Translate this page into:
Preferred and Actual Places of Death Among Patients with Advanced Cancer: A Single-centre Cohort Study in Japan
*Corresponding author: Yusuke Hiratsuka, Department of Palliative Medicine, Tohoku University School of Medicine, Sendai, Japan. hiratsuka.med.t@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ikari T, Hiratsuka Y, Oishi T, Miyashita M, Morita T, Mack J, et al. Preferred and Actual Places of Death Among Patients with Advanced Cancer: A Single-centre Cohort Study in Japan. Indian J Palliat Care 2024;30:268-74. doi: 10.25259/IJPC_133_2024
Abstract
Objectives:
Achieving a ‘good death’ is one of the important goals of palliative care. Providing goal-concordant care and an environment tailored to the patient’s preferences can contribute to a ‘good death’. However, the concordance rate between the preferred and actual places of death among advanced cancer patients in Japan is less explored. This study aimed to identify the concordance between patients’ preferred and actual places of death and the associated factors among patients with advanced cancer in Japan.
Materials and Methods:
Patients with advanced cancer who underwent chemotherapy at Tohoku University Hospital between January 2015 and January 2016 were enrolled and followed up for 5 years. The enrolled patients were asked about their preference for their place of death. The response options were: “Own home,” “General ward” and “Palliative care unit (PCU).” We compared the actual place of death with the patient’s preference through a follow-up review of the medical records.
Results:
A total of 157 patients with advanced cancer were enrolled between January 2015 and January 2016. Of these patients, 22.9% (11/48) died at home according to their preference, 64.0% (16/25) in the general ward and 37.9% (11/29) in the PCU. Only thirty-seven (37.3%) patients died where they wanted, based on the comparison between patients’ preferences and actual places of death.
Conclusion:
The concordance rate between the preferred and actual places of death is not high in Japan. Improving concordance between patients’ preferences and actual places of death has the potential to improve end-of-life care.
Keywords
Advanced cancer
Preferred place of death
Actual place of death
End-of-life discussion
Chemotherapy
INTRODUCTION
Achieving ‘good death’ is one of the important goals of palliative care.[1] It has been shown that providing goal-concordant care and an environment tailored to the patient’s preferences was associated with the patient’s ‘good death’.[1-3] In previous studies, the concordance rate between the preferred and the actual places of death for advanced cancer patients ranged from 60.2% to 67.1%.[4-6]
In previous studies, several factors have been identified as factors associated with death in a preferred place: Patients providing their opinions regarding where they wanted to die,[4,6,7] patient-caregiver agreement on the preferred place of death,[4] presence of a caregiver[6-8] and the presence of social support for caregivers.[4] In Japan, one study conducted in 2001 compared the preference with the actual place of death for patients who received home hospice care.[9] Few studies in Japan have investigated the factors associated with patients dying in their preferred place despite potential variations in preferred places of death based on cultural background.[10]
In addition, these studies were conducted before 2011, but systemic anti-cancer treatment options have changed drastically since then.[11] Hence, the factors associated with patients dying in their preferred place may have changed owing to changes in the sense of values, social environment and medical system prompted by changes in systemic anti-cancer treatment.[12]
This study aimed to (1) identify the concordance rate between patients’ preferred and actual place of death and (2) investigate the factors associated with the concordance of patients with advanced cancer in Japan. We hypothesised that this study would provide fundamental data for future palliative care programmes by identifying the actual places of death of patients with advanced cancer, along with the factors associated with their ability to die in their preferred places.
MATERIALS AND METHODS
Study design
This study was a follow-up of a previous cross-sectional study conducted at a single centre in Japan. The parent study investigated the association between physician communication and prognostic awareness in patients with unresectable/recurrent solid cancers.[13,14] During the recruitment phase of the parent study, the researcher in charge relocated to another hospital, which limited our ability to reach the target sample size of 250. Patients with advanced cancer who underwent chemotherapy at Tohoku University Hospital between January 2015 and January 2016 were enrolled and followed up for 5 years.
