Translate this page into:
Impact of Applying Palliative Care on Symptoms and Survival of Patients with Advanced Chronic Disease Admitted to the Emergency Department
Address for correspondence: Dr. Jose P. Amado, 238 Belisario Flores Street Apart 301. Lince, Lima, Peru. E-mail: jpamadot@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
In the emergency department, there is a need to provide palliative care; however, they are not usually administered. The present study evaluates the evolution of the intensity of the symptoms when applying palliative care, in adult patients with advanced chronic disease admitted to the emergency room, and compares survival between those who receive this care and those who do not.
Materials and Methods:
A clinical intervention study was conducted including patients older than 18 years with advanced chronic disease admitted to the emergency room with an indication of palliative support according to the Supportive and Palliative Care Indicators Tool 2015. Three hundred and seven patients were studied (74 in the intervention group and 233 in the group not intervened). In the intervention group, the intensity of pre- and postintervention symptoms was compared (Wilcoxon test). The survival of both the groups were then compared (logrank test).
Results:
There was a significant decrease in pain and dyspnea at 24 and 48 h postintervention (P < 0.01), respectively, while drowsiness increased significantly at 24 h (P < 0.01) but did not change at 48 h (P = 0.38). Excluding patients with better functional status, there was less survival at 3 months in the intervention group (P = 0.01).
Conclusions:
Dyspnea and pain decreased with the application of palliative care but not drowsiness. Survival in the intervention group was lower than in the nonintervention group. However, the reason for providing palliative care is to relieve suffering at the end of life.
Keywords
Emergency department
palliative care
terminal care
terminally ill
INTRODUCTION
Palliative care is a holistic intervention to improve the quality of life of the patient with serious health problems related to oncological and nononcological diseases, especially near the end of life, providing physical, psychological, social, and spiritual support to the patient and family, by a multidisciplinary team.[123] In the world, accessibility to palliative care is not equitable and depends on the development of the local or regional health system.[14]
Patients who go to the emergency department of referral hospitals are increasingly complex, and as far as it is known, there is little information on the proportion of need for palliative care.[56789] In Latin America, there is a disparity regarding the training of health personnel (probably including emergency personnel or intensive care) in palliative care.[1011] This causes procedures to be performed on patients with advanced chronic disease without clear benefits that often prolong their suffering.[4101213]
In Europe, North America, and Oceania, the benefit of palliative care programs in institutionalized, outpatient and home follow-up patients has been demonstrated.[2141516171819] Unlike other programs where the patient is followed to the end, in an emergency, the patient is sought to detect palliative care and direct him to the other programs, but in our country, this is still deficient.[11] Therefore, the objective of this study is to evaluate the evolution of the intensity of symptoms when applying multidisciplinary palliative care in adult patients with advanced chronic disease admitted to the emergency room, as well as comparing survival between those who receive this care and those who do not.
MATERIALS AND METHODS
Quasi-experimental clinical intervention study with two asynchronous groups of patients over 18 years of age with advanced chronic disease admitted to the emergency department of a tertiary hospital. Patients who had (in the history of admission) advanced cancer, advanced chronic noncancer disease, or total functional dependence were included in the study; those who had no indication for palliative support (Supportive and Palliative Care Indicators Tool 2015, adapted and validated in Spanish)[20] and those in whom no informed consent was obtained (from the patient or caregiver) were excluded from the study.
One group received the intervention and the other did not. In the nonintervened group, verbal informed consent was obtained and its evolution was observed with conventional treatment. In the intervention group, an informed consent signature was requested, and during their stay in the emergency room, palliative care was provided by a trained multidisciplinary team (three physicians, six nurses, a psychologist and a social worker), following clinical practice guidelines.[2122]
In both the groups, clinical-demographic variables, functional status with Spanish Palliative Performance Scale (PPS) V2,[23] and symptoms (dyspnea, pain, and drowsiness) according to the Edmonton Symptom Assessment System[24] were measured on emergency admission, and it was survived at 3 months. In the intervention group, symptom intensity was also measured at 24 and 48 h after admission. The evaluations were carried out by one of seven medical specialists (four internists and three emergency physicians) and the doubts were resolved in consensus with the principal investigator.
