Translate this page into:
A Questionnaire-based Survey on Challenges Faced and Strategies Adopted by Pain and Palliative Care Physicians Working in Oncology Setup During Novel COVID-19 Pandemic – A Descriptive Cross-sectional Study

*Corresponding author: Seema Mishra, Department of Oncoanaesthesia and Palliative Medicine, Dr B.R.A., Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi, India. seemamishra2003@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta R, Mishra S, Bhatnagar S, Bharati SJ, Garg R, Kumar V, et al. A questionnaire-based survey on challenges faced and strategies adopted by pain and palliative care physicians working in oncology setup during novel COVID-19 pandemic – A descriptive cross-sectional study. Indian J Palliat Care 2021;27(2):319-29.
Abstract
Objectives:
Novel coronavirus (COVID-19) pandemic has brought to the fore various challenges faced by pain and palliative care physicians working in oncology setup all over the country. Cancer care has been afflicted a lot during the pandemic, with challenges faced by patients and their caregivers as well as the healthcare workers. The questionnaire based online survey was conducted to explore the personal challenges faced, strategies adopted and to compare the challenges between different oncology setups.
Materials and Methods:
After obtaining institutional ethical clearance the online questionnaire prepared through Google forms was rolled out to pain and palliative care physicians working all over the country with the help of social media platforms. The results were expressed in absolute number, percentage and comparisons were made with the help of Fisher’s exact test.
Results:
Maximum challenges faced were the fear of carrying infection back home (91%), the possibility of attending to a COVID positive case in day to day clinical practice because of inadequate space and screening (62%) and limited services provided by NGO’s during pandemic (71%). Strategies commonly adopted were the provision of necessary personal protective equipment (83%), the conduct of educational sessions for the task force members (67%), maximum utilization of available space in the hospital (85%) and stockpiling of necessary medications and equipment (75%).
Conclusion:
It is the need of the hour to formulate strong and effective strategies to overcome the challenges encountered by pain and palliative care physicians so that we are equipped in the future to deal with any kind of pandemics.
Keywords
Challenges
COVID-19 pandemic
Pain and palliative care physicians
Strategies
INTRODUCTION
The COVID-19 pandemic hit most healthcare providers globally in a way they did not anticipate. It has also resulted in economic, social and political devastation rapidly becoming an international public health crisis.[1] The WHO declared the disease as pandemic on 12th March 2020 and urged countries to limit its spread.[2] In India also the count is rising steadily, experts believe that India is currently in the stage of limited community transmission, which is expected to progress over the next few months. The older patients and those with underlying serious health conditions, for example, cancer, have an increased risk of admissions into intensive care units[3] the estimated case fatality rate in cancer patients with COVID-19 is 6%,[4] as compared to 1% among the general population.[5] With the estimated number of cancer cases in India being approximately 2.25 million the impact of this pandemic on cancer patients will be grave affecting both survival as well as quality of life.[6] Palliative care with its holistic approach, the motto of giving realistic hope and honest opinion, focus on symptom management (physical, psychological), expertise in discussing prognostic uncertainty, establishing goals of care based on patient and family values and preferences and support of the caregivers and families provides an option for taking care of cancer patients suffering with pain.[7] Policies of physical distancing and lockdown to mitigate the spread of novel COVID-19 pandemic have impeded the ability of pain and palliative care physicians to provide quality care. With this background, we conducted a descriptive cross-sectional survey on the challenges faced and the strategies adopted by pain and palliative care physicians working in different oncology setups in India during the novel COVID-19 pandemic. This may help us in preparing a standard operating protocol to provide uninterrupted and good pain and palliative care services to the cancer patients.
MATERIALS AND METHODS
Study design
The descriptive cross-sectional study was conducted by the Department of Onco-Anaesthesia and Palliative Medicine at Dr. BRA, IRCH, AIIMS, New Delhi. Permission was obtained from the hospital Ethics Committee of AIIMS Hospital, New Delhi, India. (IEC-444/22/05.2020). The trial was registered under CTRI. (CTRI/2020/08/027051).
Selection of the participants
The cross-sectional survey was conducted on health-care professionals practicing pain and palliative care in oncology setup in India and willing to participate in the survey.
Aims and objectives
The main objective of the study was to assess the personal challenges faced by the pain and palliative care physicians working in oncology setup in delivering their services and the strategies they have adapted to mitigate these challenges during the time of the novel COVID-19 pandemic. Secondary objective was a comparison of the challenges faced by different oncology health-care setups in India during COVID-19 pandemic.
