Translate this page into:
The Need for Palliative Care in Adults in Nepal: Projections Based on Modeling Mortality Data
Address for correspondence: Ms. Eleanor M Swarbrick, University of Bristol, First Floor, 5 Tyndall Avenue, Bristol BS8 1UD, United Kingdom. E-mail: es13281@my.bristol.ac.uk
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims:
With noncommunicable diseases rising in prevalence, Nepal has a significant need for palliative care, but little research has been conducted to evaluate this in depth. This study aimed to generate a quantified estimate of the projected need for palliative care in Nepal.
Subjects and Methods:
The World Health Organization mortality rates were multiplied by the percentage pain prevalence for each disease, to produce an estimate, by disease, of the number of adults requiring palliative care at the end of life. These projections were then broken down for the rural and urban populations. Experts were consulted on the findings to explore how their insight from experience compared to the figures generated.
Results:
Estimates found that there were a total of 58,000 adults needing palliative care in Nepal in 2012. Cardiovascular disease represented the greatest need (21,249) followed by cancer and chronic obstructive pulmonary disease. The majority of those requiring palliative care were found to be in rural areas. However, the majority of provision currently is for cancer in urban areas. Professionals consulted felt that the results were likely to be representative, although many responded that this was a minimum estimate and with more raw data and more diseases included, the figures could be far higher.
Conclusions:
The need for palliative care is great and is mostly represented by cardiovascular and respiratory disease in rural areas. Provision must be adapted and developed to meet this need, but more primary data is needed to inform such decisions.
Keywords
Estimate
need
Nepal
noncommunicable diseases
provision
INTRODUCTION
Palliative care in Nepal has been developing over the last 20 years, with provision being mainly in Kathmandu and other major cities and mostly focused on cancer.[1] Nepal is ranked in the lowest 20% of the world's countries in terms of development.[2] Along with other low-income countries with aging populations and increasing urbanization, it is currently facing a double burden of disease,[3] with causes of death shifting from infectious diseases and maternal and child health disorders to noncommunicable diseases (NCDs). According to the World Health Organization (WHO), over 50% of deaths in low-income countries will be from NCDs by 2030;[4] however, in 2012, it was estimated that almost 60% of deaths in Nepal were already attributable to NCDs.[2]
Nepal does not have a robust system of national disease databases and death registries, so monitoring of disease patterns is difficult;[3] moreover, few surveys have measured the prevalence of NCDs. Those studies which are available disagree on the proportion of deaths which are due to NCDs, but all demonstrate the significant and rising burden of NCDs.[35678910] Very few studies have focused on the need for palliative care.
Patients with NCDs in low-income settings often present to health-care facilities or physicians late.[1112] This is likely to be related to misconceptions about disease, particularly among people with limited levels of education, and restricted access to health care, which in Nepal is particularly affected by its mountainous terrain, with many remote, rural communities.[613] In this context, provision of palliative care to address high levels of suffering is important but also challenging.
The World Health Assembly in 2014 called signatory states to improve palliative care through measures such as increased training, funding, and drug availability, with the aim of palliative care being part of universal health coverage accessible to all.[14] Nepal has responded to this commitment by adopting a national strategy for palliative care which takes a public health approach to ensure that palliative care is available for all who need it, whatever their illness and wherever they live.[15161718]
The Global Atlas of Palliative Care at the End of Life was published in 2014 by the WHO and the Worldwide Hospice Palliative Care Alliance (WHPCA), outlining the availability and need for palliative care globally.[19] The report included a method for modeling the WHO mortality data and pain prevalence figures by disease to project an estimate of the number of people requiring palliative care, region by region. Since modeling is based on pain incidence, it provides a conservative estimate of palliative care need but offers a useful insight into the current level of palliative care needs. Using a modified version of this method, we aimed to generate estimates of the need for palliative care in Nepal which would assist with planning for palliative care provision. The estimates were then shared with a panel of experts in NCD management and palliative care in Nepal and internationally. The objective of this research was to inform policy approaches and palliative care service provision in Nepal, but we hope it is a method which can also be transferable and useful for developers in other countries and thus be of interest to readers more generally.
