Translate this page into:
Topical Menthol for Treatment of Chemotherapy-induced Peripheral Neuropathy
Address for correspondence: Dr. Alessio Cortellini, Medical Oncology Unit, St. Salvatore Hospital, University of L’Aquila, ASL1 Abruzzo, Via Vetoio, 67100 L’Aquila, Italy. E-mail: alessiocortellini@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Chemotherapy-induced peripheral neuropathy is a frequent treatment-limiting factor that significantly impairs patients’ everyday life, also because of a lack of valid palliative options. Here, we report a case of a male patient with a history of metastatic colon cancer and previous chemotherapies. He came to our attention with a peripheral neuropathy that impaired his quality of life and could limit the further line of chemotherapy. We treated the neuropathy with menthol aqueous cream with benefit.
Keywords
Cancer
chemotherapy
menthol
neuropathic pain
TRPM8
INTRODUCTION
Chemotherapy-induced peripheral neuropathy (CIPN) is one of the most frequent adverse events for anticancer treatments, including both cytotoxic and biological agents; CIPN is often underestimated by clinicians, even though it frequently becomes a dose-limiting toxicity, because of the significant worsening in patients’ quality of life. The incidence is variable, and it can be estimated that from 30% to 40% of chemotherapy-treated patients experienced CIPN.[1] Despite the relevance of the problem, treatment options are limited and often unsuccessful; the most used ones are oral anticonvulsants and antidepressants, which require long-term intake, with relevant side effects.[2] It has been shown that molecular receptors for cooling are upregulated in neuropathic pain models;[34] one of these is the transient receptor potential melastatin 8 (TRPM8), a cation channel that is present on central and peripheral terminals of primary sensory neurons. After the demonstration that the activation of TRPM8 can reverse the sensitization of behavioral reflexes elicited by peripheral nerve injury in animal models,[5] some clinical experiences with topical activators of TRPM8, such as menthol based creams in various concentration, have marked a potential new approach in the therapy for CIPN.[678] In our institute, we noticed that the most limiting factor reported is the interference in activities of daily living, which can impair mood and compliance of patients, who do not want to “add to the list” another drug to treat a side effect, especially without a perceived benefit.
CASE REPORT
We report a case of a male patient, previously treated at another institute, with a history of stage IV colon adenocarcinoma and two previous chemotherapy treatments. After the radical left hemicolectomy, he received 8 cycles of adjuvant chemotherapy with oxaliplatin and capecitabine at standard doses, developing a long-lasting painful drug-induced peripheral neuropathy. The disease-free survival was 21 months, due to relapse to lungs, lymph nodes, and peritoneum, so he received a first-line chemotherapy with FOLFIRI and bevacizumab at standard doses, with partial response after 3 and 6 cycles and progressive disease after 9 cycles. He came to our attention at the age of 58 years, in need of a second-line chemotherapy, showing good clinical conditions, no comorbidities, and Eastern Cooperative Oncology Group Performance Status 0;[9] the only disabling symptom reported was the CIPN G2 (NCI CTCAE version 4.0), particularly to the extremities, previously treated with pregabalin without benefit. We decided to start a second-line chemotherapy with 5-Fluorouracil (5FU), bevacizumab, and oxaliplatin, scheduled as follows: 5-FU 900 mg/m2 for four nights timed flat infusion of 12 h,[101112] every 2 weeks, bevacizumab 5 mg/kg every 2 weeks, oxaliplatin 70 ng/m2 every 2 weeks, in 28 days cycles. In order to classify, monitor, and prevent the worsening of the neuropathy, we planned an assessment at the baseline and at every cycle during the treatment, while topical 1% menthol in aqueous cream (galenic preparation) was applied to the areas of sensory disturbance (extremities) twice a day; given the subjectivity of CIPN, the evaluations were not performed with instrumental measurements, but using a 0–10 numeric pain rating scale (NRS),[13] the neuropathic pain symptom inventory (NPSI),[14] and the Italian version of the Brief Pain Inventory (i-BPI).[15] During the first 4 months of chemotherapy, the NRS score for the neuropathy was 6 at cycle one, 5 at cycle two, 4 at cycles three and four, and 3 at cycle five. In the NPSI, the most relevant answers were number 4 and 12, which characterized the pain as a continuous tingling; while the duration of the pain remained the same through the 24 h of the day, the scores that defined the tingling were 8 at cycle one, 7 at cycle two, 4 at cycle three, 8 at cycle four, and 5 at cycle five. The most interesting data come from the i-BPI, where we observed no significant scores in answers 3, 4, 5, and 7, which defined the severity and intensity of the pain (every answer was less than or equal at 3 out of 10), while we noted relevant scores in answer 9, that describes how much the pain interferes with several everyday-life activities and with mood. [Figure 1] shows changes in the scores at the answer 9 during the cycles; notably at the second and the third assessment, we can observe meaningful improvements in all the parameters, and while at the fourth evaluation, there is a worsening trend. In that period, the patient had the planned computed tomography scan, which showed partial response of disease, but at the same time, he has experienced a reduced compliance with applications of menthol cream, not related to side effects of the cream itself. At the fifth cycle, after the recovery of patients’ compliance, that trend stopped.