Methodology
The survey was carried out using the free online software and questionnaire-based tool service from Google Forms (https://docs.google.com/forms). The questionnaire was validated by a panel of five pain and palliative care physicians. There was 100% agreement among all the physicians regarding the questionnaire [Annexure 1]. A link for the questionnaire was generated, which was then sent to the health care professionals practicing pain and palliative care in oncology setup working across the country through social media platforms - WhatsApp and Facebook. The information of professionals working in oncology setup was retrieved from the list of members of various medical bodies like Indian Association of Palliative Care. They were also encouraged to pass on the survey questionnaire to as many other physicians as possible. Clicking the link by participant was taken as consent for the present online survey. Reminder message was sent after 1 week if no response was received. The effort was made to avoid such questions that could reveal the identity of respondents. The questionnaire consisted of three sections – the first section analysed the demographic data such as age, gender, specialty, years of experience in the specialty and place of practice. The second section dealt with the challenges encountered at various levels by pain and palliative care physicians – such as at the hospital level, personal level and at the level of home and hospice. The third section of the questionnaire tried to analyse the strategies adopted at four levels – system, staff, space and stuff.
Statistical analysis
The responses were directly downloaded from the Google forms into an Excel file master chart and necessary graphs were made. The data were then expressed in absolute number and percentage. The comparison between oncological setups (Medical colleges and private hospitals) was done using Fisher’s exact test and Open Epi software. P < 0.05 was considered to be statistically significant.
RESULTS
Link for the questionnaire was sent to 230 pain and palliative care physicians working in oncology setup out of which 207 responded (90%) out of 207 participants, 59% (122) were males and rest 41% (85) were females. The majority of participants (82%) belonged to the age group of 20–40 years. Most of the respondents were anaesthetists (58.45%) working in oncology setup practicing both cancer pain management and palliative care. About 36.4% had an experience of >6 years in their field of specialty. Total of 116 respondents were practicing in medical college (government or private) [Table 1].
| Question with responses | n (percentage) |
|---|---|
| Specialty of the respondents | |
| Anaesthesia* | 121 (58.45) |
| Palliative Medicine | 30 (14.49) |
| Radiation oncology* | 32 (15.45) |
| Medical oncology* | 12 (5.79) |
| Surgical oncology* | 12 (5.79) |
| Years of experience | |
| 1–3 | 62 (30) |
| 3–6 | 70 (33.8) |
| >6 | 75 (36.2) |
| Working area distribution | |
| Medical college (government/private) | 117 (56.5) |
| Government Hospital | 36 (17.4) |
| Private Hospital | 45 (21.7) |
| Free lancing | 9 (4.3) |
Challenges faced at the “Hospital Level”
More than 50 % of physicians faced challenges on various fronts at the hospital level during this pandemic. They felt that there is a possibility of attending to a COVID-19 positive case during their day to day clinical practice with inadequate space in hospital premises to screen the patients. It was also reported by them that the inpatient and out-patient services have come down a lot; care givers are not easily allowed which impeded the counselling procedure. Physicians also faced an ethical dilemma of triaging the patients leaving many patients with mild symptoms unattended. On the academic front they felt that primary pain and palliative care research was getting hampered because of this pandemic [Figure 1].

- Challenges at hospital level.
Challenges faced at “Personal Level”
More than 90% (n = 189) physicians had the fear of carrying infection back home from the hospital. Sixty-one percent (n = 126) had difficulty in convincing the patients and their caregivers about curtailing their visit to the hospital during the pandemic. Forty-nine percent (n = 102) felt that it was getting difficult to keep oneself updated with the latest COVID related guidelines as they are dynamic and changing rapidly on day-to-day basis [Figure 2].
