Translate this page into:
Analysis of Sociodemographic Parameters of Patients Admitted in a Newly Established Palliative Care Center in a Regional Cancer Institute of North-West India
Address for correspondence: Dr. Mukesh Kumar Singhal; E-mail: drmukeshsinghal78@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
After 4 months of the establishment of palliative care center (PCC) in our institute, we present an audit of the sociodemographic parameters of admitted patients. Such an audit can help to recognize the lacuna in the management and thus help to identify the specific requirements of cancer patients that might be overlooked in a busy cancer center.
Materials and Methods:
A total of 234 patients were admitted in our PCC since its inception in October 2013. The study design was retrospective, collecting the data from the medical records of the patients. The descriptive statistics of all these data were calculated in terms of frequencies and percentage of categorical variables.
Results:
Out of 234 patients admitted in PCC, 156 (66%) were male. The median age of the patients was 54 years. A total of 44% patients had primary malignancy of head and neck, 14% of cervical, 17% of lung cancer, 6% of breast, and 5% of colon, respectively. Metastatic disease was present in 76% of the patients admitted in the PCC. Liver was the most common (46%) metastatic site. Total 13 symptoms were identified with mean number of symptoms per patient at admission in PCC being 5.17.
Conclusions:
Palliative care services are an indispensable part of a tertiary regional cancer care center. The oncologists should be made aware of the requirement of better relief of pain and other distressing symptoms to provide better quality of life to the patients suffering from advanced cancer.
Keywords
North-West India
Palliative cancer center
Regional cancer center
Sociodemographic parameters
INTRODUCTION
There has been a great surge in both incidence and prevalence of cancer, especially in the context of developing countries. This may be ascribed to the changing lifestyle and an improvement in both the diagnostic and therapeutic health facilities. This has led to the prolongation of life expectancy, thereby more patients of geriatric age developing cancer leading to overall increase in the cancer incidence. The concept of palliative care is emerging and integrated palliative care aims to provide the best possible quality of life for the patients, the family, and the society at large. The palliative care is a multimodality approach that integrates the physical, psychosocial, emotional, and spiritual aspects of care with individualization of the needs of the patients. Palliative care provides effective relief from pain and other distressing symptoms without hastening or postponing death.[1] Only few dedicated palliative care center (PCC) are available in north-west India, our regional cancer center being one of them. After 4 months of establishment of PCC in our institute, we present an audit of the sociodemographic parameters of patients admitted in our PCC.[2] Such an audit can help to recognize the lacuna in the management and thus help to identify the specific requirements of cancer patients that might be overlooked in a busy cancer center. Also, by understanding the sociodemographic parameters of the patients attending a newly established PCC, the future policies of management strategies can be modified to suit the demands of such patients.
MATERIALS AND METHODS
A total of 234 patients were admitted in our PCC since its inception in October 2013. The study design was retrospective collecting the data from the medical records of the patients. The data entry in record sheet was done according to specific format, including all the important sociodemographic parameters and in-depth clinical history. The characterization of pain is done according to intensity, type, character, and radiation of pain. Because a large number of patients visiting our center belong to low socioeconomic status, the income group was also considered as an sociodemographic factor. The socioeconomic status was assessed by the modified BG Prasad classification. Because our regional cancer center is located in north west India, it serves a large population of states of Rajasthan, Haryana, and Punjab with occasional patients coming from far off places. The admission criterion in the PCC being all those patients in whom curative intent was not feasible and the target was to improve their quality of life. The patients are provided the medicines and palliative care free of cost. The PCC provides not only hospice care, but also the palliative treatments in ambulatory patients. A specialized pain clinic with free supply of oral morphine and trained nursing staff to take appropriate care for the patients is available in the setup. The descriptive statistics of all these data were calculated in terms of frequencies and percentage of categorical variables. Because the study was retrospective, ethics committee approval was not required as the patients were treated according to standard institutional protocol.