SUBJECTS AND METHODS
The method for estimating the number of people requiring palliative care is based on multiplying the number of people dying from a particular condition by the percentage pain prevalence (PPP) for the condition. The PPP represents the proportion of people suffering from pain at the end of life and is an evidence-based figure based on a review of the literature undertaken by researchers of WHPCA and provided in Global Atlas of Palliative Care.[19] The number of deaths for each condition for Nepal was taken from the WHO Global Health Estimates (GHE) for deaths by country dataset of the WHO Health Statistics and Information Systems.[20]
The diseases included in the study were those which were judged most likely to have a phase where adult sufferers (age 15 or over) would require palliative care. These corresponded to those listed by the WHPCA which were based on a Delphi study. The diseases included were as follows: cancer, HIV/AIDS, Alzheimer's disease (AD) and other dementias, cardiovascular disease (CVD), chronic obstructive pulmonary disease (COPD), cirrhosis of the liver, diabetes mellitus, kidney disease, multiple sclerosis (MS), Parkinson's disease (PD), rheumatoid arthritis, and tuberculosis.[19]
According to the method, adjustments are made to the initial estimates generated,[19] one-third of the cardiovascular deaths were removed to factor in sudden deaths.
We also made an estimate of the need for palliative care in children, but these results will not be presented in this paper, which focuses on palliative care need in adults.
Estimates for rural and urban palliative care need were initially calculated by multiplying the national figures by the proportion of the population in each (82.7% and 17.3%, respectively).[21] The literature was searched for comparative prevalence in urban and rural areas in South Asia of CVD, diabetes mellitus, COPD, and cancer, and their associated risk factors.
Weighted ratios were calculated for diabetes mellitus and CVD; when factoring in the differing risk factor prevalence, disease prevalence,[3671322] and population size,[21] it was estimated that for both diseases, the ratio of total number of deaths between rural and urban areas was 2:1. There was not sufficient evidence to suggest that there is any urban–rural difference in the incidence of COPD or cancer, so no weighting was applied for these diseases.
Data were also extrapolated to create estimates of the need for palliative care per 100,000 of the national population, based on the national population in 2012.[21]
The findings of the analysis were sent to professionals with experience of NCD management or palliative care in Nepal or other low-income settings [Figure 1]. They were asked to respond to a series of questions related to disease prevalence, need for palliative care, and the method used [Figure 2]. This enabled us to explore whether experience in practice supported the estimates generated in the study.
- Roles of experts consulted
- Questions posed to experts consulted as part of qualitative research
RESULTS
Table 1 gives the results for each disease for which need for palliative care was calculated. Overall, it was estimated that over 58,000 adults required palliative care in Nepal in 2012. More than a third of these patients have CVD, making this the greatest contributor to the need for palliative care [Figure 3]. Patients with cancer and COPD are the other two main groups in need of palliative care, each with more than 11,000 per year. There was relatively little need for palliative care for people with MS, AD, and PD. The majority of the patients needing palliative care live in rural areas, but the prevalence of patients requiring palliative care is relatively higher in urban areas than rural areas [Table 1].
| Disease | Deaths 2012 | Pain prevalence at the end of life (%) | Number of patients needing palliative care | ||||
|---|---|---|---|---|---|---|---|
| Total | Total in urban population | Total in rural population | Per 100,000 population | ||||
| Urban | Rural | ||||||
| Cancer | 13,724 | 84 | 11,528 | 1994 | 9534 | 42 | |
| HIV/AIDS | 3847 | 80 | 3078 | 532 | 2545 | 11 | |
| AD and other dementias | 221 | 47 | 104 | 18 | 86 | 0 | |
| CVD* | 31,714 | 67 | 21,249 | 7083 | 14,166 | 149 | 62 |
| COPD | 17,049 | 67 | 11,423 | 1976 | 9447 | 42 | |
| Cirrhosis of liver | 3759 | 34 | 1278 | 221 | 1057 | 5 | |
| Diabetes mellitus* | 5215 | 64 | 3338 | 1113 | 2225 | 23 | 10 |