Patients included in the study were aged ≥20 years, had unresectable/recurrent solid cancer or had failed first-line chemotherapy. The following exclusion criteria were applied: (1) unwillingness to provide written informed consent, (2) cognitive impairment, (3) unconfirmed lesions by imaging, (4) lack of awareness of the diagnosis, (5) inability to understand or complete a questionnaire in Japanese and (6) unsuitability to participate in the opinion of the primary attending physician. Eligibility was initially evaluated using the medical records. The primary attending physician, defined as the medical oncologist who examined the patient most frequently, was consulted to confirm eligibility and allow the researcher to contact the patient.
Both inpatients and outpatients were eligible for enrolment in the study. The limited number of available researchers necessitated the enrolment of patients by convenience to some extent; potentially eligible patients were sometimes excluded if several were identified on the same day or for other practical reasons. The primary attending physician obtained informed consent from each patient.
Collection of data
The enrolled patients were surveyed using a questionnaire developed specifically for the study and were required to complete and return the questionnaire to our office within 2 weeks of enrolment. We developed the questionnaire based on three previous reports[15-17] and included questions that had been used in prospective longitudinal studies in the United States[15,18,19] after applying the back-translation method. First, the principal investigators examined the validity of the professionally translated Japanese statements. Second, the revised translations were sent back to the translator for retranslation into English. Finally, we confirmed the uniformity of the questions with two authors of the three previous papers.[15,18,19]
Information on the following items was sought in the patient survey: Preference for treatment (prolongation of life or palliation), hopes for participating in a clinical trial, preference for place of death, whether they had an end-of-life discussion, awareness of their terminal status (understanding of how unlikely it was that their cancer would be cured),[19] desire for prognostic information, the potential for cure (how likely patients thought chemotherapy would cure their cancer),[17] understanding of the purpose of chemotherapy, understanding of physicians’ goals when administering chemotherapy,[19] characterisation of communication with physicians, score on the Patient Health Questionnaire (PHQ)-9, which has been validated in Japan[20] as a screening tool for depression, the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC-QLQ-C30), which has been validated in Japan[21] to assess the quality of life.
End-of-life discussion was defined as a discussion on palliative care or a do-not-attempt-resuscitate order. We used the commonly accepted definition of palliative care,[1,22] specifically (1) an approach that improves the quality of life for patients and their families facing the problems associated with life-threatening illness; (2) treatment of pain and other problems, which may be physical, psychosocial or spiritual and (3) care provided in the patient’s own home or a palliative care unit (PCU).
We calculated a summary score for communication with the primary attending physician[23] by asking patients five questions; ‘How often did your doctors listen carefully to you?’ ‘How often did your doctors explain things in a way you could understand?’ ‘How often did your doctors give you as much information as you wanted about your cancer treatments, including potential benefits and side effects?’ ‘How often did your doctors encourage you to ask all the cancer-related questions you had?’ and ‘How often did your doctors treat you with courtesy and respect?’ The response options for each question were ‘Always’ (score 3), ‘Usually’ (score 2), ‘Sometimes’ (score 1) and ‘Never’ (score 0). We then calculated the total score, with 0 being the worst possible total score and 15 being the best. The PHQ-9 scores were calculated based on a previous study and ranged from 0 to 27 points. The EORTC-QLQ-C30 scores were transformed into a 0–100-point scale according to the scoring manual.[24]
We also obtained baseline patient data from the medical records, including age, sex, primary cancer site, Eastern Cooperative Oncology Group performance status, employment status, marital status, highest education level and number of family members living at home. Actual survival time was calculated by reviewing medical records after a follow-up period of 5 years from enrolment, where the date of enrolment was subtracted from the date of death. Patients who were alive at the final follow-up were censored. We also obtained information from physicians regarding whether they discussed the patient’s preference for place of death with the patients or their families. The physicians were asked two questions: ‘Did you discuss the preferred place of death with your patient?’ and ‘Did you discuss the preferred place of death with your patient’s family?’ The response options included ‘explained that we should discuss your preferred place of death’, ‘explained that there are death places such as general wards, hospices and your own home’, ‘explained specifically about your preference for death place’ and ‘did not explain’. For analysis, we categorised patients whose physicians answered ‘explained that we should discuss your preference for death place’ or ‘explained that there are death places such as general wards, hospices and your own home’ or ‘explained specifically about your preference for death place’ as an ‘explained group’ and those whose physicians answered ‘did not explain’ were classified as a ‘not explained group’.
