Translate this page into:
Pediatric End-of-life Care Barriers and Facilitators: Perception of Nursing Professionals in Jordan
Address for correspondence: Dr. Omar Mohammad Khraisat, Almareefa Colleges, Diriyah 11597, Riyadh, P. O. Box 71666, Kingdom of Saudi Arabia. E-mail: khraisat1111@hotmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
End-of-life care is a critical issue for pediatric population with terminal illness to ensure the best possible quality of care for them and their families. A survey was conducted to identify the barriers and facilitators to provide pediatric end-of-life care.
Methods:
A descriptive cross-sectional study was conducted at three tertiary centers providing end-of-life care in Jordan. Two hundred critical care nurses were surveyed (response rate 93%).
Results:
Nurses reported moderate level of experience in all areas of delivering pediatric end-of-life care. The highest scoring of barriers respectively were patients-families barriers having deal with angry family member; health-care professional barriers multiple physicians, involved with one patient, who differ in opinion about the direction care, and where plan of care should go; and organizational barriers not available support person for the family. The highest scoring of facilitators respectively were of patients families facilitators having family members accept that the patient is dying; health-care professional-facilitators having a physician agrees about the direction of care, and organizational facilitators providing family members adequate time to be alone with the pediatric after he or she has died.
Conclusion:
Nurses perceived that patient-family, health-care professionals, and organizational related barriers and facilitators were had the most influence in providing of pediatric end-of-life care. Findings highlighted the need for additional education and support for pediatric staff, across professions, in providing pediatric end-of-life care. A pediatric end-of-life care team should be developed to assist in improving patients’ quality of care and increasing the awareness for the need for a standardized tool to evaluate the nursing competency level concerning pediatric end-of-life care.
Keywords
Barriers
end-of-life care
facilitators
pediatric
INTRODUCTION
Providing pediatric end-of-life care may be the most traumatic facet of nursing according to many researchers.[12]
Pediatric end-of-life was defined by Contro et al.,[3] as “the science and art of lessening physical, psychosocial, emotional, and existential suffering.”[3] Pediatric end-of-life care is a holistic care aiming at improving the quality of life in spite of prognosis. Nurses encounter many unpleasant and disturbing feelings and experiences that may hinder their abilities to provide satisfactory pediatric end-of-life care.[24]
There are many barriers and facilitators for pediatric end-of-life care. Barriers to provide pediatric end-of-life care are categorized into patient-family-related factors, health-care professional-related factors, and organizational-related factors.[4567] Contro et al.,[3] affirms that barriers may occur when health-care providers are prevented from acting according to their professional standards. Determination of these barriers must be achieved to maintain appropriate patient care.[8] When nurses feel they can no longer help the terminally ill recover, they begin to experience a deep sense of sadness, uncertainty, and helplessness and do not know how to cope with the dilemma of providing pediatric end-of-life care.[9] Terminal pediatric patients can suffer from pain and other alarming symptoms because of inadequate symptom management, lack of education, poor communication, and an unspecialized environment because this care most of the time provided in Intensive Care Unit (ICU) which impact the quality of pediatric end-of-life care (Wolfe, Grier, Klar, Levin, and Jeffrey, 2000).[91011]
However, facilitators to pediatric end-of-life care were defined as “any supportive issue that advocates the delivery of optimal pediatric end-of-life care services.”[12] These facilitators to improve pediatric end-of-life care include patient-family, health-care professional, and organization-related facilitators.[46713]
A number of specific interventions, programs, and resources have been suggested to improve care for pediatric end-of-life. In a national survey of ICU directors in the U.S more than 80% of respondents identified helpful strategies to improve end-of-life care in ICUs.[14] These strategies included training of health professionals in end-of-life communication skills, role modeling, and supervision of trainees by clinicians experienced in end-of-life care, and regular meetings of a senior physician and nurse with the patient's family to help reduce conflict about appropriate care goals.[14] Furthermore, ICU directors also offered other strategies including access to consultants with expertise in palliative care, incorporation of end-of-life care within the ICU, hospital and health system quality monitoring programs, and bereavement services.[14]
Other studies identified possible facilitators to provide pediatric end-of-life care and their families including providing a peaceful, dignified bedside environment for the family after a patient's death, acceptance of the family toward the dying patient, and allowing the family adequate time alone with the patient.[4615] However, few of these strategies available in ICUs.[4615]
It is important to remember that the combination of pediatric end-of-life care with curative treatment is essential in providing the child and family with the most holistic nursing care possible. There is much to be done by nursing professionals to secure the future of pediatric end-of-life care programs. The first task is to increase the awareness of pediatric end-of-life care programs and the special needs of nurses who care for pediatric patients in the end-of-life stage. This study would involve clearly identifying the role of the nurses in pediatric end-of-life care specifically and pediatric palliative care in general.
