Translate this page into:
Unraveling the Role of Palliative Surgery in the Era of COVID-19 Pandemic
Address for correspondence: Dr. Seema Mishra, Department of Onco-Anaesthesia and Palliative Medicine, Dr. B. R. AIRCH, AIIMS, New Delhi, India. E-mail: seemamishra2003@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Palliative surgery forms an important pillar of palliative treatment to provide holistic care to cancer patients in the form of providing relief from pain, local control of disease, hemorrhage, and for the purpose of rehabilitation. During the COVID-19 pandemic, we report the successful management of two cases of colorectal cancer which came under the category of high priority and underwent palliative surgery to provide relief from pain.
Keywords
COVID-19 pandemic
high priority
malignant bowel obstruction
palliative surgery
INTRODUCTION
The International Association for Hospice and palliative Care defines palliative care as “The active holistic care of individuals across all ages with serious health related suffering due to severe illness and especially of those near the end of life. The aim is to improve quality of life of patients, their families and caregivers.”[1] The novel coronavirus pandemic has affected the population worldwide, making inroads into the political, economic, social, and health arenas of the countries, thus marking a new epoch in the field of medicine. The pandemic has brought to the fore the requirement of specialist palliative care services during this time as they are expert in the interdisciplinary management of frail, chronically ill patients[2] such as those suffering from cancer and who are expected to bear the maximum brunt of this infectious disease. Since ages in the domain of palliative care related to cancer patients, the focus has largely been on palliative chemotherapy or radiotherapy, with palliative surgery often being overlooked.[3] More so due to the COVID-19 pandemic, health-care systems across the world have ensued the triaging system, leading to many elective surgeries being deferred. It has also forced us to think our surgical strategies because of logistic, ethical, and clinical challenges involved.[4] However, palliative surgeries remain an important pillar of providing holistic care to cancer patients by providing good symptom control in the form of pain management, as well as leading to reconstruction and rehabilitation.[5] Herein, we report two cases who underwent successful palliative surgery admitted during this pandemic.
CASE REPORT
Case 1
An 18-year-old female (45 kg, 152 cm), a known case of Stage IV metastatic sigmoid colon cancer, post 4 cycles of chemotherapy (CAPOX regimen), was admitted in the palliative care unit with complaints of pain abdomen for 10 days, multiple episodes of vomiting, inability to pass stools, and flatus for 3 days. There was no history of fever, cough, and difficulty in breathing at the time of presentation. She resided in the containment zone of the national capital which was the hotspot for coronavirus. X-ray erect abdomen was done which revealed multiple air–fluid levels [Figure 1]. Initially patient was managed conservatively and kept nil per oral. Nasogastric tube was inserted. Injection paractemaol alongwith injection fentanyl infusion was given for managing her pain. After 24 h of conservative management, there was no improvement in signs and symptoms; it was decided to go for contrast-enhanced computed tomography (CECT) abdomen, which revealed single-level obstruction at the level of sigmoid colon with the proximal bowel dilated and the distal segment collapsed [Figure 1]. Keeping in mind the ESMO and ACS guidelines for cancer care prioritization during the COVID pandemic, it was decided to take the case for surgical intervention.[67] However, at the same time, the patient developed fever, so, along with infection control department, it was decided to test for severe acute respiratory syndrome (SARS)-coronavirus before taking up for surgery as the patient came from a COVID-19 hotspot area and fell into the category of immunocompromised patient as well as developed fever despite giving round-the-clock paracetamol. The patient and the family members were explained about the pros and cons of the surgery, and written informed consent was taken. Once the reports of SARS coronavirus came out to be negative, then, the surgical oncologists proceeded with palliative diversion transverse loop colostomy with both the anesthesiologists and the surgeons using full precautions and personal protective equipment. Post procedure, the patient was shifted to the ward, slowly injection fentanyl was tapered, and she got discharged on tablet paracetamol only. One week post surgery, she was called up for follow-up in our outpatient department and reported complete pain relief with stoma functioning well.