RESULTS
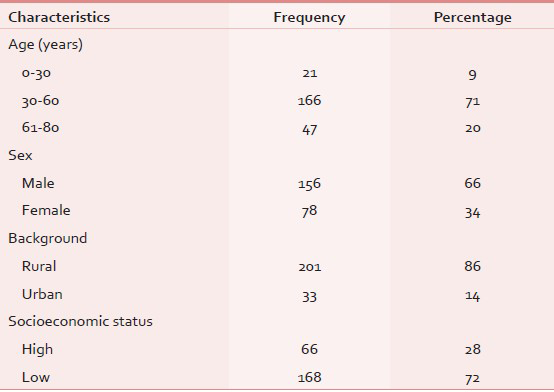
Out of 234 patients admitted in PCC, 156 (66%) were male. The median age of the patients was 54 years (range 22-78 years), 86% of the patients were from rural areas, and low socioeconomic status group patients comprised 72% of the cohort [Table 1]. A total of 44% patients had primary malignancy of head and neck, 14% cervix, 17% lung, 6% breast, and 5% colon [Table 2]. A total of 76% of the patients admitted in PCC had metastatic disease. Metastasis to the liver being the most common (46%); brain, lung, and bone metastasis constituted 13, 11, and 14%, respectively [Table 3]. Pain was present in 96% of patients at the time of admission in PCC. A total of 88% patients had fatigue (excessive lethargy) as one of the symptom complex. Altered bowel habits (diarrhea and/or constipation) were present in 68%; 32% patients had dysphagia, whereas nausea and vomiting were reported in 46 and 24% of the patients, respectively. Loss of appetite and insomnia were reported by a large number of patients (54 and 46%, respectively). Total 13 symptoms were identified with mean number of symptoms per patient at admission in PCC being 5.17 [Table 4].



As expected, pain was the most commonly reported symptom present in 96% of patients, most of the patients suffered from pain of moderate intensity (51%). Severe pain was recorded in 28%, whereas the rest had mild pain. Most of the patients (64%) having severe pain were suffering from head and neck cancer. 42% of patients had pain for more than 6 months duration of which 16% experienced radiation of pain. 78% of the patients admitted in PCC had received radiotherapy as a part of previous treatment, whereas 96% had received chemotherapy either as neoadjuvant, concurrent, or adjuvant treatment. Alternate system of medicine (Department of Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy (AYUSH)) was used by 23% of the patients prior to consulting the PCC.
DISCUSSION
In addition to the prescription of primary modalities of cancer treatment like chemotherapy and radiotherapy at a regional cancer center, there is always a requirement of a dedicated PCC to address the pain and other symptoms of advanced cancer. Establishment of such an unit can go a long way in providing better quality of life to a cancer patient by the multimodality approach. Ahmad et al., reported the need of similar palliative care services in a teaching hospital in Bangladesh.[3] Palliative care should be started from the day of starting of antineoplastic treatment in each and every patient of cancer. Fadare et al., reported the gaps in the knowledge of healthcare workers in the area of palliative care and stressed on the need to incorporate the study of palliative care in the curriculum of medical doctors and other healthcare workers at all levels.[4] Onyeka reported the requirement of good communication skills in the members of the multidisciplinary team who deal with palliative care.[5] Cancer is usually stamped as a death sentence, and the patients are highly vulnerable to suffer from the psychosocial impact of this dreadful disease as well.[67] Thus, efficient use of behavioral therapy and pharmacological intervention is necessary, especially in patient receiving palliative care.[8]
The male:female ratio of newly registered cancer patients in our regional cancer center in the last decade is 1.24:1, whereas this ratio was 1.9:1 for the patients admitted at the PCC. This gender disparity between incidence of cancer and attendance at PCC might point toward the poor care of female still prevalent in our society, especially in rural areas. The range of age of patients receiving palliative care is wide, implying that patient of every age group may require palliative care.[910] We observed that the patients presented with a wide range of symptoms with pain being present in most of them, 28% having severe pain. This may be explained in terms of pain being primary symptom with other symptoms being added progressively as a patient shifts from curable to noncurable disease.[11] Breuer et al., conducted a nationwide survey and concluded that limitations in oncologists’ knowledge and practices relating to pain management may be contributing to a substantial unmet need in populations with cancer.[12] Also, the psychiatric comorbidity is often overlooked by the treating oncologist leading to development of complex myriad of symptoms that may worsen quality of life.[11] Because pain is present in nearly all the patients eligible for palliative care, a PCC should be well equipped with a trained pain clinic to target pain by both medical and surgical approaches. After pain, fatigue was the second most common complaint in our patient cohort. This is similar to multicenter studies by Ho et al.[13] and Vainio et al.[14]
Though symptoms of depression were present in most of the patients receiving palliative care, professional psychological assessment was not possible for every patient admitted in our PCC. A better psychosocial support system is required to effectively manage this comorbidity. Most of patients had pain, fatigue, altered bowel habits, insomnia, and loss of appetite.[15] Also, we found that 23% of the patients resorted to alternate system of medicine before being admitted in our PCC. This may point to the lack of awareness for providing symptomatic relief to the cancer patient by the primary oncologists. The barriers to pain and palliative management remain to be almost exactly the same as 20-years ago: Poor assessment by the physician, reluctance to prescribe/take opioid analgesics, and reluctance on the part of the patient to report pain. Such barriers can be crossed with proper training of oncologists to improve communication skills and symptomology management. Also, this study identifies the major symptoms in a patient eligible for palliative care, which may help the physicians to concentrate and carefully address these often overlooked symptoms.
