Translate this page into:
Attitudes and Knowledge of Iranian Nurses about Hospice Care
Address for correspondence: Dr. Hossein Jabbari; E-mail: hosseinhosseinj@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Due to expansion of chronic diseases and increase of health care costs, there is a need for planning and delivering hospice care for patients in their final stages of life in Iran. The aim of the present study is to investigate the knowledge and attitudes of nurses about delivering hospice care for End of Life (EOL) patients.
Materials and Methods:
This cross-sectional study was conducted in 2012 with a sample size of 200 nurses that were selected by convenient (available) sampling. The data collection instrument was a self-administered questionnaire whose validity was approved by experts’ opinions and its reliability was approved by test-retest method.
Results:
Among all participants of this study, 87% were female. The mean age of nurses was 32.00 ± 6.72. From all respondents 62% stated that they have no knowledge about hospice care and 80% declared that need for hospice care is increasing. Most of the participants felt that, appropriate services are not presented to patients in the final stages of their lives. About 80% believed that hospice care leads to reduction of health care costs, improvement of physical, mental and social health of patients and finally improvement of the quality of health care services. There was a significant relationship between age, employment history and level of education of nurses and their attitude and knowledge about how this service is provided.
Conclusion:
In view of the increase in chronic illnesses and the costs of caring, the need for provision of hospice care is felt more and more every day. However the awareness level of nurses about these services is low. Therefore the need for including these issues in nursing curriculum and holding scientific courses and seminars in this field is needed.
Keywords
Attitude
End of life
Hospice
Knowledge
INTRODUCTION
The term “hospice” originates from “ Hospitum” which was an inn on the road during medieval times providing a place of shelter and rest for travelers, pilgrims and the sick and injured warriors.[1] At present time, this term suggests the site or the system of care for patients in their final stages of life.[2] In fact end of life (EOL) patients are those who won’t be alive for more than 6 months, and are in a phase of illness trajectory where there is no possibility of any cure or disease modification.[3] Nowadays, hospice care has become increasingly important to patients and their families. These patients have many different physical, social and emotional needs, and most of their deaths (about 70%) occur in hospitals.[45] In 2002 about 885,000 people used hospice services in America. In recent years, this figure has increased by 15% and 90% of cancer patients used such services.[6]
Despite the emergence of advanced diagnostic and treatment technologies in hospitals, scope of hospital based treatment is limited in EOL patients. These groups of patients usually receive limited professional care, and their families have limited knowledge and skills about palliative care.[7]
Nurses are one of the most important groups who have a very significant role in providing care for EOL patients.[4] Due to the nature of the nursing profession, nurses are the first people who are in contact with the patients and their families.[8] Caring, comforting and giving solace to dying patients and their families are one of the most difficult and important duties of nurses. The role of the nurses in this case is to help patients and their families accept and understand death.[9] Due to the crucial role of nurses in delivering the needed care for EOL patients, they must commit themselves to learn special skills and have appropriate attitudes toward these patients.[1011]
Since hospice services have not yet been designated and operated in Iran and there is no study conducted in this field in Iran, the current study aims to assess knowledge and attitudes of Iranian nurses about the hospice care in order to provide suitable information and background for planning and delivering these services in Iran.
MATERIALS AND METHODS
This cross-sectional study was conducted in 2012 with a sample size of 200 nurses in Iran. They were selected by convenience (available) sampling method. All nurses agreed to participate in the study and they, therefore, signed the consent form. Data were gathered with a self-administered questionnaire (based on our two recent studies). The content validity of the questionnaire was assessed by a group of experts in the related field (the questionnaire was modified based on the experts’ comments). To assess the reliability of knowledge constructs, the test retest method was used. The internal consistency for the questionnaire was calculated using Cronbach's alpha coefficient and it was 0.7. The questionnaire included six demographic questions, two questions about experience of contacting with and providing service to EOL patients, two questions regarding nurses’ knowledge about hospice, seven questions about nurses’ attitudes toward providing care to EOL patients and eight questions about nurses’ attitude toward results of hospice care. A five-point Likert scale was used to score this section of the questionnaire, (0 = strongly disagree, 1 = disagree, 2 = no opinion, 3 = agree, and 4 = strongly agree). After completion of the questionnaire by the nurses, the obtained data were analyzed using SPSS: 13.0 software and statistical tests (descriptive, independent t- test and Chi-Square). Ethical approval was obtained from the medical research ethics committee of Tabriz University of Medical Sciences and the confidentiality of the data was assured.