| Kidney disease | 3638 | 50 | 1819 | 315 | 1504 | 7 | |
| MS | 34 | 43 | 15 | 3 | 12 | 0 | |
| PD | 187 | 82 | 153 | 26 | 126 | 1 | |
| Rheumatoid arthritis | 61 | 89 | 54 | 9 | 45 | 0 | |
| TB | 5210 | 90 | 4689 | 811 | 3878 | 17 | |
| Total | 84,659 | 58,727 | 14,102 | 44,625 | 297 | 196 | |
*Based on risk factor prevalence, disease prevalence, and population, a weighted ratio for the total deaths was used (2:1 rural: urban) (see method). AD: Alzheimer’s disease, CVD: Cardiovascular disease, MS: Multiple sclerosis, PD: Parkinson’s disease, TB: Tuberculosis, COPD: Chronic obstructive pulmonary disease
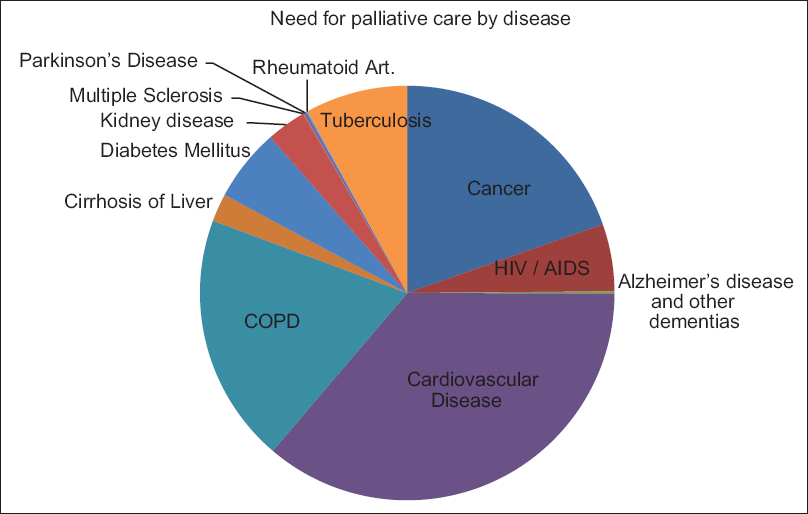
- Pie chart showing relative proportion of adults needing palliative care in 2012 by disease.
Responses from experts contacted suggested that the results were reasonably reflective of their experience in terms of the diseases highlighted. Neurological conditions and rheumatoid arthritis needing palliative care were thought to be more common than the results suggested and suggesting that they might have been underrecorded as the cause of death. Severe injury was highlighted as a disease which, although not listed as globally needing palliative care, may commonly require such management in Nepal. It was suggested that to further understanding, samples and data could be collected from institutions and projects in urban and rural areas. Detailed comments can be seen in Table 2.
| Theme | Comments |
|---|---|
| Agreement with results | “Many of them seem right”[C] |
| “Methods … used for the atlas were followed correctly”[D] | |
| Nonmalignant conditions: “Specialist working in these fields … are best able to deliver the care”[E] | |
| “Numbers seem realistic”[F] | |
| Underestimates | AD, RA, PD: “Not often listed as the cause of death?”[A] |
| RA is reasonably common[C] | |
| Cirrhosis of liver: “Cirrhosis is a huge problem … secondary to alcoholic liver disease”[C] | |
| Severe injury, e.g., burns[F] | |
| Dementia: “Not recognized as cause of death”[H] | |
| Motor neurone disease: “Should be at least similar to MS”[H] | |
| Overestimates | MS: “Never seen any here”[C] |
| PD: “Much less than RA … have not seen an end-stage case”[C] | |
| HIV: “Don’t have so many deaths in regular ART patients”[C] | |
| Comments on method | “Doesn’t consider the duration of needing PC”[A] |
| “Needs relates to the prevalence of an advanced condition rather than the incidence of deaths”[B] | |
| “Prevalence data is quite difficult to obtain”[D] | |
| Double the estimate to account for needs beyond the method definition[D] | |
| “Minimum need”[D] | |
| “Rough estimate”[D,E] | |
| “Made difficult by not having prevalence data in Nepal”[E] | |
| “Prevalence as well as mortality”[F] | |
| “Absence of good population registry data”[G] | |
| Suggestions | Capturing data about migrants/workers with HIV[F] |
| “Census-like data from projects”[F] | |
| Weighting factor for estimating prevalence from death rates[G] | |
| Sample from urban and rural institutions[G] |
Numbers refer to experts’ roles [Figure 1]. AD: Alzheimer’s disease, RA: Rheumatoid arthritis, PD: Parkinson’s disease, MS: Multiple sclerosis, HIV: Human immunodeficiency virus, ART: Antiretroviral therapy
DISCUSSION
Our results show a high level of need for palliative care in Nepal, with the greatest contributor to this need being CVD, COPD, and cancer. Nepal has a predominantly rural population, so the need for palliative care is higher in these areas. Neurological diseases such as AD and PD seem to represent the smallest need for palliative care, but according to experts in the field, the significance of these diseases could be underestimated, and other conditions not listed require palliative care in Nepal, such as severe trauma. Road traffic injuries alone represent the 11th highest cause of disability-adjusted life years and cause an estimated 7–17 deaths per 100,000 per year.[23] The experts consulted agreed that these projections are likely to be an underestimate with numbers of people needing palliative care likely to be greater. This perspective fits with that of the authors of the Global atlas of palliative care (GAPC) at the End of Life[19] who, in discussion with WHO, agreed that a more realistic estimate may be found by doubling the findings (personal communication), since palliative care need does not just relate to pain control at the end of life as identified by this method.