Limitations of the study
The diverse patient populations with different cancer type and being a retrospective analysis, it is difficult to draw a direct conclusion on the data of palliative care in our settings. Prospective studies with outcome data on larger number of patients may help in the establishment of better conclusive findings. However, such assessments are necessary to give impetus to the improvement of palliative care in a newly established set up.
CONCLUSIONS
Palliative care services are an indispensable part of a tertiary regional cancer care center. The oncologists should be made aware of the requirement of better relief of pain and other distressing symptoms to provide better quality of life to the patients suffering from advanced cancer. We stress on the need of development of a better overall care addressing not only the cancer but also improved patient symptom management.
ACKNOWLEDGMENTS
The first two authors contributed equally to the manuscript. The authors would like to thank consultants in Department of Oncology, Dr. Ajay Sharma, Dr. N Sharma, Dr. S L Jakhar, and Dr. S Beniwal. Also, they express gratitude to postgraduate (PG) students of the department: Dr. Satyanarayan, Dr. Sitaram, Dr. Guman Singh, Dr. Murali, Dr. Tanya, Dr. Rajesh, and Dr. R Purohit.
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- Principles of Palliative Care. In: Varghese C, ed. Manual for palliative care (1st ed). New Delhi: Directorate General of Health Services Ministry Of Health And Family Welfare; 2005.
- [Google Scholar]
- Palliative care in developing countries: What are the important issues? Palliat Med. 2007;21:173-5.
- [Google Scholar]
- Palliative care outpatient consultation service in a teaching hospital in Bangladesh. Mymensingh Med J. 2011;20:98-103.
- [Google Scholar]
- Healthcare workers knowledge and attitude toward palliative care in an emerging tertiary centre in South-West Nigeria. Indian J Palliat Care. 2014;20:1-5.
- [Google Scholar]
- Psychosocial issues in palliative care: A review of five cases. Indian J Palliat Care. 2010;16:123-8.
- [Google Scholar]
- Factors that influence cancer patients’ anxiety following a medical consultation: Impact of a communication skills training programme for physicians. Ann Oncol. 2006;17:1450-8.
- [Google Scholar]
- Patient evaluation and outcome measures, the measurement of pain and other symptoms. In: Doyle D, ed. Oxford Textbook of Palliative Medicine (3rd ed). New York: Oxford University Press; 2007.
- [Google Scholar]
- Anxiety disorders in cancer patients: Their nature, associations and relations to quality of life. J Clin Oncol. 2002;20:3137-48.
- [Google Scholar]
- Palliative care team: The first year audit in Japan. J Pain Symptom Manage. 2005;29:458-65.
- [Google Scholar]
- Needs of terminally ill patients and their families: An experience with fifty three patients attending a newly organized palliative care service in Bangladesh. J BSA. 2006;19:38-43.
- [Google Scholar]
- Medical Oncologists’ attitudes and practice in cancer pain management: A national survey. J Clin Oncol. 2011;29:4769-75.
- [Google Scholar]
- Experiences and attitudes of patients with terminal cancer and their family caregivers toward the disclosure of terminal illness. J Clin Oncol. 2010;28:1950-7.
- [Google Scholar]
- Prevalence of symptoms among patients with advanced cancer: An international collaborative study. Symptom Prevalence Group. J Pain Symptom Manage. 1996;12:3-10.
- [Google Scholar]
- Multidisciplinary symptom control clinic in a cancer center: A retrospective study. Support Care Cancer. 2001;9:162-8.
- [Google Scholar]