RESULTS
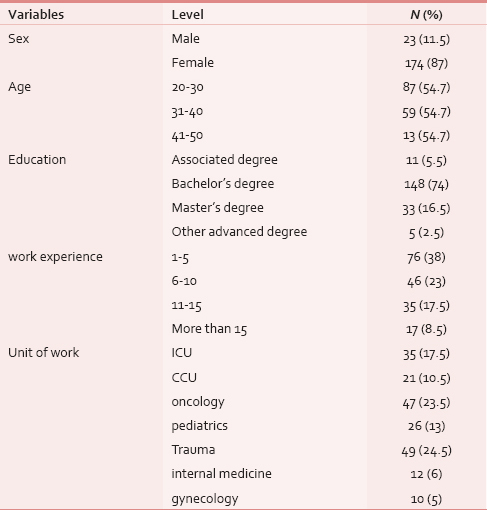
Out of a total of 200 nurses, 174 (87%) were female and 148 (74%) had bachelor's degree. The average age of the respondents was 32 years (SD = 6.72). The demographic characteristics of the respondents are presented in Table 1.
Sixty two percent of respondents stated that they do not have any sufficient information about the hospice care. And about 37% also mentioned that they have little knowledge about this area. Most common sources of information about the hospice care include journals, internet and seminars.
The results of the hospital nurses’ attitudes toward hospice care is summarized in Table 2.
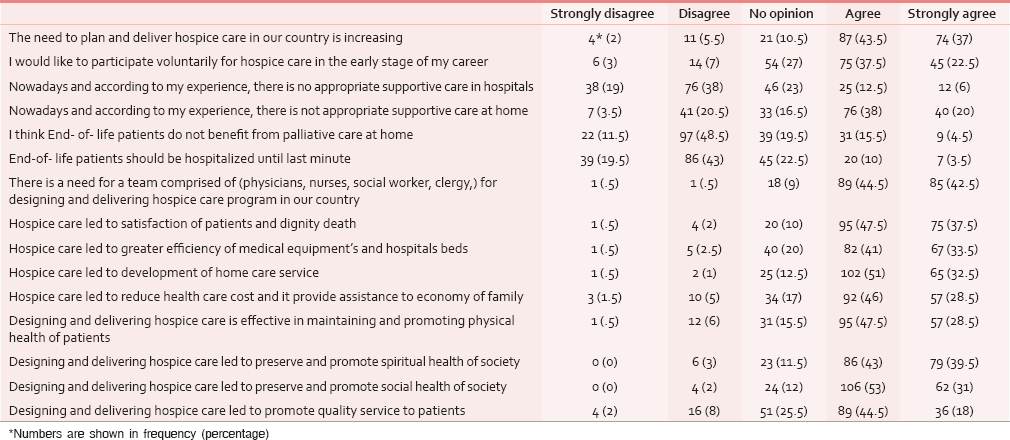
As Table 2 shows, about 80% of the respondents expressed that there is an increasing need for hospice care in Iran. About 61% of the participants were willing to cooperate in designing and delivering hospice care. According to the nurses’ experiences and views, currently there are not enough appropriate services for EOL patients in hospitals and homes. Most of the nurses disagreed with the belief that EOL patients can’t be cared at home. Approximately 87% of respondents stated that a team comprising doctors, nurses, social workers and clergies are required for planning and delivering hospice care in our country.