This is the first study reporting a national projection of palliative care need in Nepal. However, other recently published studies enable a comparison with the findings. A cross-sectional survey of inpatients in Kathmandu found that of the 116 inpatients in the 24 h survey period, 35 were found to need palliative care. Nearly, half of these patients had chronic respiratory disease and almost a quarter had CVD.[24] A similar survey in rural Nepal also found that the greatest need for palliative care was in patients with chronic respiratory conditions followed by CVD.[25] Therefore, these studies suggest that deaths from respiratory disease might be underestimated in the GHE data. In addition, both studies report higher proportions of neurological diseases and dementia than the calculated projections, which were suggested by our expert group.
In Nepal, most palliative care is provided for patients with cancer;[126] however, the results of this study indicate that more palliative care is needed for patients with noncancer conditions. This is to be expected since deaths from cancer represent only 8% of the total deaths in Nepal, while deaths from NCDs make up around 60% of all deaths.
The recently adopted national strategy for palliative care has noted that while most of the need for palliative care is in rural areas, most are provided in cities with 80% of the palliative care beds being located in Kathmandu.[126] Steps are being taken to provide appropriate training to health-care workers in rural areas.[1] With its varied geography, different models of palliative care will be needed in different areas of Nepal. Some of the hill districts have only around 150,000 inhabitants compared to more densely populated areas on the plains (Terai) which have more than 500,000 population.[27] Expressing the projected need per 100,000 enables local projection of need to be made by health planners. More densely populated areas with higher levels of need are more likely to justify palliative care teams, whereas sparely populated areas may be better served by upskilling local generalists clinicians including midlevel health workers.[28]
This study has several limitations. The estimates generated were rough initial estimates, providing a baseline from which further research can be conducted. The diseases explored were from a list compiled as significant globally, but which may not be so relevant to the specific setting of Nepal. The data used to generate the projections were from the WHO estimates, not data collected through surveys in Nepal, and therefore, may not be completely robust. The data are also from 2012, and in the last 6 years, the disease profiles are likely to have changed further. Therefore, how representative the data are of the true situation in Nepal is unclear. Pain prevalence is a method of estimating the need for palliative care, distinguishing between the total deaths and the proportion of people dying who need palliative care, but it is likely to underestimate the need quite considerably. In addition, people might need palliative care for longer than 1 year, so this will lead to a further underestimate. The studies which were used to estimate the PPP were difficult to interpret as their definition of the severity, frequency, and duration of the symptom varied,[19] and it is not known how accurate these estimates are. However, despite these caveats, because of the lack of population-based survey data, we believe these projections are a useful indication of palliative care need and can be used to plan services and design further studies to collect primary data.
CONCLUSIONS
There is a great need for palliative care in Nepal which is currently not being adequately met by services available. The majority of this need is for patients with NCDs other than cancer. In the absence of locally generated data from surveys and disease registries, this method is useful for offering a broad foundational assessment and could be used in similar settings internationally. Primary surveys and disease registries are needed to provide robust data which can inform service development.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Palliative care in Nepal: Current steps to achieving universal health coverage. Eur J Palliat Care. 2018;25:40-6.
- [Google Scholar]
- The World Bank. Nepal. The World Bank: Countries 2016. Available from: http://www.worldbank.org/en/country/nepal
- Burgeoning burden of non-communicable diseases in Nepal: A scoping review. Global Health. 2015;11:32.