Preference for place of death
We asked the enrolled patients the following question about their preference for place of death: ‘Where would you like to spend your end of life?’ The response options were ‘own home,’ ‘general ward’ and ‘palliative care unit’
In addition, we compared each patient’s preferred and actual place of death through a follow-up review of their medical records.
Statistical analysis
First, we performed descriptive analyses to summarise baseline characteristics. Second, we compared patients preferred and actual places of death. If a patient’s preference and actual place of death were in the same category, we termed their result concordant. If a patient’s preference and actual place of death were in different categories, the result was deemed to be non-concordant. Third, we performed Wilcoxon rank-sum tests for continuous variables, Cochran– Armitage trend tests for ordinal variables and Fisher’s exact tests for categorical variables to identify the factors associated with concordance. Statistical significance was set at P < 0.05 as statistically significant. All the statistical analyses were performed using JMP version 16 for Windows (SAS Institute Inc., Cary, NC, USA).
Ethics statement
The study met the ethical guidelines for medical and health research involving human subjects outlined by the Ministry of Health, Labour and Welfare in Japan and was conducted in accordance with the ethical standards of the Declaration of Helsinki. The primary attending physicians obtained written informed consent from all patients. The study was approved by the independent ethics committee of Tohoku University School of Medicine (approval no. 2016-1-689).
RESULTS
Patient characteristics
In total, 157 patients with advanced cancer were enrolled between January 2015 and January 2016 [Table 1]. After a follow-up period of 5 years, 10 patients were still alive, 135 had died, and 12 were lost to follow-up. There was missing data regarding the preference for place of death for 33 patients.
| Characteristics | n(%) |
|---|---|
| Age, years (mean±SD) | 63.9±12.3 |
| Gender | |
| Male | 64 (62.7) |
| Female | 38 (37.3) |
| Primary cancer site | |
| Gastrointestinal | 48 (47.1) |
| Lung | 11 (10.8) |
| Hepatobiliary pancreatic | 12 (11.8) |
| Sarcoma | 12 (11.8) |
| Breast | 4 (3.9) |
| Head and neck | 2 (2.0) |
| Others | 13 (12.7) |
| ECOG PS* | |
| 0 | 29 (28.7) |
| 1 | 55 (54.5) |
| 2 | 13 (12.9) |
| 3 | 4 (4.0) |
| Employment status** | |
| Employed | 23 (23.0) |
| Non-employment | 77 (77.0) |
| Marital status* | |
| Married or living with partner | 81 (80.2) |
| Unmarried | 20 (19.8) |
| Highest level of education* | |
| Not to high school | 11 (10.9) |
| High school or some college | 69 (68.3) |
| College or higher degree | 21 (20.8) |
| Living with family | |
| Yes | 86 (84.3) |
| No | 16 (15.7) |
| Median survival time (days, range)*** | 273 (18–1731) |
Finally, data for 102 patients who died during the follow-up period were available for analysis [Figure 1]. The study group consisted of 64 men (62.7%) and 38 women (37.3%) with a mean age of 63.9 years (standard deviation, 12.3). The primary cancer sites were the gastrointestinal (47.1%), hepatobiliary pancreas (11.8%) and sarcoma (11.8%). The median survival time was 273 days (range: 18–1,731).