Pediatric end-of-life care is deemed a necessary service in pediatric care units for several reasons. First, many pediatric patients have a significant risk of dying during ICUs admission. Second, a significant part of patient care before death involves extremely invasive and painful procedures. Third, the pediatric patients’ end-of-life care and their families inevitably confront crisis situations to a greater degree in ICUs than during admission to nonintensive pediatric care units.[1617] Yet, many children who survive with significant morbidity are often returned to ICUs and die later.[8] Such situations encounter pediatric care health professionals to efficiently provide quality pediatric end-of-life care that addresses the physical, psychological, and spiritual needs of pediatric patients and their families.
In Jordan, limited evidence exists to identify the barriers that hinder providing end-of-life care, and facilitators that help in providing end-of-life care for pediatric patients in the intensive care setting. This study aimed to identify the barriers and facilitators to provide pediatric end-of-life care the Jordanian intensive care settings.
The research questions were addressed in this study as follows:
-
What are the greatest intense, and the greatest frequently occurring barriers that would hinder providing end-of-life care to pediatric patients as perceived by nurses in the ICUs?
-
What are the greatest intense and the greatest frequent facilitators that would help in providing end-of-life care to pediatric patients as perceived by nurses in the ICUs?
METHODS
Design
A descriptive cross-sectional design was used to identify the barriers and facilitators in providing pediatric end-of-care as perceived by critical care nurses.
Setting
The study was conducted from January 2016 to July 2016 in the ICUs of three tertiary care centers in Amman, the capital of Jordan: One as university center and two governmental centers. These centers provide specialized care services in ICUs for pediatric patients who are critically ill and have multiple complications and/or conditions that require continued hospitalization and advanced treatments.
Study population
Nurses who are providing pediatric end-of-life care in ICUs in Jordan were eligible to participate. Two hundred participants were required based on power = 0.80, alpha (α) = 0.05, and medium effect size = 0.25.[18] All the nurses included in the study practiced end-of-life care in ICUs. Ethical approval was obtained, and standard code of ethics for nurses and the requirements of the Institutional Review Board were followed.
Survey questionnaire
Two questionnaires were used to collect data. The two surveys were conducted using a 5 point Likert scale. Initially, the selection of demographic variables for the proposed study was guided by literature reviewed. Age, gender, level of education, ICU experience, number of pediatric patients given end-of-life care, nurses positions, unit capacity, ICUs’ types were used to describe Jordanian nurses who are providing pediatric end-of-life care in ICUs. The first questionnaire was The Experience of Pediatric End of Life Care questionnaire[3] designed to measure experience and competency of pediatrics end-of-life care in eight items. Experience scale reliability was (Cronbach's α = 0.90). Second, Modified National Survey of Critical Care Nurses Regarding End-of-Life Care Questionnaire (Beckstrand, Kirchhoff, 2008) was used to measure barriers and facilitators to provide pediatric end-of-life care. This questionnaire is comprised 53 items splitting into two subscales with thirty items for barrier subscale, and 23 items for the facilitator subscale. Participants were asked to indicate on a 5-point Likert scale point scale for intensity (0 = not an obstacle, 1 = extremely small, 2 = small barrier, 3 = medium, 4 = large, 5 = extremely large) and participants were asked to indicate on a 5-point Likert scale point scale for frequency (0 = never occurs, 1 = almost never occurs, 2 = sometimes occurs, 3 = fairly often occurs, 4 = very often occurs, 5 = always occurs). Barrier subscale reliability was (Cronbach's α = 0.92). The facilitator subscale splits into a 5-point scale for intensity (0 = not a help, 1 = extremely small, 2 = small help, 3 = medium help, 4 = large help, 5 = extremely large) and 5-point scale for facilitator frequency (FF) (0 = never occurs, 1 = almost never occurs, 2 = sometimes occurs, 3 = fairly often occurs, 4 = very often occurs, 5 = always occurs). Facilitator subscale reliability was (Cronbach's α = 0.96). The barriers and facilitators categorized into three categories: Patient-family category, healthcare-professional category, and organizational category. All questionnaires were translated from English to Arabic and back translated by a panel of three qualified academic doctoral-prepared experts in nursing pediatric care and served as content specialists selected from the Faculty of Nursing at the University of Jordan for content validity purpose.