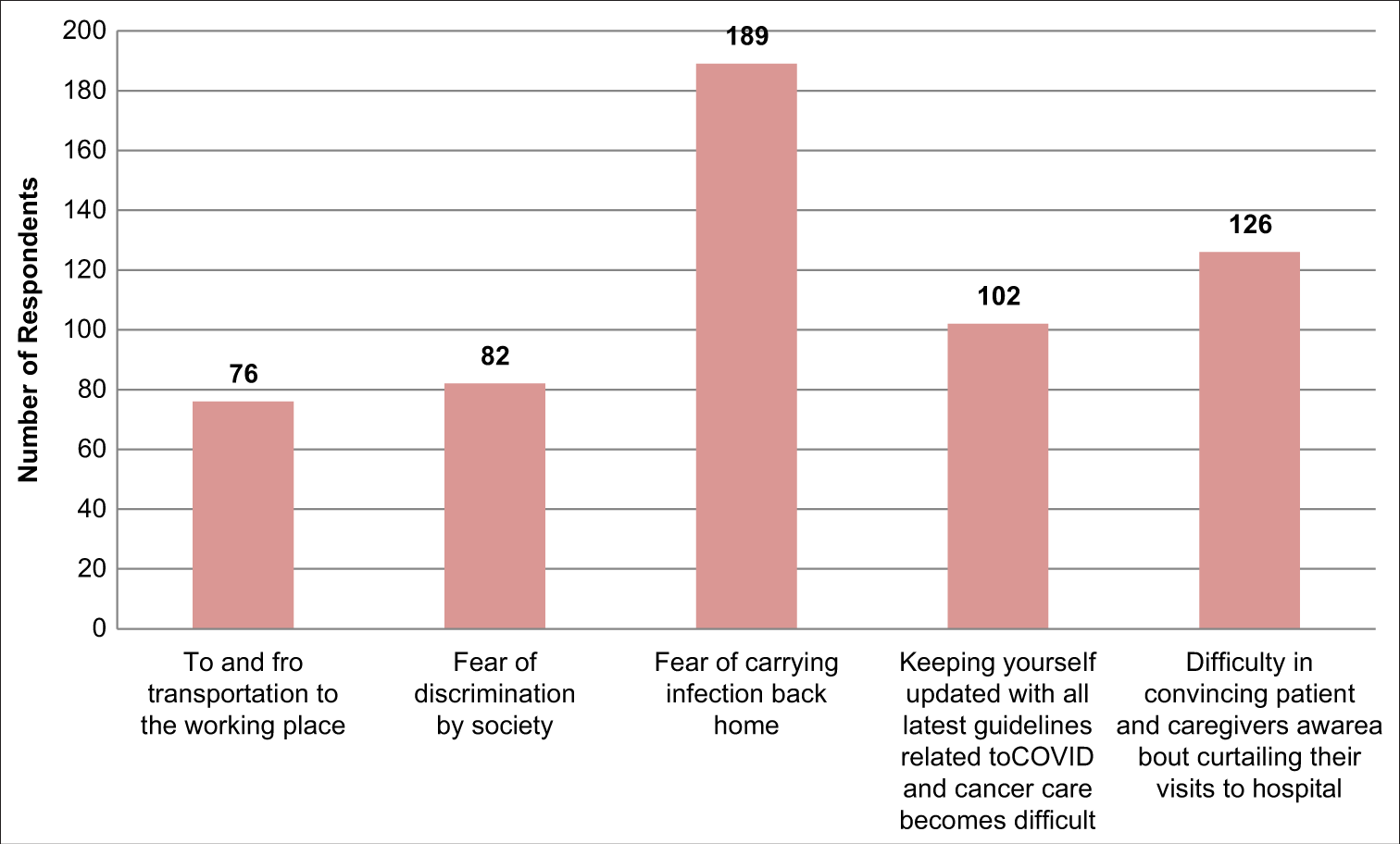
- Challenges at personal level.
Challenges faced at the level of home and hospice based pain and palliative services
At the level of home and hospice based palliative care services 147 physicians (71%) felt that NGOS’s have not been able to provide their palliative care services because of lack of supporting staff, limited supply of PPE and inability to go to patient’s home. 124 physicians (60%) reported that there have been no new admissions by the hospice due to fear of community transmission of coronavirus [Figure 3].
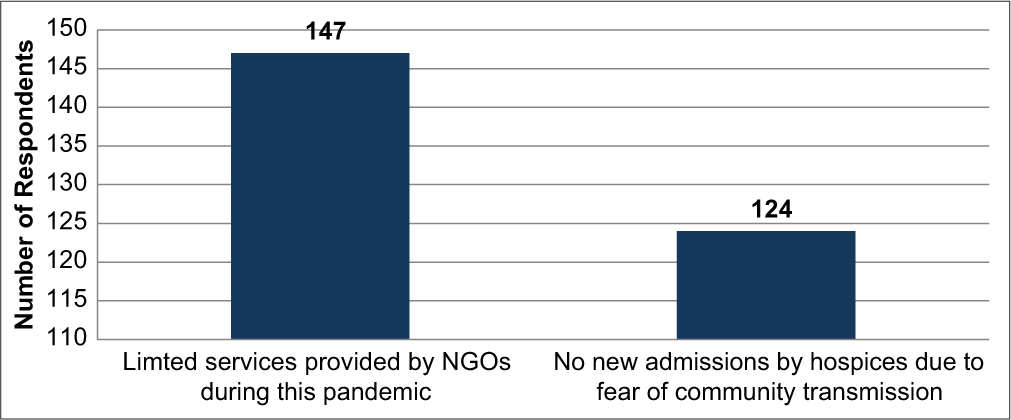
- Challenges at level of home and hospice based services.