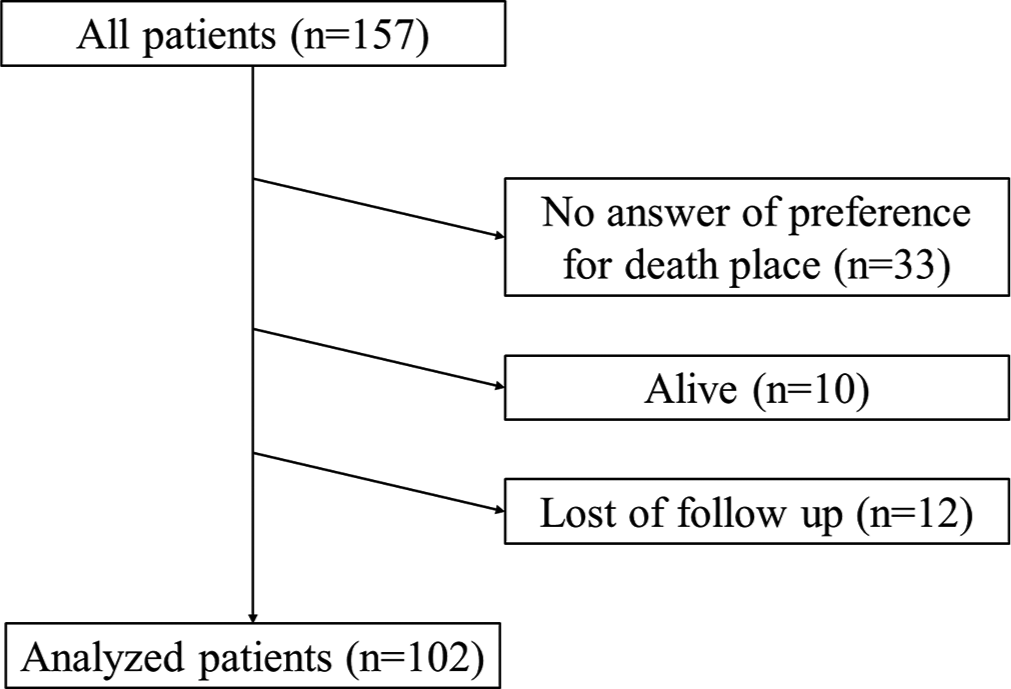
- Flow chart outlining participant selection.
Preference of death place and actual death place
Table 2 shows the patients’ preferred and actual place of death in the study population. Forty-eight patients (47.1%) answered ‘Own home,’ 25 (24.5%) answered ‘General ward’ and 29 (28.4%) answered ‘Palliative care unit’. Regarding the place of death, 17 (16.7%) patients died in their homes, 55 (53.9%) in general wards and 30 (29.4%) in PCUs. As for the comparison between patients’ preference for death place and actual death place, 37.3% of patients died at the place they wanted.
| Actual | ||||
|---|---|---|---|---|
| Answer | Home (%) | Hospital (%) | Palliative care unit (%) | Total (%) |
| Preference | ||||
| Home | 11 (10.8) | 25 (24.5) | 12 (11.8) | 48 (47.1) |
| Hospital | 2 (2.0) | 16 (15.7) | 7 (6.9) | 25 (24.5) |
| Palliative care unit | 4 (23.5) | 14 (13.7) | 11 (10.8) | 29 (28.4) |
| Total | 17 (16.7) | 55 (53.9) | 30 (29.4) | 102 |
κ=0.11. κ=Kappa coefficient. The kappa coefficient indicates the extent of the concordance between patients’ preference and the actual place of death.