Analysis
The data were coded numerically and subjected to descriptive and inferential statistical analysis using statistical software (Statistical Package for the Social Sciences (SPSS. 17). SPSS Inc. was a software house headquartered in Chicago and incorporated in Delaware, most noted for the proprietary software of the same name SPSS. The company was started in 1968 when Norman Nie, Dale Bent, and Hadlai “Tex” Hull developed and started selling the SPSS software. Statistical significance was set at P < 0.05. Means were computed from intensity and frequency ratings for each item on the Modified National Survey. An item score was computed for each of the thirty items of barrier subscale. Each item score was calculated by multiplying the mean of the barrier intensity ratings by the mean of the barrier frequency ratings for that item. The range of possible item scores was 0–25. The range of possible values for the barriers scores was 0–750. Similarly, an item score was computed for each of the 23 items of facilitator subscale. Each item score was calculated by multiplying the mean of the facilitator intensity ratings by the mean of the FF ratings for that item. The range of possible item scores was 0–25. The range of possible values for the barriers scores was 0–575.
The barriers and facilitators categorized into three categories: patient-family category, health-care professional category, and organizational category. The questionnaire items as follows represent patient-family-related barriers items: (2, 3, 4, 6, 7, 9, 10, 16, 22, 24), health-care professional-related barriers items are (1, 5, 13, 15, 17, 18, 23, 26, 27, 29), organizational-related barriers items are (8, 11, 12, 14, 19, 20, 21, 25, 28), patient-family-related facilitators items are (31, 37, 48, 50), health-care professional related facilitators items are (32, 34, 36, 38, 40, 42, 44, 45, 46, 52, 53), organizational-related facilitators items are (33, 35, 39, 43, 47, 49, 51, 54).
RESULTS
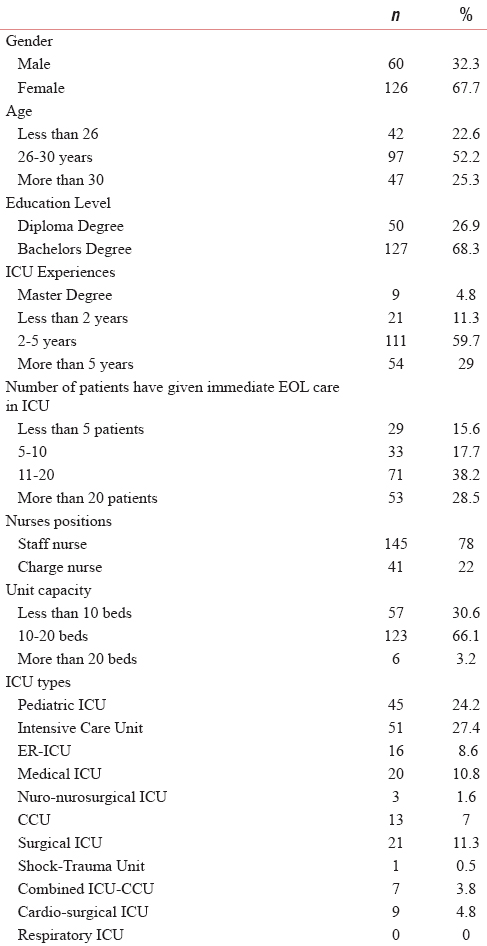
Of the 200 questionnaires distributed, 186 were returned (response rate 93%). The majority of participant's age was ranged between 26 and 30 years 97 (52.2%). Participants were predominately female 160 (67.7%), two-third of them were educated at the baccalaureate level 127 (68.3%) and had 108 (58.1%) of the participants 2–5 years of nursing experience in critical care. The majority of participants 72 (38.2%) were dealt with more than twenty children during the period of dying and were predominately they hold staff nurses position 145 (78%) as shown in Table 1.