Strategies adopted at the level of “System”
To overcome various challenges faced by pain and palliative care physicians working in oncology setup hospitals and administration have adopted strategies at the level of system on various fronts by providing the necessary PPE equipment (172 cases), paid leave for some proportion of healthcare staff (124 cases), telemedicine facility for contacting with the patients (160 cases) and triaging system to identify patients in need of specialized pain and palliative care services in 121 cases [Figure 4].

- System level strategies.
Strategies adopted at the level of “Staff ”
The physicians have adopted some strategies at the level of staff itself to mitigate the challenges posed to them during the pandemic. 129 (62%) responded stating that they are trying to empower the caregivers to play an active role to provide patient care. One hundred and fifteen (55.5%) were practicing teleconsultation for follow up patients. A standardized protocol for symptom management has been done by 123 (59%) respondents. Sixty-seven percent (139) physicians mentioned that educational sessions were also being conducted for task force members; this is apart from the training sessions for the patient and their caregivers (115 respondents) to make them aware of the pandemic and its precautions [Figure 5].

- Staff level strategies.
Strategies adopted at the level of “Space”
At the level of space 176 (85%) physicians told that they were trying to utilize the available space in its best possible way following the norms of social distancing among patient and healthcare workers. Fifty-seven percent responded (118) that they also have identified new areas at their workplace to provide pain and palliative care services [Figure 6].
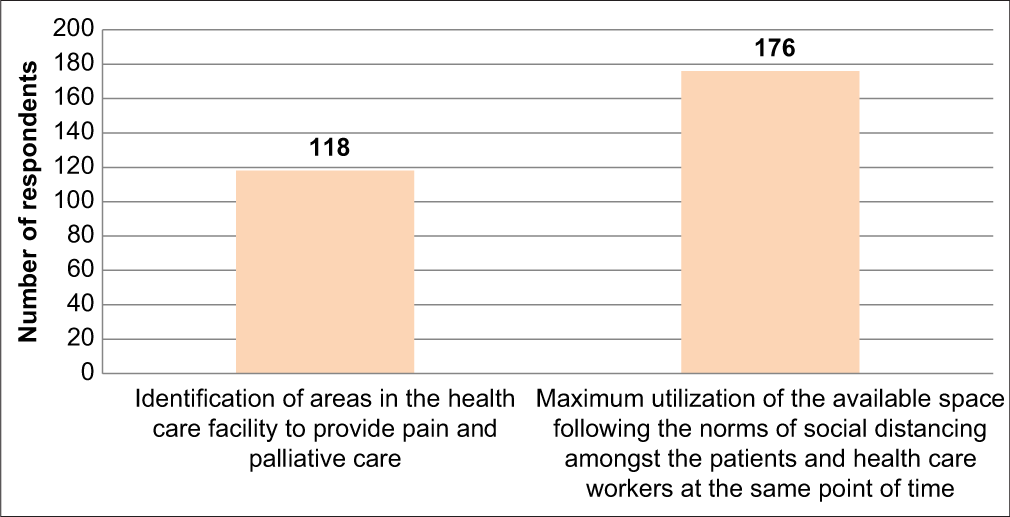
- Space level strategies.
Strategies at the level of “Stuff ”
The strategies apart from the level of the system, staff and space were also adopted at the level of stuff. Stockpiling of necessary medications for symptoms such as nausea, vomiting and dyspnoea was done by 155 (75%). One fifteen prepared (55.5%) medication and equipment kits for home care of patients [Figure 7].