A sample size was not calculated a priori, recruiting all patients who met criteria for 3 consecutive months, and for the intervention group, all possible patients according to available resources [Figure 1]. Recruitment of the nonintervened group began in February 2017 and the intervention group in July 2017. There was no randomization or blinding for ethical reasons.

- Flow diagram of selection of patients with advanced chronic disease admitted to the emergency room of a tertiary hospital
STATA 14 software (STATACorp., LLC, TX, USA) with a 0.05 level of significance was used, performing a comparison analysis of the study groups, evaluating difference of medians with Mann–Whitney U-test and proportions with Chi-square test. The evolution of the intensity of symptoms of the intervention group was compared using Wilcoxon test. Excluding patients with PPS >50, survival was compared in the study groups (logrank test).
A power analysis was made, concluding that it was suitable for pre and post comparison in the intervention group as well as for comparing survival functions between both the groups. Approval was obtained from the ethics committee of the respective hospital.
RESULTS
Of the total number of patients assigned after applying the criteria and exclusion, losses in follow-up (10.1%) included those readmitted to the emergency room or who changed their intention to participate in the study. For the analysis, those who died within the first 24 h of admission (5%) and those with incomplete data (6.5%) were not considered [Figure 1].
In the total number of patients studied, the age varied between 20 and 100 years. Those with PPS >50 in the control group and in the intervention group constituted 20% and 8%, respectively [Table 1]. The most frequent symptoms were pain, dyspnea, and drowsiness, with a higher percentage of dyspnea in the intervention group (41%) compared to the control group (24%) [Table 1]. The most frequent oncological etiologies in both the groups were genitourinary and gastrointestinal cancer (41% and 35%, respectively), while in noncancer patients, they were dementia, stroke sequelae, and liver cirrhosis (38%, 26%, and 20%, respectively).
| Characteristic | Nonintervention group (n=233), n (%) | Intervention group (n=74), n (%) | P |
|---|---|---|---|
| Age (years)& | 77 (66.5-87.5) | 77 (66-88) | 0.963* |
| Sex, female | 137 (58.8) | 44 (59.5) | 0.920** |
| Oncologic disease | 99 (42.5) | 41 (55.4) | 0.052** |
| Functionality PPS | |||
| <40 | 96 (41) | 38 (51) | 0.047** |
| 40-50 | 90 (39) | 28 (41) | |
| >50 | 47 (20) | 5 (8) | |
| Place of admission | |||
| Shock trauma | 103 (44) | 32 (43) | 0.607** |
| Medicine | 117 (50) | 36 (49) | |
| Surgery/traumathology | 13 (6) | 6 (8) | |
| Symptoms | |||
| Pain | 64 (27) | 21 (28) | 0.879* |
| Dyspnea at rest | 55 (24) | 30 (41) | <0.005* |
| Drowsiness | 61 (26) | 22 (30) | 0.549* |
&Median (percentile 25-percentile 75), *Mann-Whitney U-test, **Chi-square test. PPS: Palliative Performance Scale
Regarding the intensity of symptoms identified in the intervention group, there was a statistically significant difference between pain at admission and at 24 h (P < 0.01) and also at 48 h (P < 0.01) [Table 2]. The same happened with dyspnea (P < 0.01) [Table 2]. In addition, there was a significant difference between drowsiness at admission and 24 h (P < 0.01) but not with drowsiness at 48 h (P = 0.38) [Table 2]. When looking at the graphs, there is a tendency to decrease between admission and follow-up in the case of pain and dyspnea but not in the case of drowsiness [Figure 2].