Table 3 shows the factors associated with the concordance between patients’ preferences and the actual place of death. No significant factors were identified in the univariate analysis. Meanwhile, understanding physicians’ goals of chemotherapy (P = 0.10) and discussions regarding patients’ preference for the place of death with patients (P = 0.17) and their families (P = 0.11) had a weak association with the concordance.
| Variable | Achievement (n=38) | Non-achievement (n=64) | P-value |
|---|---|---|---|
| Age, years (mean±SD) | 65.3±10.2 | 63.0±13.3 | 0.65 |
| Sex | |||
| Male | 23 (35.9) | 41 (64.1) | 0.83 |
| Female | 15 (39.5) | 23 (60.5) | |
| ECOG PS | |||
| 0 | 11 (37.9) | 18 (62.1) | 1.00 |
| 1 | 20 (36.4) | 35 (63.6) | |
| 2 | 6 (46.2) | 7 (53.9) | |
| 3 | 1 (25.0) | 3 (75.0) | |
| Employment status | |||
| Employed | 10 (43.5) | 13 (56.5) | 0.63 |
| Non-employed | 28 (36.4) | 49 (63.6) | |
| Marital status | |||
| Married or partner | 28 (34.6) | 53 (65.4) | 0.21 |
| Unmarried | 10 (50.0) | 10 (50.0) | |
| Highest education level | |||
| Not to high school | 5 (45.5) | 6 (54.6) | 0.54 |
| High school or some college | 25 (36.2) | 44 (63.8) | |
| College degree or higher | 7 (33.3) | 14 (66.7) | |
| Living with family | |||
| Yes | 31 (36.1) | 55 (64.0) | 0.58 |
| No | 7 (43.8) | 9 (56.3) | |
| Global health status (EORTC-QLQ-C30) (mean±SD) | 59.4±22.9 | 53.8±23.2 | 0.15 |
| Summary score (EORTC-QLQ-C30) (mean±SD) | 73.4±15.5 | 71.1±16.5 | 0.54 |
| Patient Health Questionnaire-9 (mean±SD) | 5.9±4.4 | 9.3±15.1 | 0.40 |
| Preference for treatment | |||
| Prolongation of life | 14 (34.2) | 27 (65.9) | 0.67 |
| Palliation | 23 (39.7) | 35 (60.3) | |
| Hope for participation in a clinical trial | |||
| Yes | 25 (34.3) | 48 (65.8) | 0.35 |
| No | 12 (46.2) | 14 (53.9) | |
| End-of-life discussion about palliative care | |||
| Yes | 10 (37.0) | 17 (63.0) | 1.00 |
| No | 28 (37.8) | 46 (62.2) | |
| End-of-life discussion about do-not-attempt resuscitation | |||
| Yes | 18 (38.3) | 29 (61.7) | 1.00 |
| No | 20 (36.4) | 35 (63.6) | |
| Awareness of terminal status | |||
| Yes | 13 (41.9) | 18 (58.1) | 1.00 |
| No | 11 (39.3) | 17 (60.7) | |
| Desire for prognostic information | |||
| Yes | 27 (38.6) | 43 (61.4) | 1.00 |
| No | 11 (36.7) | 19 (63.3) | |
| Potential for cure | |||
| Impossible | 14 (36.8) | 24 (63.2) | 0.81 |
| Possible | 15 (41.7) | 21 (58.3) | |
| Understanding of purpose of chemotherapy | |||
| Cure | 3 (25.0) | 9 (75.0) | 0.49 |
| Prolong life | 27 (38.6) | 43 (61.4) | |
| Palliation | 8 (47.1) | 9 (52.9) | |
| Understanding of physicians’ goals of chemotherapy | |||
| Cure | 0 (0) | 7 (100.0) | 0.10 |
| Prolong life | 25 (40.3) | 37 (59.7) | |
| Palliation | 8 (34.8) | 15 (65.2) | |
| Discussion about patient’s preference for death place with patient | |||
| Yes | 6 (60.0) | 4 (40.0) | 0.17 |
| No | 32 (35.2) | 59 (64.8) | |
| Discussion about patient’s preference for death place with family | |||
| Yes | 10 (55.6) | 8 (44.4) | 0.11 |
| No | 28 (33.7) | 55 (66.3) | |
| Communication score (mean±SD) | 7.9±3.5 | 7.7±2.6 | 0.73 |
ECOG: Eastern Cooperative Oncology Group, PS: Performance status, EORTC-QLQ-C30: European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30, SD: Standard deviation
DISCUSSION
This is the first study in Japan to compare the concordance rate between preferred and actual places of death for patients receiving cancer therapy, and the concordance rate was 37.3%. While no significant variables were not statistically associated with the concordance between the patients’ preferences and the actual places of death, understanding physicians’ goals of chemotherapy, discussions about patient’s preference for death place with patient and their family had weak association with concordance.