Nurses reporting moderate level of experience in all areas of delivering pediatric end-of-life care starting by coordinating care of dying patients, managing symptoms, pain management, discussing transitioning from curative treatment to end-of-life care, discussing Do Not Resuscitate status with patients and families, and ending by acting as mentor or role model to younger colleagues (scale anchors range from 1 to 4; mean ranged = 2.33 [0.79] to 2.57 [0.71]) indicating that nurses require further training in end-of-life care for pediatric patients.
Barriers to provide pediatric end-of-life care
Barriers were grouped into three main categories: Patient-family category, health-care professional category, and organizational category. Nurses reported that the greatest frequent and intense patient-family related barrier to provide pediatric end-of-life care was deal with angry family member situation (mean = 12.51) as shown in Table 2. As well, nurses reported that the greatest frequent and intense health-care professional related barrier to provide pediatric end-of-life care was multiple physicians, involved with one patient, who differ in opinion about the direction care, should go (mean = 10.05). Finally, nurses reported that the greatest frequent and intense organizational related barrier to provide pediatric end-of-life care was not available support person for the family such as a social worker or religious leader (mean = 9.03) as shown in Table 2.

Facilitators to provide pediatric end-of-life care
Facilitators were grouped into three main categories including patient-family category, health-care professional category, and organizational category. Nurses reported that the greatest frequent and intense helpful patient-family-related facilitator to provide pediatric end-of-life care was having family members accept that the patient is dying (mean = 9.94) as shown in Table 3. The greatest frequent and intense helpful health-care professional-related facilitator to provide pediatric end-of-life care was having the physicians involved in the patients care agree about the direction care should go (mean = 11.10). Moreover, the greatest frequent and intense helpful organizational-related facilitator in providing end-of-life care to pediatric patients was allowing family members adequate time to be alone with the patient after he or she has died (mean = 11.10) as shown in Table 3.

DISCUSSION
Providing end-of-life care for pediatric patients and their families can be stressful for nurses because they may be insufficiently trained to manage the process. The process of dying in an ICU can be complicated. Nurses who have chosen to work in ICU settings can find the confusion associated with death unpleasant. A better understanding of the greatest intense and the greatest frequently occurring barriers that restrict nurses from providing quality of pediatric end-of-life care could lead to increase the awareness and testing of interventions to lower both the intensity and the frequency of these barriers. Understanding the greatest intense and greatest frequent facilitators could lead to the development of interventions to maintain the highly rated supportive behaviors and increase the lower rated supportive behaviors.[15] The study aimed to identify barriers and facilitators to provide pediatric end-of-life care in ICUs in Jordan through surveying nurses’ perceptions.
Nurses reported are moderately experienced, in average in all areas of delivering pediatric end-of-life care, from coordinating care of end-of-life for pediatric patients to acting as mentor or role model to younger colleagues. These results indicated that pediatric end-of-life care training might be primarily occurring informally (i.e., through personal and clinical experiences). As well, there is often a strong dependence on trial and error in learning to care for pediatric end-of-life care (Hinds, Oakes, Furman, Quargnenti, Olson, and Foppiano 2001).[19] Moreover, hands-on training is inadequate and ineffective at improving their ability to provide pediatric end-of-life care during work.[20] Together, these findings provide strong support for the need for formalized training in pediatric end-of-life care.