| Symptom intensity | n | Median | P25-P75 | P |
|---|---|---|---|---|
| Pain | ||||
| Upon admission | 49 | 0 | 0-8 | |
| At 24 h | 49 | 0 | 0-3 | <0.001* |
| At 48 h | 39 | 0 | 0-2 | <0.001** |
| Dyspnea | ||||
| Upon admission | 50 | 5,5 | 0-9 | |
| At 24 h | 50 | 3 | 0-5 | <0.001* |
| At 48 h | 40 | 1 | 0-4 | <0.001** |
| Drowsiness | ||||
| Upon admission | 50 | 0 | 0-4 | |
| At 24 h | 50 | 2 | 0-6 | <0.001* |
| At 48 h | 40 | 2 | 0-3.5 | 0.385** |
*Wilcoxon test comparing values between admission and 24 h. **Wilcoxon test comparing admission values and 48 h
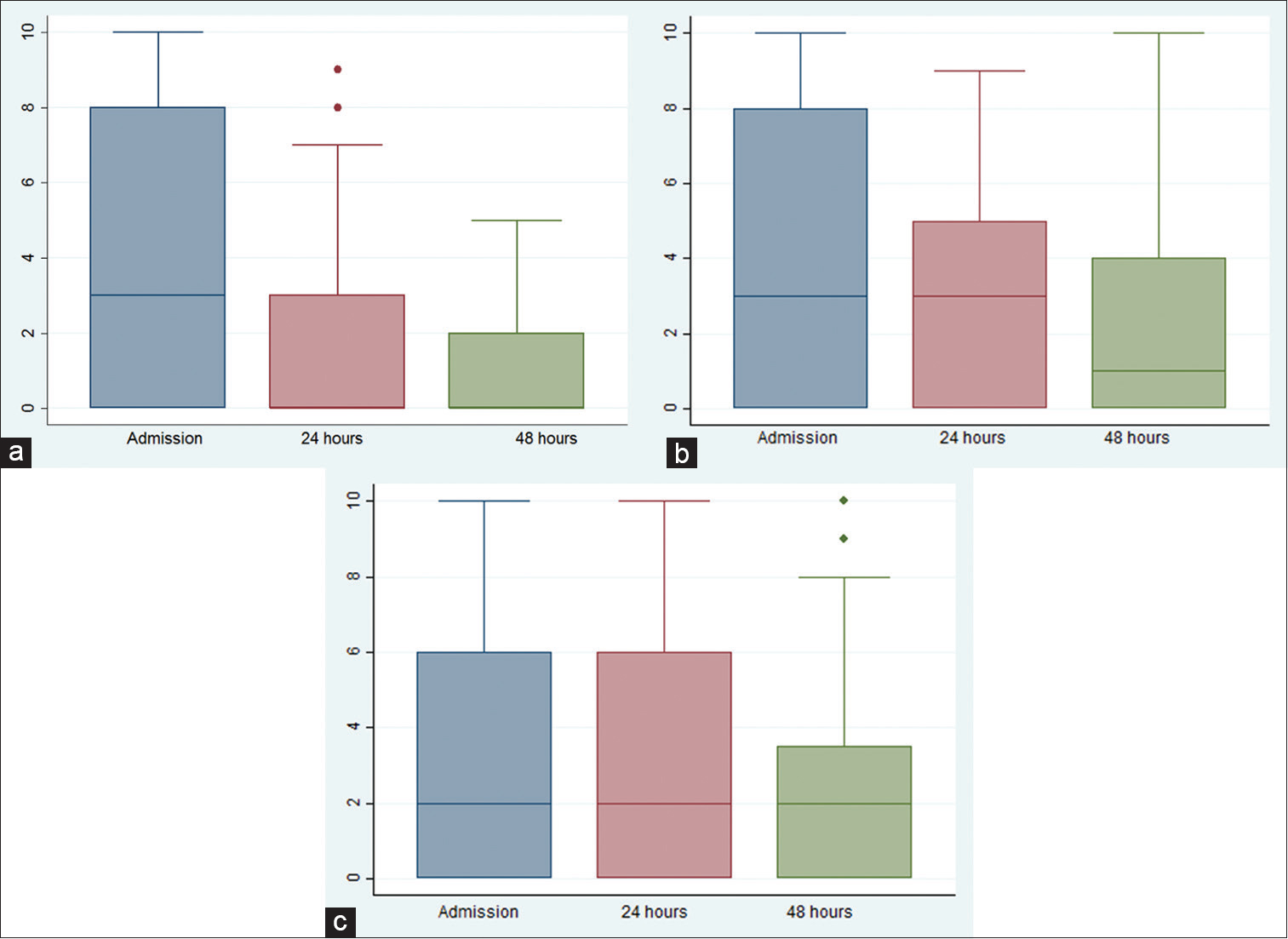
- Evolution of the intensity of symptoms in patients with advanced chronic disease admitted to the emergency room of a tertiary hospital, who received multidisciplinary palliative care. (a) Pain, (b) dyspnea at rest, and (c) drowsiness (according to the Edmonton Symptom Assessment System)
When comparing patients with PPS ≤50, it is observed that between the groups, there is no statistically significant difference in the proportions of the PPS categories (P = 0.22); however, the oncological disease was more frequent in the intervention group (P = 0.02) [Table 3]. In addition, there was a statistically significant difference in patient survival between both the groups (P = 0.01) at 3 months of follow-up, with cumulative survival being greater in the nonintervened group (0.30) and lower in the intervention group (0.19).