The present study indicated a lower concordance rate than those reported in previous studies.[4-6] In particular, this study revealed that the concordance rate for death at home was 22.9% (11/48), which is lower than 59.5–88.5% in those results.[4-6] Similarly, the concordance rate for death at PCU was 37.9% (11/29), which is lower than 50.0–90.0% in another report.[5,25] On the other hand, the number of patients who preferred to die in the general ward was 25 (24.5%), while the number of those who actually died in the general ward increased to 55 (53.9%). These suggested that patients who preferred to die at home or in the PCU may have died in the general ward.
Compared to Europe and America, the time for end-of-life discussions between medical staff and patients and their families is often delayed in Japan.[26,27] Delays in end-of-life discussions may be associated with an increased proportion of patients dying in the general ward. The Ministry of Health, Labour and Welfare in Japan has been promoting educational activities for healthcare providers by holding a workshop, ‘Education For Implementing End-of-Life Discussion’, since 2016 to improve the decision-making process at the end of life.[28] As this activity becomes more prevalent and more medical staff are educated, the concordance rate between the preferred and actual places of death might also increase.
We assumed that the insufficient number of general practitioners (GPs) might have affected our results. It has been shown that the percentage of people who are in the preferred place increases when GPs provide palliative care.[29] It has been revealed the uneven distribution of GPs in Japan[30] and the insufficient number of GPs in Japanese provincial cities.[31] Patients may be more likely to die in their preferred places by ensuring that GPs are appropriately located in urban and rural areas and developing specialised educational programmes that enable GPs to provide palliative care.
This study identified several factors that were weakly associated with concordance. We assumed that patients who understood the goals of chemotherapy in this study might have accurate prognostic awareness, which allowed them to select the preferred place of death based on their own prognosis.[32] Discussions with the patients in this study may have triggered the patients to consider the place of their own death and may have led them to provide their own opinions. Discussion with the family in this study may have also triggered the family to consider the patient’s preferred place and match with that of the family.
This study had several limitations. First, it was performed at a university hospital in Japan, which may have affected the generalisability of the results to other regions of Japan or other countries. Nevertheless, the study’s findings are consistent with a series of national surveys conducted by the Ministry of Health, Labour and Welfare, which reported that almost half of the respondents wanted to die at home.[33] Second, the preferred place of death may change or may have preferred more than one place during the treatment process because of the longer follow-up period of 5 years in the current study compared with 1–3 years in previous studies.[4-6] In contrast, a systematic review by Gomes et al.[34] revealed that 80% of the patients had no change in their preferred places of death. Further studies are needed to determine the relationship between duration of care and change in the preferred place of death. Third, the study relied on patient and physician reports of previous communication, which may be subject to recall bias. Fourth, our use of a convenience sample, along with the fact that physicians were asked to approach their own patients about participating in the study, might have introduced a degree of selection bias. In addition, the lack of information on the number of patients treated at the institution who were asked to participate and the final number who participated in the parent study might have affected the degree of selection bias. Finally, unmeasured factors, such as physicians’ communication styles, may have influenced patients’ preferred places of death, highlighting the need for further research in this area.
CONCLUSION
The concordance rate between preferred and actual places of death was not high in this study. This study highlights the need for further research to identify factors associated with the gap between patients’ preferences and actual places of death and to develop interventions to increase concordance rates. It may be necessary for medical staff to explain the condition to the patient at the appropriate time and to begin advance care planning early so that the patient can die in the preferred place.