This study is consistent with Higginson et al.[21] (2003) study in which the nurses reported inexperienced with regard pediatric end-of-life care, namely in pain and symptoms management, and felt particularly distressed when a pediatric patient appeared to be suffering.
Inexperienced in pediatric end-of-life care can cause nurses to feel less competent and often result in susceptibility to feelings of burnout, inadequacy, and discomfort.[3] Consequently, despite the availability of guidelines regarding the need for instruction in caring for terminally ill pediatric patients during training, the majority of nurses never receive formal instruction in end-of-life care.[2622]
Perceived barriers
Barriers are the factors that hinder providing end-of-life care for pediatric.[3] Barriers were grouped into three categories: patient-family-related category, health-care professional-related category, and organizational-related category.
The greatest barrier patient-family-related category was dealing with an angry family member; the finding was consistent with studies of[6132324] that reported the highly rated barrier to provide pediatric end-of-life care was dealing with anxious family members. This status might be related to the time surrounding the death of pediatric is extremely tense and stressful for parents and family members. Further, parents reported they are increasing stress from seeing the child suffer and from fearing the death of the child, particularly because they are unable to protect their child, and they did not know much about the disease (Mularski et al. 2005).[42526] These stressors cause a sense of deep helplessness for parents, and they need compassionate support from caregivers; nurses are well-positioned to provide such support.[41027] Thus, nurses must make time to listen when family members need to express their feelings, to provide words of comfort and talk openly and honestly about grief.
Moreover, “multiple physicians involved in the care of one patient who differ in opinion about the direction of care” was rated as the greatest barrier related to health-care professionals. This finding is consistent with to studies.[415] Pediatric patients who are critical ill mostly confronted compound diseases that needed involvement of several different specialties of physicians. Among these separate groups of specialties, there are frequent differences in opinion regarding the plan for a patient's treatment. These separate specialists often fail to communicate or collaborate effectively with each other, further fragmenting care.[428]
ICU nurses confront stressful consequences of fragmented caregiving, including communication of inconsistent or conflicting information to patients and families, failure to achieve clarity about care goals.[614] According to Beckstrand and Kirchhoff,[15] communicating the pediatric end-of-life care decisions to the family is a challenge for nurses, because nurses feel poorly prepared to provide information about expected prognosis.
Finally, “no available support person for the family such as a social worker or religious leader” was ranked as the greatest organizational-related barrier. Jordanian intensive care nurses felt that lack of support personnel for the family was an important barrier standing against providing pediatric end-of-life care. Interdisciplinary team is a cornerstone to enhance the quality of pediatrics end-of-life care.[29] The interdisciplinary team of pediatric end-of-life care is not well established in the selected centers. In addition, nursing shortage certainly increases the workload for intensive care nurses. They have to simultaneously deal with patients whose lives are being maintained and those whose lives are ending. The intensive care nurses may feel it is too much to tolerate these situations alone. Therefore, they need support and assistance from others such as social workers or religious leaders in moving through the pediatric end-of-life care process with their patients.
Perceived facilitators
Facilitators are the factors that may be helpful to facilitate the enhancement of end-of-life care services.[3] Facilitators were grouped for three categories: patient-family-related category, health-care professional-related category, and organizational-related category.
The greatest patient-family-related facilitator that reported by nurses was: Having family members accept that the pediatric patient is dying. The finding of the present study consistent with studies reported earlier.[47132430]
A family member who accepts the pediatric patient who is dying encourages other family members to accept end-of-life care earlier, leading to better quality of life and less suffering for the pediatric patient (Wolfe et al., 2000).[11] As well, family members who realize the valued time that they have to spend with their loved one[4] are more likely to facilitate quality of pediatric end-of-life care.