| Characteristic | Nonintervention group (n=186), n (%) | Intervention group (n=69), n (%) | P |
|---|---|---|---|
| Functionality PPS | |||
| 10-30 | 96 (52) | 38 (55) | 0.221** |
| 40-50 | 90 (48) | 31 (45) | |
| Age (years)& | 79.5 (65-94) | 77 (66.5-87.5) | 0.465* |
| Sex, female | 111 (60) | 42 (61) | 0.863** |
| Oncologic disease | 69 (37) | 37 (54) | 0.017** |
| Place of admission | 0.514** | ||
| Shock trauma | 92 (50) | 30 (44) | |
| Medicine | 86 (46) | 34 (49) | |
| Surgery/traumathology | 8 (4) | 5 (7) | |
| Symptoms | |||
| Pain | 45 (24) | 17 (25) | 0.941* |
| Dyspnea at rest | 39 (21) | 28 (41) | 0.002* |
| Drowsiness | 39 (21) | 20 (29) | 0.177* |
&Median (percentile 25-percentile 75), *Mann-Whitney U-test, **Chi-square test. PPS: Palliative Performance Score
DISCUSSION
Palliative care has been shown to improve the quality of life at the end of life in patients with advanced cancer,[25] evidence of their benefit in noncancer diseases (such as dementia and heart failure) has also been published;[2627] however, most studies on palliative care have been developed in cancer patients.[28] Underreporting of symptoms in patients with chronic diseases is frequent.[29] In the present study, it was observed as the main finding that dyspnea and pain decrease with the use of palliative care.
Pain is the best known symptom in palliative care. Here, it was presented in a similar proportion to the admission in both the study groups, which were similar to that found in a previous study in the same hospital[12] but smaller than foreign reports where only critical cancer patients were evaluated.[3031] The median intensity did not vary after the intervention, but the 75th percentile did so with respect to admission, which represents a decrease in pain intensity between admission and after the intervention, this decrease being statistically significant [Table 2]. The majority of patients studied were older adults, which is a factor that could induce undertreatment of pain in an emergency department and is consistent with reports of less opioid use in this population.[32] It has been published that there is a greater pain relief in patients who approach the end of life if they are treated for palliative care.[33]
Dyspnea on admission is the most frequent symptom in our intervention group and was greater than in the nonintervened group. In turn, in the intervention group, this was similar to a previous report of the same service[12] but larger than other reports in cancer patients.[3031] The intensity of dyspnea decreased with the intervention according to publications that mention that the use of low doses of strong opioids (e.g., morphine) is effective and safe for oncological and nononcological patients with dyspnea.[3435]
Drowsiness was another frequent symptom in this study, greater than admission in the intervention group than in the comparison group. In turn, this initial drowsiness was greater than in other reports.[1230] An increase in its intensity was found with the intervention and may be associated with adverse effects of treatments used as opioids.[3637]
After matching the value of PPS in both the groups, a predictor of survival,[38] the lower survival of the intervention group could be explained by the higher proportion of cancer patients in the intervention group (which have a lower survival than the nononcological) and the highest proportion of dyspnea in that group, which is reported as an indicator of the arrival of the end of life in oncological and nononcological patients.[39] Palliative care controls symptoms and suffering of the patient and family, also avoiding futile measures and therapeutic obstinacy, without accelerating the time of death but also not prolonging the suffering.[3212240]
The main limitation of the present study included sample size calculation; however, the power analysis to respond to the objectives of the study shows that the number of patients studied was adequate. In addition, it was not possible to compare the effects of the intervention with the evolution of the nonintervened group because there were no follow-up measurements in this; however, the information obtained is useful for future studies.
