
| Fear of getting infected by the patient | 9 (9) |
| Lack of knowledge about palliative care | 9 (9) |
| Fear of taking individual decision for the patient | 9 (9) |
COVID: Coronavirus disease, PPE: Personal protective equipment
According to the various responses given by the residents and the consultants, we plotted the graphs separately in order to evaluate the different barriers [Figures 1-4].

- It shows the number of consultant and residents choosing an option regarding use of PPE
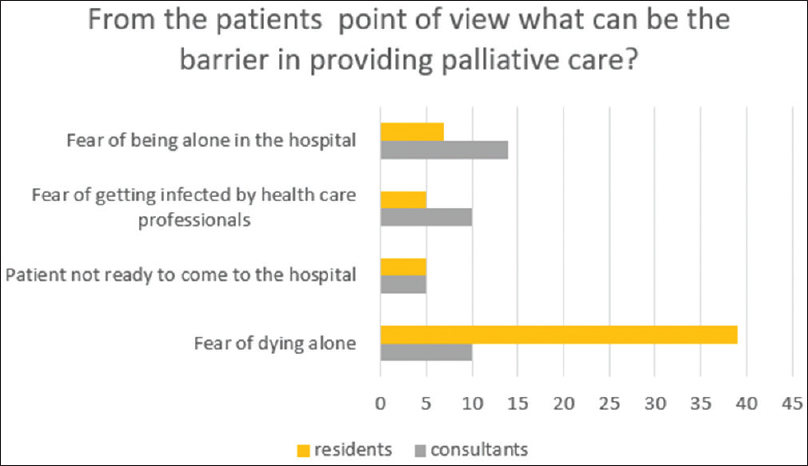
- It's shows the number of consultant and resident choosing an option regarding barriers

- It's shows the number of consultant and resident choosing an option regarding ministry directions and changes in care
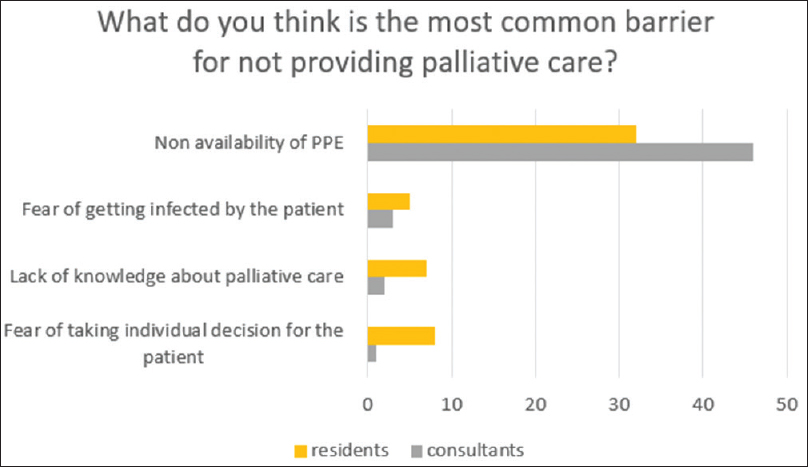
- It shows the number of consultant and resident choosing an option regarding most common barrier
Thus, according to the result, barriers can be divided into three main categories.
With respect to the health-care worker
As seen by the responses we got from the health-care workers, the main issue is the nonavailability of the personal protective equipment (PPE) during this pandemic. Among many residents, it is a big barrier for not providing palliative care to the patient. Furthermore, fear of getting infected by the patient is a big fear among the doctors. Palliative care is not an easy job to do. It involves breaking the bad news to the family as well as to the patient.
Due to social distancing norms, there are many obstacles in a way that the relatives cannot be presented with the patient during their last moments. Due to these things, few doctors have fear of upsetting patients, thereby referring the patients to other doctors or higher centers. Furthermore, few of them do not know the resource availability as well as use of them for the patients.
With respect to the patients
According to the studies done before, there are five major points which a patient identifies as major theme of palliative care:
-
To receive adequate pain and symptom management Medications
-
Avoid inappropriate prolongation of the death
-
Have a sense of control over the decision made for himself/herself
-
Relieving the burden of the disease
-
Strengthening relationship with the loved ones.