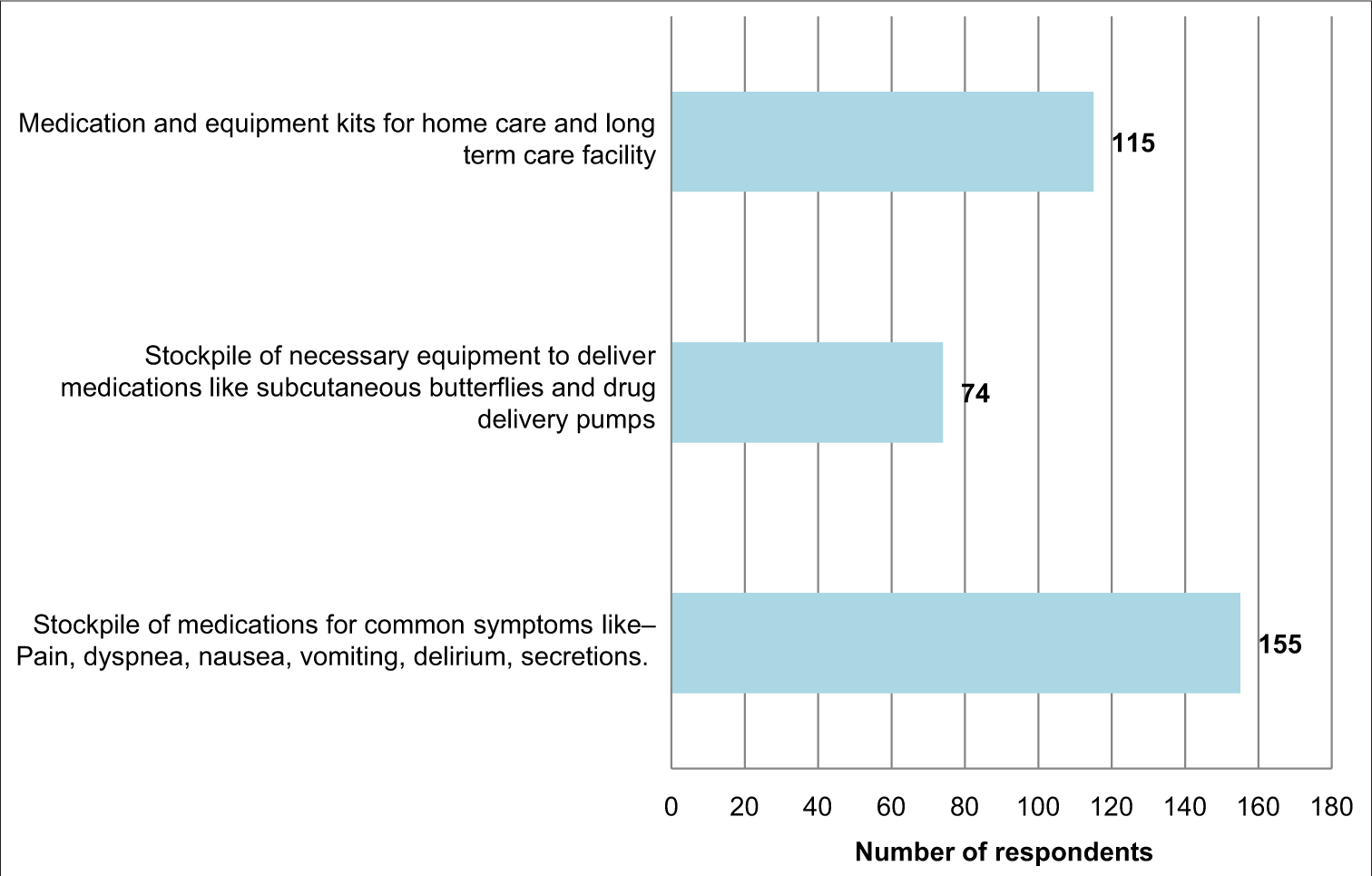
- Stuff level strategies.
Comparison of challenges faced by medical colleges and private hospitals [Table 2]
| Challenges at hospital level | Medical college n/N (%) |
Private hospitals n/N (%) |
Two-tailed P-value |
|---|---|---|---|
| Limited outpatient and inpatient services | 80/117(68.3) | 20/45(44.4) | 0.006 |
| Limited access to allied health care professionals like physiotherapists, wound care specialist | 65/117(55.5) | 10/45(22.2) | 0.0002 |
| Ethical dilemma because of the triaging of patients leaving many patients with mild and moderate symptoms unattended | 70/117(59.8) | 10/45(22.2) | 0.0001 |
| Lack of pharmacy dispensing wings in various hospitals to deliver pain medications like opioids to patients | 15/117(12.8) | 15/45(33.3) | 0.005 |
| Lack of telemedicine facility | 15/117(12.8) | 5/45(11.1) | 1.000 |
| Restricted entry to the caregivers impedes the ability to provide needed psychosocial support to family members which are of utmost importance in cancer patients | 65/117(55.5) | 20/45(44.4) | 0.222 |
| Pain and palliative care research in cancer patients getting affected due to pandemic | 50/117(42.7) | 30/45(66.6) | 0.008 |
| Inadequate place to screen the suspected corona patients and inadequate testing | 70/117(59.8) | 5/45(11.1) | 0.0001 |
| There is a possibility of attending a COVID 19 positive case for symptom management in the palliative care services provided | 80/117(68.3) | 20/45(44.4) | 0.006 |
n: Number of respondents who faced challenges out of the total number of respondents. N: Total Number of respondents
Challenges faced percentage wise by medical colleges were far more on every front compared to private hospitals except in lack of pharmacy dispensing wings to deliver opioid medications and pain and palliative care research getting afflicted during a pandemic.