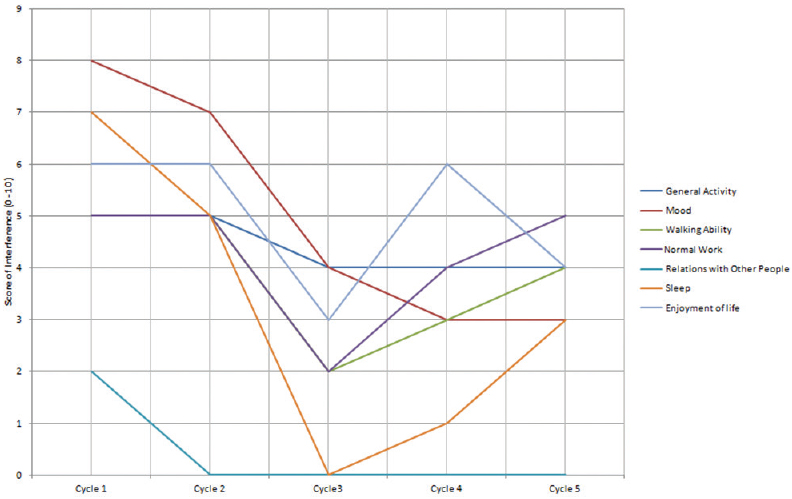
- Changes in the scores at the answer 9 during the cycles
DISCUSSION
Neuropathic pain is a multifaceted symptom, difficult to assess; in some cases, the disability can be so serious as to limit further disease-oriented treatments. Our patient benefits twice from menthol cream application: first, because of the subjective improvements reported during the treatment, that result in a better quality of life, and second, because it enabled an effective chemotherapy dose delivery, without dose discontinuation, which in turn resulted in a longer survival. Improvements in management of CIPN are still required, but topical medications, such as menthol aqueous creams of galenic preparation, could represent a valid palliative option, because of their rapid efficacy, the low cost and the easy accessibility, and because of their being “nondrugs,” which allows avoiding the effect of “adding to the list” on patients. On the other hand, the posology, which requires long-term therapy, with more than one daily application, could influence patients’ compliance. Further studies are required in this setting, to confirm this strategy of the treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Drug Class Review: Neuropathic Pain Update 1 Final Report. Prepared by the Oregon Evidence-Based Practice Center for the Drug Effectiveness Review Project. Portland: Oregon Health and Science University; 2011.
- TRPM8 in health and disease: Cold sensing and beyond. Adv Exp Med Biol. 2011;704:185-208.
- [Google Scholar]
- Transient receptor potential channels on sensory nerves. Handb Exp Pharmacol. 2009;194:261-81.
- [Google Scholar]
- Analgesia mediated by the TRPM8 cold receptor in chronic neuropathic pain. Curr Biol. 2006;16:1591-605.
- [Google Scholar]
- From bench to bedside: A case of rapid reversal of bortezomib-induced neuropathic pain by the TRPM8 activator, menthol. J Clin Oncol. 2008;26:4519-20.
- [Google Scholar]
- Reversal of dose-limiting carboplatin-induced peripheral neuropathy with TRPM8 activator, menthol, enables further effective chemotherapy delivery. J Pain Symptom Manage. 2010;39:e2-4.
- [Google Scholar]
- Cancer treatment-related neuropathic pain: Proof of concept study with menthol – A TRPM8 agonist. Support Care Cancer. 2015;23:2769-77.
- [Google Scholar]
- Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649-55.
- [Google Scholar]
- Increased tolerability of bimonthly 12-hour timed flat infusion 5-fluorouracil/irinotecan regimen in advanced colorectal cancer: A dose-finding study. Oncol Rep. 2006;15:1345-50.
- [Google Scholar]
- Triplet schedule of weekly 5-fluorouracil and alternating irinotecan or oxaliplatin in advanced colorectal cancer: A dose-finding and phase II study. Oncol Rep. 2010;23:1635-40.
- [Google Scholar]
- “Poker” association of weekly alternating 5-fluorouracil, irinotecan, bevacizumab and oxaliplatin (FIr-B/FOx) in first line treatment of metastatic colorectal cancer: A phase II study. BMC Cancer. 2010;10:567.
- [Google Scholar]
- Development and validation of the Neuropathic Pain Symptom Inventory. Pain. 2004;108:248-57.
- [Google Scholar]
- A validation study of an Italian version of the Brief Pain Inventory. Pain. 1996;65:87-92.
- [Google Scholar]