Keeping the current scenario in mind, regarding COVID-19, the patients are at fear of coming to the hospital at first place, and even if they come then the fear of being alone haunts them. The decisions of further management are being taken by the doctors only keeping in mind the state of the patient, which increase their anxiety levels. One of the biggest fears of the patient is dying alone, without being in contact with their loved ones.
With respect to the relatives
Losing their loved ones is a big loss for any person, and not being in touch with them during their last moments is the biggest fear. Increased awareness about the pandemic has made everyone cautious about the infection, making people believe in everything they hear or see, for which directly or indirectly people avoid their loved ones to bring to the hospital. Furthermore, people are worried of the infection being transferred from the health-care workers to themselves as well as to the patient, thereby decreasing the number of patients being brought to the hospital these days.
DISCUSSION
The study conducted is a pilot study. There are many ongoing studies where the data will be different as the number of cases increasing, increasing the incidence and the prevalence of the disease, causing difference in the result of the study.
The data provided by the study performed show that the most common barrier occurring among the health-care workers in the tertiary health-care center in providing the palliative care to nonmalignant patient is the fear of getting infected due to the lack of availability of PPE. An important concern voiced by the doctors is the lack of preparedness for COVID-19.
Palliative care plays an important role in COVID-19 not only in the cancer patients but also among the noncancer illness patients. Many policies and guidelines are being made for the cancer patient; there is now need for guidelines for nonmalignant illness to be considered for palliative care during this pandemic. It provides support with complex decisions and triage of the patients, providing psychological support to the patient as well as family. It has been shown that the patient receiving the palliative care has improved the quality of life during the last days rather than prolonging the duration of suffering, thereby reducing the chances of depression among the patients, also patient feels more in control. However, as death is often sudden and unpredictable[56] in these patients, palliative care should be provided to this group.
With respect to the nonmalignant illnesses, the major barrier is the lack of definition of the terminal illness which needs palliative care and is nonmalignant.
Therefore, essential elements to be remembered while implementing a palliative care plan during this pandemic include:
-
Provide health-care workers with proper PPE, medication kits, and equipment needed for the patients
-
Provide knowledge to the staff, health-care professionals on symptom management, forming standard sheets and protocols, and involving caretakers in providing psychological and bereavement support
-
Identification of the wards and beds appropriate for the patients going to die
-
System to identify the patients in need of palliative care and provide them with appropriate support.[7]
CONCLUSION
Palliative care should be an essential part of any health-care service in any humanitarian crisis, including the COVID-19 pandemic. A physician's desire to cure his/her patient is often seen with frustration over futility, and patients' desire to live is often balanced with the concern for comfort. These differences in the ideas could create tension among the health-care professionals, patients, and the relatives. These tensions could be relieved by providing early access to the palliative care.
The government must urgently recognize the role of palliative care among the nonmalignant cases during the COVID-19 pandemic and ensure that this is protected and integrated in the health-care system as soon as possible so that all the patients can be in benefit.
Thus, patients who are not expected to survive must receive palliative care as a human right.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;325:1435-40. doi: 101001/jama 20203972
- [Google Scholar]
- China novel coronavirus investigating and research team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727-33.
- [Google Scholar]
- Impact of physician sitting versus standing during inpatient oncology consultations: Patients' preference and perception of compassion and duration. A randomized controlled trial. J Pain Symptom Manage. 2005;29:489-97.
- [Google Scholar]
- Cancer patients' perceptions regarding the value of the physical examination: A survey study. Cancer. 2014;120:2215-21.
- [Google Scholar]
- Differences in health care utilization at the end of life among patients with chronic obstructive pulmonary disease and patients with lung cancer. Arch Intern Med. 2006;166:326-31.
- [Google Scholar]
- Palliative care and cardiovascular disease and stroke: A policy statement from the American Heart Association/American Stroke Association. Circulation. 2016;134:e198-225.
- [Google Scholar]
- Palliating a pandemic: All patients must be cared for. J Pain Symptom Manage. 2010;39:291-5.
- [Google Scholar]