Challenges in the form of lack of telemedicine facility and restricted entry to caregivers were not statistically significant between the two groups. Otherwise, there was a highly significant statistical difference between the groups among all the other challenges.
DISCUSSION
Novel COVID-19 pandemic since its time of inception has created havoc for the healthcare infrastructure and professionals working in the health-care setup. Cancer patients have been one of the most afflicted during this pandemic as the immunosuppression associated with cancer increases the chances of contracting coronavirus infection.[8] It is not just the patients and their caregivers who are getting affected but also the pain and palliative care physicians working in oncology setup all over the country, as they are facing numerous challenges. At the level of hospital facilities many physicians felt that there is a high possibility of attending a COVID-19 positive case as many patients are asymptomatic. Due to policies of lockdown and social distancing the inpatient and outpatient services were curtailed in their setup, so they need to triage the patients due to which many patients with mild and moderate symptoms could not be attended. They also reported that the space to screen patients for COVID 19 symptoms was inadequate. The services of allied health-care professions such as dieticians, physiotherapists and wound care specialists were also not easily available during the pandemic. Many physicians felt that due to lack of telemedicine facility they were not available to help the patients who could not visit the hospital. Furthermore, restricted entry to the caregivers in the hospital made it difficult for the patients to cope up with the stress of the disease. At a personal level majority feared carrying infection back home and thus had anxiety that they may affect the elderly and small children living along with them. Trouble regarding transportation to and from the hospital and discrimination by society was also reported. Physicians felt the fear of discrimination in the society because of working in the hospital setup. Furthermore, keeping oneself updated regarding the latest guidelines related to COVID and cancer care was found to be difficult. Home and hospice based palliative care services which form an integral component of the management of many terminally sick cancer patients was also not spared from the wrath of this pandemic. Physicians reported that hospice did not take new admissions and NGO’s have not been able to provide home based care like before because of the shortage of manpower and unavailability of sufficiently good quality personal protective equipment. Downer et al. mentioned that during the time of the pandemic, triaging systems have ensured palliative care but no concrete plan has been developed to manage the sudden increase in demands of palliative care. So they devised 4 S strategy addressing stuff, staff, space and system to fulfil the responsibility towards patients.[9] In our study, also we explored the strategies adopted by pain and palliative care physicians on these four fronts. At the level of the system, we found that telemedicine services were being utilized to provide cancer care to patients so that their hospital visits can be reduced only when it is very essential. Necessary PPE kits were being provided so that the healthcare workers (HCWs) feel safe while providing care to the patients. Advance care planning has been adopted by many physicians so that in the terminal stage the caregivers and patients are mentally prepared and do not opt for futile treatments. HCWs have also been called to hospitals on a rotational basis so that there is always a reserve workforce available in time of requirement if some other worker contracts COVID infection. At the level of staff patients’ caregivers are being empowered to provide as much care as possible to the patient. Training sessions have been conducted for all the HCWs to keep them updated about the pandemic and the precautions they need to take. At the same time patients visiting the hospitals along with caregivers are being educated and sensitized about the precautions they need to follow. Using palliative screening tools patients are categorized into priorities so that those who need maximum care do not get neglected. At the level of space areas have been identified in the hospital premises where the pain and palliative care patients could be cared for and if there was no extra space available whatever space was available judicious use of that is being done keeping in mind the norms of social distancing. At the level of stuff physicians have done stockpiling of necessary equipment and drugs for symptomatic management of cancer patients. Kits which could be handed over to the patients have also been prepared for long term care at home. As far as the comparison of medical college setup and private hospitals is concerned, there was a huge gap among the challenges faced by the medical college setup. Medical colleges had limited outpatient and inpatient services, limited access to allied health-care professionals, inadequate place to screen for suspected COVID patients. The discrepancy in challenges between the two setups could be explained by the huge patient upload catered to by the medical colleges compared to the private hospitals and the lack of infrastructural facilities. Private hospitals compared to medical colleges faced more challenges in domain of research getting affected and lack of pharmacy dispensing wings for opioid for cancer patients. Singhai et al. have said that the present pandemic and the national strategies formulated to mitigate the spread of COVID-19 pose significant challenges to the delivery of palliative care at hospital level, home based and hospice based palliative care services and they have proposed System of triaging, Hospital policy, Adequate and uninterrupted supply of essential medications, Resources, Empathetic communication and Documentation strategy to overcome these challenges.[10] Willian et al. mentioned that a primary challenge when planning for a pandemic is human resource management. Hospital admissions will need to come up with plans and ideas that does not hamper the treatment process and at the same time protect patients and HCWs as infections rise.[11] Randall et al. have emphasized the importance of addressing advance care planning during novel COVID-19 pandemic. They reiterate the fact that physicians should hold discussions regarding end-of-life care with patients and their caregivers especially for people suffering from chronic illness like cancer. They formulated an informed assent approach to code status discussions, as it may be useful for patients in whom cardiopulmonary resuscitation is unlikely to allow a successful return to a quality of life.[12] We also propose that a standard operating protocol be formulated by the hospitals keeping in mind the challenges faced by oncology setups in our country.