- [Google Scholar]
- US Department of Health and Human Services National Institute on AgingGlobal Health and Aging. 2011. World Health Organization. Available from: http://www.who.int/ageing/publications/global_health.pdf
- [Google Scholar]
- Epidemiology of chronic obstructive pulmonary disease: A descriptive study in the mid-Western region of Nepal. Int J Chron Obstruct Pulmon Dis. 2012;7:253-7.
- [Google Scholar]
- The burden and determinants of non communicable diseases risk factors in Nepal: Findings from a nationwide STEPS survey. PLoS One. 2015;10:e0134834.
- [Google Scholar]
- Nepal Health Research Council. Non Communicable Diseases Risk Factors: STEPS Survey Nepal 2013. Goverment of Nepal Ministry of Health and Population Nepal Health Research Council. Nepal Health Research Council 2013
- [Google Scholar]
- Nepal Health Research Council. Prevalence of Non Communicable Disease in Nepal: Hospital Based Study. 2010. Kathmandu: Nepal Health Research Council; Available from: http://www.nhrc.org.np/reports/Non_Communicable_diseases.pdf
- [Google Scholar]
- Prevalence of chronic bronchitis in a rural community of the hill region of Nepal. Thorax. 1984;39:331-6.
- [Google Scholar]
- Of what diseases are nepalese people dying? Kathmandu Univ Med J (KUMJ). 2007;5:121-23.
- [Google Scholar]
- Palliative care in South Asia: A systematic review of the evidence for care models, interventions, and outcomes. BMC Res Notes. 2015;8:172.
- [Google Scholar]
- Non-communicable diseases in South Asia: Contemporary perspectives. Br Med Bull. 2014;111:31-44.
- [Google Scholar]
- World Health Assembly. Sixty-Seventh World Health Assembly: Agenda Item 15.5: Strengthening of Palliative Care as a Component of Comprehensive Care throughout the Life Course. 2014. Geneva, Switzerland: World Health Assembly; Available from: http://www.apps.who.int/gb/ebwha/pdf_files/WHA67/A67_R19-en.pdf
- [Google Scholar]
- Cancer Control: Knowledge into Action: WHO Guide for Effective Programmes: Palliative Care. 2007. Geneva, Switzerland: World Health Organization; Available from: http://www.apps.who.int/iris/bitstream/handle/10665/44024/9241547345_eng.pdf;jsessionid=2B5444E4B60D927E61A0C528810B63E8?sequence=1
- [Google Scholar]
- The public health strategy for palliative care. J Pain Symptom Manage. 2007;33:486-93.
- [Google Scholar]
- Supportive, palliative, and end-of-life care for patients with cancer in Asia: Resource-stratified guidelines from the Asian oncology summit 2012. Lancet Oncol. 2012;13:e492-500.
- [Google Scholar]
- What are the key challenges facing palliative care internationally in the next 10 years? Int J Palliat Nurs. 2010;16:316-9.
- [Google Scholar]
- Global Atlas of Palliative Care at the End of Life. 2014. London: Worldwide Hospice Palliative Care Alliance, World Health Organization; Available from: http://www.thewhpca.org/resources/category/global-atlas-of-palliative-careat-theend-of-life
- [Google Scholar]
- Global Health Estimates Summary Tables: Disease and Injury Country Mortality Estimates 2012. 2014. WHO: Health Statistics and Information Systems. World Health Organization. Available from: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index 1.html
- [Google Scholar]
- 2013. UNICEF. Nepal: Statistics. UNICEF Statistics and Monitoring. Available from: http://www.unicef.org/infobycountry/nepal_nepal_statistics.html
- Epidemiology of road traffic injuries in Nepal, 2001-2013: Systematic review and secondary data analysis. BMJ Open. 2016;6:e010757.
- [Google Scholar]
- Palliative care need among inpatients in acute general hospitals in Nepal: A point prevalence survey. J Patan Acad Health Sci. 2017;4:42-6.
- [Google Scholar]
- Population-based need assessment of palliative care in rural Nepal. J Patan Acad Heal Sci. 2017;4:21-6.
- [Google Scholar]
- 2017 IAPCON abstracts: Review of palliative care services in Nepal. Indian J Palliat Care. 2017;23:121-79.
- [Google Scholar]
- Providing palliative care in rural Nepal: Perceptions of mid-level health workers. Indian J Palliat Care. 2018;24:150-5.
- [Google Scholar]