There was a significant relationship between age, experience and education among nurses and their knowledge about and attitudes toward delivering hospice care. Increasing age, education, and experience of the nurses, tended to enhance their knowledge toward hospice care and they develop a positive attitude toward hospice care.
DISCUSSION
This study provides important information about the level of nurses’ knowledge and their attitudes toward hospice in Iran. The scores of knowledge and attitudes regarding hospice care among the nurses studied in this study were low. In other words, these results demonstrated that the nurses’ knowledge about and attitude toward hospice care is far from optimal. Most of them (80%) believed that the current system of hospice care is not appropriate.
The findings of this study revealed that Iranian nurses have a positive attitude toward hospice care service. In appropriate circumstances, nurses can constitute a relationship with patients to improve both patient care and their quality of life. This finding is consistent with beliefs and attitudes (positive attitude) among nurses about EOL Care in Hungary and the United States.[12]
In the current study, the nurses’ awareness was low and about 62% of them had no information about hospice care and just a small percentage of them had little information regarding this issue. Some studies also reported similar results.[1314151617] However, nurses who participated in Laura and colleagues[18] study had high awareness about these services and the majority of them (70%) had received training in this area during the past 5 years. This indicates the importance of planning and revising of nursing curricula so that courses related to care of EOL patients should be included in the curricula of the programs provided by universities of medical sciences in Iran.
According to the perception of nurses who participated in this study, different providers in the health care system should be included in a hospice care service team. This finding is consistent with findings of our previous study in this regard.[19] Also a study of Torben Bruecjner conducted in Germany[20] showed that proficient persons and experts in various fields of the health care system should contribute in delivering this service. In this regard, it has been suggested that various health care providers be included in a hospice care team.[212223]
Participants of this study believed that delivering hospice care in Iran may lead to cost reduction of healthcare and treatment in Iran. This reduction was also investigated in a study conducted by Gozalo et al., (2008). They investigated the government spending for hospice care at home.[24] Also results of some previous studies show that hospice care can reduce healthcare costs.[252627] The reasons for this cost reduction might be lower inpatient length of stay in hospital, lesser usage of expensive medications, as well as restricted use of diagnostic tests.[28] Furthermore, the participants in this study believed that hospice care service may lead to decreased referrals and workload at hospitals as well as increase the home care service. Gozalo et al., in their study conducted in Brown University concluded that providing this service causes higher efficiency of hospital services and also enhances the palliative care at home.[29]
In the current study, 80.5% of participants believed that there is an increasing need for hospice care and it should be provided in the health care system. These findings are consistent with the results of a study conducted by Dumitrescu et al., in Romania in which physicians mentioned that such service should be offered at a level more than the current one.[30]
The results of this study revealed that more than half of the participants (62.5%) disagreed that EOL patients should be hospitalized until last minute. This reiterates the fact that nurses prefer hospice care to hospital care. Kang and colleagues’ study in Taiwan (2012) shows that hospice care provided cost-efficient and high quality services for end-of-life patients when compared to general acute ward care.[31]
There are limited studies investigating hospice care in Iran. This study provides some quantitative data related to the knowledge of health providers about this service in hospitals. We hope these findings lead to the development of quality improvement measures in Iranian hospitals and larger scale studies.
CONCLUSION
Given the changes in the pattern of diseases throughout the world, especially in Low and Middle Income countries such as Iran, as well as the increase in chronic disease and related care costs in hospitals, planning and delivering hospice care in health care systems is of great importance.
In addition, the findings of this study reveal that the level of awareness and knowledge among nurses about this service is low. It is necessary to introduce educational courses regarding hospice care for nurses in their program curriculum. They also need continuing education during their work.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Medicine and Care of the Dying: A Modern History. Vol 1. (1st ed). Oxford: Oxford University Press; 2007.
- [Google Scholar]
- The Case Against Assisted Suicide: For the Right to End-of-life. USA: Care JHU Press; 2002.