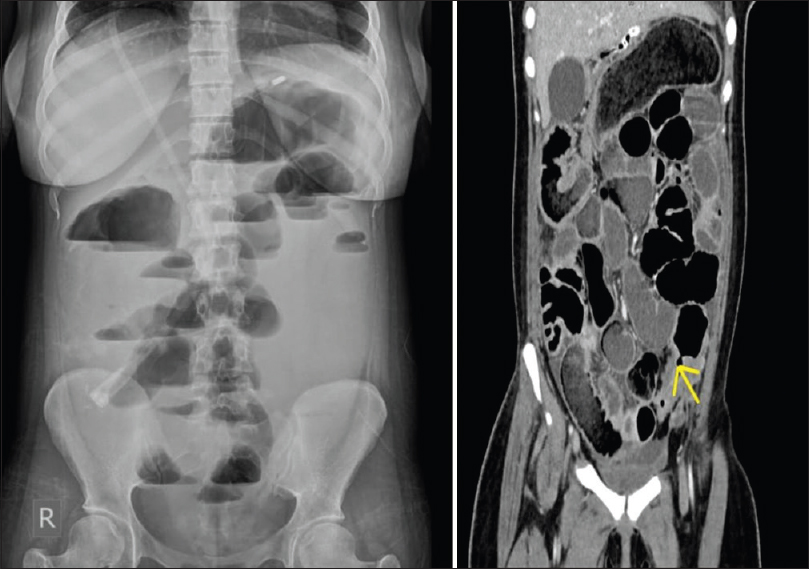
- X-ray erect abdomen showing multiple air–fluid levels. Contrast-enhanced computed tomography abdomen showing obstruction at the level of sigmoid colon with the distal segment collapsed
Case 2
A 27-year-old male (44 kg, 160 cm), a known case of carcinoma anorectum, was admitted under the palliative care unit with complaints of severe pain abdomen for 2 days with stoma not functional for 1 day. He had previously undergone diversion colostomy 1 month back for fecal incontinence and was taking tablet morphine, tablet paracetamol, and tablet gabapentin for pain relief. He had been planned to receive a long course of radiotherapy and chemotherapy before the diversion surgery. This case was also from a COVID hotspot area. During this admission, conservative management was planned initially. He was started on injection fentanyl for pain relief, Ryles tube was inserted, kept nil per oral, and laxative suppository along with enema was given for suspected fecolith as the cause of abdominal pain. With no signs of improvement in the next 24 h and the patient developing guarding and rigidity along with fever, X-ray erect abdomen was done which showed no air under the diaphragm, but CECT abdomen revealed wall defect in the sigmoid colon along with fecal matter collection in the pelvic cavity [Figure 2]. Immediately, the patient was planned for exploratory laparotomy. Goals of care were discussed with the patient and the caregiver. Meanwhile, SARS-coronavirus sample was sent keeping in mind that the patient was immunocompromised and developed high-grade fever. Report for SARS-COVID came out to be negative, and blood products were arranged from the blood bank in view of deranged coagulation function. The patient underwent Hartmann's procedure the same day, which is often used as a palliative intent for perforation of bowel secondary to cancer. Postoperatively, blood transfusion was done in view of anemia, and injection fentanyl was continued for pain relief.
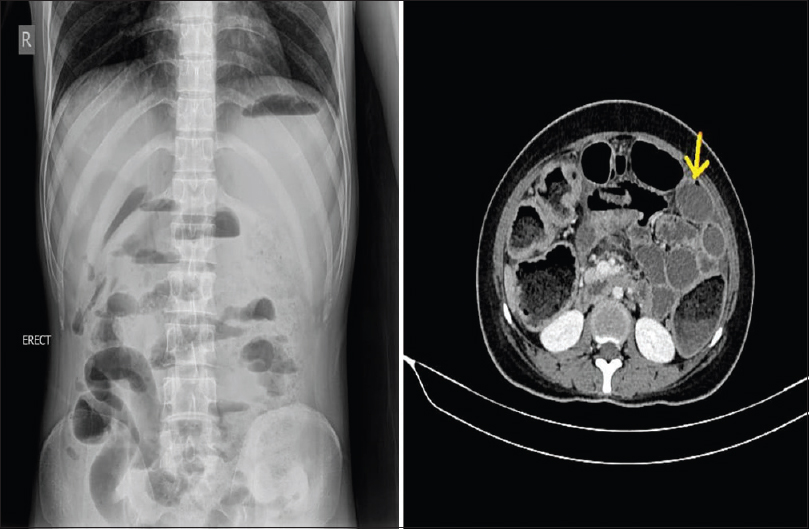
- X-ray erect abdomen does not show air under the diaphragm, but contrast-enhanced computed tomography abdomen shows wall defect in the sigmoid colon
DISCUSSION
Palliative surgery is an important pillar to provide holistic palliative care for cancer patients.[8] Following the principles of palliative care to provide comfort care and improving the quality of life, the goals of palliative surgery are also based on the safety, efficacy, and resolution of symptoms rather than reversing the disease itself which has already advanced.[3] Before proceeding with any kind of palliative surgery, the goals of care should be clearly outlined and discussed with the patient as well as the caregivers that whether it is being done with the intention of local control of disease, control of pain and hemorrhage, or for the purpose of rehabilitation.[5] Both the cases presented by us also highlight that the principle of control of pain was the main motto for proceeding with surgery apart from saving life in the second case. The role of providing specialist palliative care services becomes even more important in these testing times of global coronavirus pandemic. This pandemic has come across as one of the biggest catastrophic mass casualty events the humankind has ever witnessed, with the rising tide of cases affecting millions of people worldwide.