Moreover, the greatest health-care professional-related facilitator reported by nurses was “having involved physicians agree about the direction of pediatric end-of-life care.” The finding of the present study consistent with studies reported earlier.[4132324] The finding directed the need for physicians as a gatekeeper to stop aggressive treatment and to cooperate with the other health care providers to provide pediatric end-of-life care. In line with existing pediatric literature, collaboration among physicians should be the basis to provide quality of pediatric end-of-life care.[473132]
The advantages of collaboration are 2-fold: First, communication and sharing among experts allows treatment to proceed in the same direction leading to integrated care, and second, the consistency of information facilitates parental decision making.[433] Nurses may deal with involved physicians who are not keeping the direction of care on the same pathway. As patient advocates, nurses need to encourage collaboration to ensure that the care that patients and families receive from different specialties is connected in a consistent way.
Finally, the greatest facilitating factor that relate to organization support was: Allowing family member's adequate time to be alone with a pediatric patient after he or she has died. The finding reflects the nurses’ need for legislative and administrative support to provide psychological and spiritual therapy for pediatric and their families in end-of-life stage.
In line with this finding, studies were consistent.[4132434] Prior evidence supports that psychological stress after the death of a child could seriously influence health outcomes of parents.[435] Allowing adequate time alone after a child has died respects and preserves the parent-child relationship and allows parents to fulfill their roles as a caregiver and guardian for their child.[434] Several studies document the essential need for parents to stay with their child's body in a sad time.[41036] This could help parents to cope with their early grief and may positively shape long-term sadness.[4]
CONCLUSION
The study concluded that the greatest barrier of patient-family-related category to provide pediatric end-of-life care as perceived by nurses was dealing with an angry family member. In addition, multiple physicians involved in the care of one patient who differ in opinion about the direction of care was rated as the greatest barrier related to health-care professionals to provide pediatric end-of-life care, and no available support person for the family such as a social worker or religious leader was rated as the greatest organizational-related barrier. Furthermore, having family members accept that the pediatric patient is dying care was rated as the greatest facilitator related to patient-family category to provide pediatric end-of-life care. As well, involved physicians agree about the direction of pediatric end-of-life care plan was rated as the greatest facilitator related to health-care professionals. Finally, the greatest facilitating factor dealing with organization support was allowing family members adequate time to be alone with a pediatric patient after he or she has died.
Limitations of this study
Considering the importance of the issue studied. The limitations of this descriptive study must be considered in interpreting the results. The study involved a small sample of nurses from critical care unit only, and the findings may not be representative of the perceptions of pediatric end-of-life care among nurses in other settings. As well, this study was limited to three centers located in Amman the capital, which limits the external validity of the findings. Future research should include additional studies with a larger sample size recruited from other hospital settings. More descriptive studies are still needed to gain a comprehensive understanding of the quality of pediatric end-of-life care, barriers and facilitators to provide pediatric end-of-life care in Jordanian ICUs. This is an important step before moving to interventional studies. Polit and Beck[37] advised that interventions often fail because they are designed without an adequate understanding of the problem and the relationship between variables.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Good death? An exploration of newly qualified nurses’ understanding of good death. Int J End Life Nurs. 2012;8:532-9.
- [Google Scholar]
- Home pediatric compassionate extubation: Bridging intensive and end-of-life care. Am J Hosp End Life Med. 2006;23:224-8.
- [Google Scholar]
- Hospital staff and family perspectives regarding quality of pediatric palliative care. Pediatrics. 2004;114:1248-52.
- [Google Scholar]
- Caring for caregivers: Assessing grief and coping of pediatric palliative care nurses. J Hosp Palliat Nurs. 2014;16:1-10.
- [Google Scholar]
- An assessment of nurses’ knowledge and attitudes toward end of life care pain management. J Pain Symptom Manage. 2014;3:25-32.
- [Google Scholar]
- Critical care nurses’ perceptions of quality of dying and death, barriers, and facilitators to providing pediatric end-of-life care in Thailand. Unpublished Dissertation. Case Western Reserve University. 2010
- [Google Scholar]
- End-of-life medicine in neonatal and pediatric intensive care. Child Adolesc Psychiatr Clin North Am. 2006;15:759-77.
- [Google Scholar]
- Interdisciplinary interventions to improve pediatric end-of-life care and reduce health care professional suffering. End Life Nurs. 2009;9:922-33.