Acknowledgments
We are grateful to Editage (www.editage.co.kr) for proofreading the manuscript to ensure grammar and clarity. We thank Inga T. Lennes, MD, MPH, at Massachusetts General Hospital Cancer Center, Boston, MA, USA for assisting with the backtranslation of the questions used in this survey. We are also deeply grateful to Mrs. Yamagishi, RN, of the Department of Palliative Nursing, Tohoku University Graduate School of Medicine, Miyagi, Japan for participant recruitment and data collection.
Ethical approval
The research/study was approved by the Institutional Review Board at the independent ethics committee of Tohoku University School of Medicine, number Approval no. 2016-1-689, dated January 2016.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
A JSPS KAKENHI [Grant Numbers 15K15161,18K10266].
References
- Good Death Inventory: A Measure for Evaluating Good Death from the Bereaved Family Member's Perspective. J Pain Symptom Manage. 2008;35:486-98.
- [CrossRef] [PubMed] [Google Scholar]
- Good Death in Cancer Care: A Nationwide Quantitative Study. Ann Oncol. 2007;18:1090-7.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Associated with Good Death of Patients with Advanced Cancer: A Prospective Study in Japan. Support Care Cancer. 2022;30:9577-86.
- [CrossRef] [PubMed] [Google Scholar]
- Can this Patient Be Discharged Home? Factors Associated with at-Home Death among Patients with Cancer. J Clin Oncol. 2011;29:1159-67.
- [CrossRef] [PubMed] [Google Scholar]
- Actual and Preferred Place Of Death of Cancer Patients. Results from the Italian Survey of the Dying of Cancer (ISDOC) J Epidemiol Community Health. 2006;60:412-6.
- [CrossRef] [PubMed] [Google Scholar]
- Which Hospice Patients with Cancer are Able to Die in the Setting of Their Choice? Results of a Retrospective Cohort Study. J Clin Oncol. 2012;30:2783-7.
- [CrossRef] [PubMed] [Google Scholar]
- The Interaction of Socioeconomic Status with Place of Death: A Qualitative Analysis of Physician Experiences. BMC Palliat Care. 2018;17:87.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Influencing Death at Home in Terminally Ill Patients with Cancer: Systematic Review. BMJ. 2006;332:515-21.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of the Place of Death among Terminally Ill Cancer Patients Under Home Hospice Care in Japan. Palliat Med. 2003;17:445-53.
- [CrossRef] [PubMed] [Google Scholar]
- Does Place of Death from Cancer Vary between Ethnic Groups in South East England? Palliat Med. 2011;25:314-22.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Challenges of Immune Checkpoint Inhibitors. Cancer Cell. 2020;38:326-33.
- [CrossRef] [PubMed] [Google Scholar]
- International Study of the Place of Death of People with Cancer: A Population-Level Comparison of 14 Countries Across 4 Continents Using Death Certificate Data. Br J Cancer. 2015;113:1397-404.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Perceptions of Curability and Physician-reported Disclosures of Incurability in Japanese Patients with Unresectable/Recurrent Cancer: A Cross-sectional Survey. Jpn J Clin Oncol. 2018;48:913-9.
- [CrossRef] [PubMed] [Google Scholar]
- Patients' Understanding of Communication about Palliative Care and Health Condition in Japanese Patients with Unresectable or Recurrent Cancer: A Cross-sectional Survey. Ann Palliat Med. 2021;10:2650-61.
- [CrossRef] [PubMed] [Google Scholar]
- Associations between End-of-life Discussion Characteristics and Care Received Near Death: A Prospective Cohort Study. J Clin Oncol. 2012;30:4387-95.
- [CrossRef] [PubMed] [Google Scholar]
- Patient Beliefs that Chemotherapy May Be Curative and Care Received at the End of Life among Patients with Metastatic Lung and Colorectal Cancer. Cancer. 2015;121:1891-7.