[9] Mitigating such a challenge requires an effective response from health-care systems with robust planning. It poses lot of ethical issues, challenges pertaining to the allocation of limited resources as well as alteration of standard of care. However, amidst all this chaos, we must always remember that even though the primary goal remains to save as many lives as possible, at the same time, we must minimize the suffering of the terminally ill patients and they should not be left alone. According to the recent ESMO guidelines for palliative care prioritization during the COVID-19 crisis, gastrointestinal obstructions come under the high-priority category of oncology services that require urgent intervention.[6] Furthermore, the ACS Guidelines for Triage and Management of Elective Cancer Surgery Cases During the Acute and Recovery Phases of Coronavirus Disease 2019 (COVID-19) Pandemic have reported that colorectal cancer patients admitted in the hospitals which have few COVID-19 patients and who are nearly obstructing should undergo surgery as soon as feasible.[7] Keeping abreast with these guidelines, both the cases were admitted in the palliative care unit and intervention was sought from the surgeons at the earliest. We faced a lot of challenges during their management. The first, in front of us, was the ethical dilemma to provide the patient and the family members with honest information and realistic hope about their current situation along with future prognosis, and at the same time, we had to manage their symptoms effectively. For that, we followed the path of effective communication among the surgeons, palliative care physicians, anesthesiologists, and the patient. Second, because of the triaging system ensued due to the pandemic, we had to overcome logistic hurdles also. As it is imperative that all the health-care workers should be protected, we ensured that the patient was SARS-coronavirus negative before proceeding for the surgery. We expedited the whole process of testing, got emergency radiological investigations done, as well as arranged blood products from the blood bank, which was essential during the intraoperative and postoperative period. All the health-care workers in the operation theater also took necessary precautions and made judicious use of personal protective equipment.
Through effective management of both our cases, we have tried to highlight and emphasize that palliative surgeries have a multifaceted impact on the overall outcome and quality of life of the patient and the family members. It also brings to the fore the concept that palliative care is an effective and humane treatment modality during the times of global crisis. All these are feasible with the development of a specialist palliative care team in hospital settings, who can do robust planning, effective communication, multidisciplinary team management, and judicious allocation of resources along with compassionate attitude toward the patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Redefining Palliative Care - a New Consensus-based Definition. J Pain Symptom Manage 2020 S0885-3924(20)30247-5
- [Google Scholar]
- Palliative care pandemic pack: A specialist palliative care service response to planning the COVID-19 pandemic. J Pain Symptom Manage 2020 S0885-3924(20)30177-9
- [Google Scholar]
- Surgical palliation at a cancer center: Incidence and outcomes. Arch Surg. 2001;136:773-8.
- [Google Scholar]
- To face coronavirus disease 2019, surgeons must embrace palliative care. JAMA Surg 2020 101001/jamasurg20201698
- [Google Scholar]
- Oxford Textbook of Palliative Medicine. Ox-Ford Press: Oxford England; 1998. p. :282-97.
- Palliative Care Prioritisation During the COVID-19 Crisis. Available from: https://wwwesmoorg/guidelines/supportive-and-palliative-care/ palliative-care-in-the-covid-19-era
- Palliative care considerations in mass casualty events with scarce resources. Biosecur Bioterror. 2009;7:199-210.
- [Google Scholar]