On the other hand, due to the limited personnel specialized in palliative care in our environment, there could have been difficulties for the collection of information and the administration of the intervention; however, the staff was trained and international guides were tried.[2122] Regarding the selection of the study subjects, patients who had no indication of palliative care could have been inadvertently included; however, a validated instrument was used.[20]
CONCLUSIONS
In adult patients with advanced chronic disease admitted to the emergency department, dyspnea and pain decrease with the application of palliative care but not drowsiness. Survival in the intervened group was lower than in the nonintervened group, probably because the intervened group had a worse prognosis despite having excluded those who had better functional status at the start of the study. However, the goal of palliative care is to alleviate suffering in this last stage of life.
Financial support and sponsorship
37-IETSI-ESSALUD-2016. 2016 Kaelin Research Protocols Award.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Global Atlas of Palliative Care at the End of Life. Geneva, Switzerland: World Health Organization; 2014. p. :111.
- Influencia de la atención avanzada en cuidados paliativos en la frecuentación de las urgencias hospitalarias. Med Paliativa. 2013;20:60-3.
- [Google Scholar]
- International association for hospice and palliative care position statement: Euthanasia and physician-assisted suicide. J Palliat Med. 2017;20:8-14.
- [Google Scholar]
- Alleviating the access abyss in palliative care and pain relief – An imperative of universal health coverage: The Lancet Commission report. Lancet. 2018;391:1391-454.
- [Google Scholar]
- What is the incidence of patients with palliative care needs presenting to the emergency department? A critical review. Palliat Med. 2014;28:1197-205.
- [Google Scholar]
- Analysis of patients evolution in probable situation of the last days in an emergency department. Med Paliativa. 2013;20:10-8.
- [Google Scholar]
- How common are palliative care needs among older people who die in the emergency department? Emerg Med J. 2011;28:491-5.
- [Google Scholar]
- Utilization of palliative care and acute care services in older adults with advanced cancer. J Geriatr Oncol. 2016;7:39-46.
- [Google Scholar]
- Palliative care for patients who died in emergency departments: Analysis of a multicentre cross-sectional survey. Emerg Med J. 2012;29:795-7.
- [Google Scholar]
- Atlas de Cuidados Paliativos en Latinoamérica (1st ed). Houston: IAHPC Press; 2012.
- Palliative care development in Latin America: An analysis using macro indicators. Palliat Med. 2014;28:1231-8.
- [Google Scholar]
- Patients with end-stage oncologic and nononcologic disease in emergency service of an urban tertiary hospital. Indian J Palliat Care. 2018;24:25-7.
- [Google Scholar]
- Palliative care of elderly patients in intensive care units: A systematic review. Rev Bras Ter Intensiva. 2012;24:197-206.
- [Google Scholar]
- Association between palliative case management and utilization of inpatient, intensive care unit, emergency department, and hospice in Medicaid beneficiaries. Am J Hosp Palliat Care. 2015;32:216-20.
- [Google Scholar]
- Integration of palliative care into emergency medicine: The Improving Palliative Care in Emergency Medicine (IPAL-EM) collaboration. J Emerg Med. 2014;46:264-70.
- [Google Scholar]
- Use of a structured palliative care summary in patients with established cancer is associated with reduced hospital admissions by out-of-hours general practitioners in Grampian. BMJ Support Palliat Care. 2013;3:452-5.
- [Google Scholar]
- Reduction of acute hospital admissions and improvement in outpatient attendance by intensified renal palliative care clinic follow-up: The Hong Kong experience. J Pain Symptom Manage. 2015;49:144-9.