- [CrossRef] [PubMed] [Google Scholar]
- Patients' Expectations about Effects of Chemotherapy for Advanced Cancer. N Engl J Med. 2012;367:1616-25.
- [CrossRef] [PubMed] [Google Scholar]
- End-of-life Discussions, Goal Attainment, and Distress at the End of Life: Predictors and Outcomes of Receipt of Care Consistent with Preferences. J Clin Oncol. 2010;28:1203-8.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of Newly Diagnosed Cancer Patients' Understanding of the Goals of Their Care at Initiation of Chemotherapy. Cancer. 2013;119:691-9.
- [CrossRef] [PubMed] [Google Scholar]
- Performance of the Japanese Version of the Patient Health Questionnaire-9 (J-PHQ-9) for Depression in Primary Care. Gen Hosp Psychiatry. 2018;52:64-9.
- [CrossRef] [PubMed] [Google Scholar]
- A Cross-validation of the European Organization for Research and Treatment of Cancer QLQ-C30 (EORTC QLQ-C30) for Japanese with Lung Cancer. Eur J Cancer. 1998;34:810-5.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of Prognostic Disclosure: Associations with Prognostic Understanding, Distress, and Relationship with Physician among Patients with Advanced Cancer. J Clin Oncol. 2015;33:3809-16.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of Patient-oncologist Prognostic Discordance in Advanced Cancer. JAMA Oncol. 2016;2:1421-6.
- [CrossRef] [PubMed] [Google Scholar]
- The EORTC QLQ-C30 Scoring Manual Brussels: European Organisation for Research and Treatment of Cancer; 2001.
- [Google Scholar]
- Determinants of Congruence between the Preferred and Actual Place of Death for Terminally Ill Cancer Patients. J Palliat Care. 2003;19:230-7.
- [CrossRef] [Google Scholar]
- Palliative Care Physicians' Practices and Attitudes Regarding Advance Care Planning in Palliative Care Units in Japan: A Nationwide Survey. Am J Hosp Palliat Care. 2014;31:699-709.
- [CrossRef] [PubMed] [Google Scholar]
- Survey of the General Public's Attitudes Toward Advance Directives in Japan: How to Respect Patients' Preferences. BMC Med Ethics. 2006;7:E11.
- [CrossRef] [PubMed] [Google Scholar]
- Cabinet Office. Available from: https://www5.cao.go.jp/keizai-shimon/kaigi/special/reform/wg1/281027/shiryou1-1-2.pdf [Last accessed on 2024 May 15]
- [Google Scholar]
- Actual and Preferred Place of Death of Home-Dwelling Patients in Four European Countries: Making Sense of Quality Indicators. PLoS One. 2014;9:e93762.
- [CrossRef] [PubMed] [Google Scholar]
- A Study on Gaps in the Access to Home-based Medical Care by Residents According to Medical Clinic Distributions by Prefecture. J Japan Soc Healthc Admin. 2014;105:5. (In Japanese)
- [Google Scholar]
- Geographical Distribution of Family Physicians in Japan: A Nationwide Cross-sectional Study. BMC Fam Pract. 2019;20:147.
- [CrossRef] [PubMed] [Google Scholar]
- Is the 1-day Surprise Question a Useful Screening Tool for Predicting Prognosis in Patients with Advanced Cancer?-a Multicenter Prospective Observational Study. Ann Palliat Med. 2021;10:11278-87.
- [CrossRef] [PubMed] [Google Scholar]
- Labor, and Welfare. Available from: https://www.mhlw.go.jp/toukei/list/dl/saisyuiryo_a_h29.pdf [Last accessed on 2024 May 15]
- [Google Scholar]
- Heterogeneity and Changes in Preferences for Dying at Home: A Systematic Review. BMC Palliat Care. 2013;12:7.
- [CrossRef] [PubMed] [Google Scholar]