Limitations of the study
There are several limitations to our study. First, the sample size is small, therefore it may not be representative of the challenges faced and strategies adopted by pain and palliative care physicians working all over the country. Second, there could have been many other challenges faced at individual and institutional level but we could not elicit those through our questionnaire. The respondents were given an option to discuss other challenges encountered but we did not get response for the same. Furthermore, the challenges encountered by physicians in India may not be representative of challenges faced by physicians in other countries because of different healthcare setup and resources available. Nevertheless, the study conducted by us is first of its kind to highlight the different challenges faced and strategies adopted by pain and palliative care physicians working in oncology setup in India.
CONCLUSION
The current COVID-19 pandemic has shaken the very roots of healthcare all over the world. It has brought to the fore various challenges our pain and palliative care physicians working in oncology setup have been facing otherwise also. Till date, there has been emphasis on cure and biomedical character of health care as opposed to palliative care, which focuses on quality of life of patients. But amidst this pandemic, palliative care is different with experts realising the various possibilities in this field of care and research. It is high time we address the challenges faced by our physicians on various fronts-be it at hospital level or personal level. For that the government and the health-care industry need to come forward and work as a joint force. Standard operating protocols, guidelines and effective strategies have to be formulated so that we are better equipped in the future to deal with such kind of pandemics. This will help us immensely in proving uninterrupted holistic care to the cancer patients and at the same time protect our HCWs in this battle.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- COVID-19-New insights on a rapidly changing epidemic. JAMA. 2020;323:1339-40.
- [CrossRef] [Google Scholar]
- WHO Announces COVID-19 Outbreak a Pandemic. 2020. Geneva: World Health Organization; Available from: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic [Last accessed on 2020 Jun 16]
- [Google Scholar]
- Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054-62.
- [CrossRef] [Google Scholar]
- Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;7:1239-42.
- [CrossRef] [Google Scholar]
- Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat Med. 2020;26:506-10.
- [CrossRef] [Google Scholar]
- Quality of life and needs of the Indian advanced cancer patients receiving palliative care assessment of the quality of life, problems, and needs of the advanced cancer patient receiving palliative care. Cancer Res Stat Treat. 2019;2:13844.
- [Google Scholar]
- Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335-7.
- [CrossRef] [Google Scholar]
- Educational fellows in care at the end of life. Palliating a pandemic: “All patients must be cared for”. J Pain Symptom Manage. 2010;39:291-5.
- [CrossRef] [Google Scholar]
- Palliative care for advanced cancer patients in theCOVID-19 pandemic: Challenges and adaptations. Cancer Res Stat Treat. 2020;3:127-32.
- [CrossRef] [Google Scholar]
- Care of haematology patients in a COVID-19 epidemic. Br J Haematol. 2020;189:241-3.
- [CrossRef] [Google Scholar]
- the importance of addressing advance care planning and decisions about do-not-resuscitate orders during novel coronavirus 2019 (COVID-19) JAMA. 2020;323:1771-2.
- [CrossRef] [Google Scholar]
ANNEXURE 1
Challenges faced and strategies adopted byPain and Palliative care physicians working inoncology setup during COVID 19 Pandemic
COVID 19 pandemic has emerged as a clinical challenge to all pain and palliative care physicians working in oncology setup worldwide as it is important to provide comfort care at all stages in cancer patients. This survey would help in assessing the challenges and problems faced by the Pain and Palliative care physicians in dealing with cancer patients and strategies adopted by them in mitigating those challenges. Thus it will provide an insight for formulation of a management plan for dealing with the current pandemic and such pandemics in future.
I would request you for your valuable participation in this survey. You may select the most appropriate option or more than one option where necessary.
This survey is being conducted by the Department of Oncoanaesthesia and Palliative Medicine, Dr. BRAIRCH, AIIMS, New Delhi. The study participation is voluntary and all the information will be kept confidential.
If you have any questions about this survey or any study related issue, you can contact the principal investigator Dr. Seema Mishra at seemamishra2003@gmail.com
*Required
1. Consent to participate: I have reviewed the information provided above. I understand thatmy participation will be voluntary. By clicking on “I Agree” button, I give consent toparticipate in the study.*
Mark only one oval.