- [Google Scholar]
- Community-based palliative care is associated with reduced emergency department use by people with dementia in their last year of life: A retrospective cohort study. Palliat Med. 2015;29:727-36.
- [Google Scholar]
- Emergency care use and the medicare hospice benefit for individuals with cancer with a poor prognosis. J Am Geriatr Soc. 2016;64:323-9.
- [Google Scholar]
- Spanish adaptation and validation of the supportive & palliative care indicators tool – SPICT-ESTM. Rev Saude Publica. 2018;52:3.
- [Google Scholar]
- CE NCCN Guidelines® insights palliative care, version 2.2017 Featured Updates to the NCCN Guidelines. J Natl Compr Canc Netw. 2017;15:989-97.
- [Google Scholar]
- A systematic review in support of the National consensus project clinical practice guidelines for quality palliative care, fourth edition. J Pain Symptom Manage. 2018;56:831-70.
- [Google Scholar]
- The Spanish Adaptation of the Palliative Performance Scale (Version 2) among cancer patients at the end of life: Psychometric properties. J Pain Symptom Manage. 2017;54:570-7.
- [Google Scholar]
- The Edmonton Symptom Assessment System 25 years later: Past, present, and future developments. J Pain Symptom Manage. 2017;53:630-43.
- [Google Scholar]
- Is palliative care support associated with better quality end-of-life care indicators for patients with advanced cancer? A retrospective cohort study. BMJ Open. 2018;8:e018284.
- [Google Scholar]
- Initiating palliative care consults for advanced dementia patients in the emergency department. J Palliat Med. 2014;17:346-50.
- [Google Scholar]
- Palliative care in heart failure: A meta-analysis of randomized controlled trials. Herz. 2019;44:440-4.
- [Google Scholar]
- Selection criteria for patients with non-oncological diseases in palliative care programs and/or services. Med Paliativa. 2010;17:161-71.
- [Google Scholar]
- Is the high intensity symptoms experienced by patients admitted with chronic obstructive pulmonary disease documented by health professionals.– A prospective survey with comparison of patient reported outcomes and medical records? Eur Clin Respir J. 2018;5:1506236.
- [Google Scholar]
- Emergency department visits at the end of life of patients with terminal cancer: Pattern, causes, and avoidability. Am J Hosp Palliat Care. 2016;33:658-62.
- [Google Scholar]
- Symptom assessment and early access to supportive and palliative care for patients with advanced solid tumors in Mexico. J Palliat Care. 2020;35:40-5.
- [Google Scholar]
- The quality of emergency department pain care for older adult patients. J Am Geriatr Soc. 2010;58:2122-8.
- [Google Scholar]
- Specialist palliative care support is associated with improved pain relief at home during the last 3 months of life in patients with advanced disease: Analysis of 5-year data from the national survey of bereaved people (VOICES) BMC Med. 2019;17:50.
- [Google Scholar]
- Opioids for relief of dyspnea immediately before death in patients with noncancer disease: A case series study. Am J Hosp Palliat Care. 2019;36:734-9.
- [Google Scholar]
- Opioids for the management of dyspnea in cancer patients: Evidence of the last 15 years – A systematic review. J Pain Palliat Care Pharmacother. 2015;29:341-52.
- [Google Scholar]
- The burden of opioid adverse events and the influence on cancer patients' symptomatology. J Pain Symptom Manage. 2019;57:899-908.
- [Google Scholar]
- Benzodiazepines for the relief of breathlessness in advanced malignant and non-malignant diseases in adults. Cochrane Database Syst Rev. 2016;10:CD007354.
- [Google Scholar]
- The palliative performance scale predicts survival among emergency department patients, Minia, Egypt. Indian J Palliat Care. 2017;23:368-71.
- [Google Scholar]
- Do the trajectories of dyspnea differ in prevalence and intensity by diagnosis at the end of life? A consecutive cohort study. J Pain Symptom Manage. 2010;39:680-90.
- [Google Scholar]
- Care for the dying patient in emergency departments. An Sist Sanit Navar. 2010;33(Suppl 1):173-91.
- [Google Scholar]