- [Google Scholar]
- Hospice as a place of pastoral and palliative care over a badly ill person: Wyd. UKSW Warszawa 2012
- [Google Scholar]
- National Hospice and Palliative Care Organization (2006) Available from: http://www.nhpco.org/i4a/pages/index.cfm?pageid = 4648
- [Google Scholar]
- Last Rights: Rescuing the End of Life from the Medical System. USA: MacMillan; 2007.
- [Google Scholar]
- Care of the dying patient: The last hours or days of life. Br Med J. 2003;326:30-4.
- [Google Scholar]
- Nurses’ use of palliative care practices in the acute care setting. J Prof Nurs. 2001;17:14-22.
- [Google Scholar]
- The issue of death and dying: Employing problem-based learning in nursing education. Nurs Educ Today. 2002;22:319-29.
- [Google Scholar]
- Consequences of empowered CAN teams in nursing home settings: A longitudinal assessment. Gerontologist. 2007;47:323-38.
- [Google Scholar]
- Evaluation of an educational program for long-term care nursing assistants. J Am Med Dir Assoc. 2005;6:61-5.
- [Google Scholar]
- Physicians beliefs and attitudes about end-of-life care: A comparison of selected regions in Hungary and the United States. J Pain Symp Manage. 2010;39:76-87.
- [Google Scholar]
- Knowledge and perceptions of a domiciliary hospice service among general practitioners and community nurses. Br J Gen Pract. 1993;43:57-9.
- [Google Scholar]
- Paediatric nurses’ knowledge of palliative care in Florida: A quantitative study. Int J Palliat Nurs. 2009;15:432-9.
- [Google Scholar]
- Knowledge and attitudes to opioids in palliative care patients. Palliat Med. 2007;21:721-2.
- [Google Scholar]
- Nurses’ knowledge about palliative care: A cross-sectional survey. Indian J Palliat Care. 2012;18:122-7.
- [Google Scholar]
- Nurses’ attitudes and practice related to hospice care. J Nurs Scholarsh. 2003;35:249-55.
- [Google Scholar]
- Cardiac care units’ nursing staff points of view about developing hospice services in Iran for terminal cardiovascular patients: A qualitative study. Indian J Palliat Care 2014 In press
- [Google Scholar]
- Palliative care for older people – exploring the views of doctors and nurses from different fields in Germany. BMC Palliat Care. 2009;8:7.
- [Google Scholar]
- Interdisciplinary approaches to assisting with end-of-life care and decision making. Am Behav Sci. 2002;46:340-56.
- [Google Scholar]
- Measuring the success of the interdisciplinary team. Hospice Palliat Insights. 2003;4:47-9.
- [Google Scholar]
- Job satisfaction: How do social workers fare with other interdisciplinary team members in hospice settings? Omega. 2004;49:327-46.
- [Google Scholar]
- Hospice effect on government expenditures among nursing home residents. Health Serv Res. 2008;43:134-53.
- [Google Scholar]
- Government expenditures at the end of life for short- and long-stay nursing home residents: Differences by hospice enrollment status. J Am Geriatr Soc. 2004;52:1284-92.
- [Google Scholar]
- Hospice use and public expenditures at the end of life in assisted living residents in a Florida Medicaid waiver program. J Am Geriatr Soc. 2013;61:1777-81.
- [Google Scholar]
- Attitudes of patients, patients families, physicians, nurses, heath care administrators, insurer toward designing and delivering hospice care service in developing countries. Indian J Palliat Care 2014 In press
- [Google Scholar]
- Hospice enrollment and evaluation of its causal effect on hospitalization of dying nursing home patients. Health Serv Res. 2007;42:587-610.
- [Google Scholar]
- Experiences, knowledge, and opinions on palliative care among Romanian general practitioners. Croat Med J. 2006;47:142-7.
- [Google Scholar]
- Impact of hospice care on end-of-life hospitalization of elderly patients with lung cancer in Taiwan. J Chin Med Assoc. 2012;75:221-6.
- [Google Scholar]