◯ I Agree
Personal details
2. Age (Years)*
Mark only one oval.
◯ 20-40
◯ 40-60
◯ >60
3. Gender*
Mark only one oval.
◯ Male
◯ Female
◯ Other: ___________________
4. Specialty (Multiple options can be marked depending upon the practice)*
Tick all that apply.
□ Anaesthesia
□ Pain Medicine
□ Palliative medicine
□ Critical Care
□ Radiation Oncology
□ Medical Oncology
□ Surgical Oncology
Other: □ ___________________
5. Years of experience in the specialty*
Mark only one oval.
◯ 1-3 Years
◯ 3-6 Years
◯ >6 Years
6. Place of practice*
Mark only one oval.
◯ Medical college (Government/Private)
◯ Government hospital
◯ Private hospital
◯ Free lancing
7. Name of the college/hospital with city and state (If applicable)*
Challenges at different levels
You can choose more than one option (Tick all that apply)
8. Challenges face at “Hospital level”*
Tick all that apply.
□ Limited outpatient and inpatient services.
□ Limited access to allied health care professionals like physiotherapist, wound care specialist.
□ Ethical dilemma because of triaging of patients leaving many patients with mild and moderatesymptoms unattended
□ Lack of pharmacy dispensing wings in various hospitals to deliver pain medications like opioid topatient.
□ Lack of Telemedicine facility
□ Restricted entry to the caregivers impedes the ability to provide needed psychosocial support tofamily members which is of utmost importance in cancer patients
□ Pain and palliative care research in cancer patients getting affected due to pandemic.
□ Inadequate place to screen the suspected corona patients and inadequate testing.
□ There is a possibility of attending a COVID 19 positive case for symptom management in thepalliative care services provided
Other: □ ___________________
9. Challenges at “Personal level”*
Tick all that apply.
□ To and fro transportation to the working place
□ Fear of discrimination by society
□ Fear of carrying infection back home
□ Keeping yourself updated with all latest guidelines related to COVID and cancer care becomesdifficult
□ Difficulty in convincing patient and caregivers aware about curtailing their visits to hospital
Other: □ ___________________
10. Challenges at the “Level of Home and hospice” based pain and palliative services *
Tick all that apply.
□ Limited services provided by NGO’s during this pandemic because of lack of their support staff, inability to go to patients home and limited availability of PPE with them
□ Reduced admissions by the hospices due to fear of community transmission.
Other: □ ___________________
Strategies adopted at different levels
You can choose more than one option (Tick all that apply)
11. “System level” strategies*
Tick all that apply.
□ Created a Triage system to identify patients in need of specialist pain and palliative care
□ Use of Telemedicine for direct consultation support for the patients and their family members
□ Advanced care planning done for all the patients admitted in the hospital setting
□ Creating a system for transfer of the patients who require dedicated palliative care and hospiceservices.
□ Utilizing services of Non Governmental organizations for helping patients in need of pain andpalliative care services.
□ Paid leave for some proportion of health care workers so that in case of inadvertent need ofquarantine of those affected there is always a pool of workforce left to provide health services.
□ Providing necessary PPE equipments like N95 mask, Hydroxychloroquine tablets to thehealthcare workers in the department
Other: □ ___________________
12. “Staff level” strategies*
Tick all that apply.
□ Formation of the Task force for providing Pain and Palliative care
□ Conduct of educational sessions for the task force members during the COVID Pandemic
□ Conduct of training sessions for the patient and their caregivers explaining them about thepandemic and the precautions they need to follow
□ Development of standardized protocols for symptom management
□ Use of any screening tool for further triaging the palliative care need patients into priority A, B andC
□ Involving the specialized allied health care workers for providing psychosocial and spiritualsupport
□ Use of screening stations to segregate new patients and those who are on follow up
□ Use of screening stations to identify patients with Influenze like illness or severe acuterespiratory illness so that they can be diverted to dedicated COVID care facility
□ Use of Tele-consultation for every patient under follow up.
□ Empowering family caregivers to play an active role in providing care
Other: □ ___________________
13. “Space level” strategies*
Tick all that apply.
□ Identification of areas in the health care facility to provide pain and palliative care
□ Maximum utilization of the available space following the norms of social distancing amongst thepatients and health care workers at the same point of time
Other: □ ___________________
14. Strategies at the level of “Stuff ”*
Tick all that apply.
□ Stockpile of medications for common symptoms like – Pain, dyspnea, nausea, vomiting, delirium,secretions.
□ Stockpile of necessary equipment to deliver medications like subcutaneous butterflies and drugdelivery pumps
□ Medication and equipment kits for home care and long term care facility
Other: □ ___________________