- [Google Scholar]
- Improving the quality of end-of-life care in the pediatric Intensive Care Unit: Parents’ priorities and recommendations. Pediatrics. 2006;117:649-57.
- [Google Scholar]
- Symptoms and suffering at the end of life in children with cancer. N Engl J Med. 2000;342:326-33.
- [Google Scholar]
- Critical care nurses’ perceptions of obstacles and helpful behaviors in providing end-of-life care to dying patients. Am J Crit Care. 2000;9:96-105.
- [Google Scholar]
- Emergency nurses’ perceptions of size, frequency, and magnitude of obstacles and supportive behaviors in end-of-life care. J Emerg Nurs. 2008;34:290-300.
- [Google Scholar]
- Identifying and overcoming the barriers to high-quality palliative care in the Intensive Care Unit. Crit Care Med. 2006;34(11 Suppl):S324-31.
- [Google Scholar]
- Providing end-of-life care to patients: Critical care nurses’ perceived obstacles and supportive behaviors. Am J Crit Care. 2005;14:395-403.
- [Google Scholar]
- End-of-life care in Jordan: Culturally sensitive practice. J End Life Med. 2008;11:1292-4.
- [Google Scholar]
- Nurses’ perception towards caring for end of life pediatric patient in Mansoura University Hospitals. J Med Biomed Sci. 2010;5:16-23.
- [Google Scholar]
- End-of-life decision making by adolescents, parents, and healthcare providers in pediatric oncology: Research to evidence-based practice guidelines. Cancer Nurs. 2001;24:122-34.
- [Google Scholar]
- Pediatric residents’ clinical and educational experiences with end-of-life care. Pediatrics. 2008;121:e731-7.
- [Google Scholar]
- Is there evidence that palliative care teams alter end-of-life experiences of patients and their caregivers? J Pain Symptom Manage. 2003;25:150-68.
- [Google Scholar]
- Pediatric end-of-life care moving forward: Empathy, competence, quality, and the need for systematic change. J End Life Med. 2006;9:847-9.
- [Google Scholar]
- Oncology nurses’ perceptions of obstacles and supportive behaviors at the end of life. Oncol Nurs Forum. 2009;36:446-53.
- [Google Scholar]
- Pediatric end-of-life care obstacles and facilitators in the critical care units of a community hospital. J Hosp End Life Nurs. 2008;8:92-102.
- [Google Scholar]
- Traumatic stress in parents of children admitted to the pediatric Intensive Care Unit. Pediatr Crit Care Med. 2004;5:547-53.
- [Google Scholar]
- Transcending the silos: Toward an interdisciplinary approach to end-of-life care in the ICU. Intensive Care Med. 2006;32:15-7.
- [Google Scholar]
- Food, toys, and love: Pediatric end-of-life care. Current problems in pediatric andadolescent health care. J Hosp End Life Care. 2011;35:370-86.
- [Google Scholar]
- Providing a “good death”: Critical care nurses’ suggestions for improving end-of-life care. Am J Crit Care. 2006;15:38-45.
- [Google Scholar]
- Nursing interventions to promote dignified dying in four countries. Oncol Nurs Forum. 2007;34:1151-6.
- [Google Scholar]
- Death in the pediatric ICU: Caring for children and families at the end of life. Crit Care Nurs Clin North Am. 2005;17:349-60, x.
- [Google Scholar]
- End-of-life issues in Intensive Care Units: A national random survey of nurses’ knowledge and beliefs. Am J Crit Care. 2001;10:216-29.
- [Google Scholar]
- Parental coping and bereavement outcome after the death of a child in the pediatric Intensive Care Unit. Pediatr Crit Care Med. 2001;2:324-8.
- [Google Scholar]
- Family conflict at the end of life: Lessons learned in a model program for pediatric patients. J End Life Med. 2010;9:791-801.
- [Google Scholar]
- Barriers to palliative care for children: Perceptions of pediatric health care providers. Pediatrics. 2008;121:282-8.
- [Google Scholar]
- Nursing Research: Principles and Methods (9th ed). Philadelphia: Lippincott; 2010.






