Translate this page into:
Attitudes, Aptitudes, Barriers and Knowledge of Pain Physicians towards Palliative Care Practice – A National Survey, India

-
Received: ,
Accepted: ,
How to cite this article: Pai RS, Monteiro G, Tarey SD. Attitudes, aptitudes, barriers and knowledge of pain physicians towards palliative care practice – A national survey, India. Indian J Palliat Care 2021;27(2):242-50.
Abstract
Objectives:
The bio-psycho-socio-spiritual model is a common management approach in palliative care (PC) and chronic pain medicine (CPM), adopted by PC Physicians and Pain Physicians (PPs), respectively. There is a dearth of services and personnel of PC in India. As PPs are familiar with pain management and the bio-psycho-socio-spiritual model, we hypothesised that they would be willing to incorporate PC in their practice and therefore, sought to understand their attitudes/aptitudes/barriers/knowledge towards it.
Materials and Methods:
We did a cross-sectional cohort study through a national survey of Indian PPs. The ten- item validated, survey questionnaire was mailed to 1300 PPs having E mail and registered with Indian Society for Study of Pain.
Results:
We received responses from 6.6% of the PPs. About 10.39% did not want to practice PC; the rest were either practicing or wanted to, or were unable to. 81.8% had <10 years CPM experience while the rest had 10–15 years. About 53.3% PPs had <10 years’ experience in PC; 10.4% had > 10 years and the rest had not practiced. About 70% were motivated by human suffering or had “personal reasons.” About 40.26% had no barriers; the rest cited stress or lack of infrastructure/knowledge/skills/time/financial compensation. The majority chose institutional courses for training and the popular choice of duration of the course was 3 months. The opinion on financial viability/non-viability of PC was equally divided among the respondents. About 62.3% had “knowledge” but half of them lacked “skills;” 27.6% lacked both; the rest had no inclination towards PC. About a third felt multi-disciplinary care was feasible while half felt that it was partially feasible.
Conclusion:
Policy-makers, at regional to global levels are strategizing options for popularizing PC since it supports the dualistic model of cure and care, most essential for both, chronic-debilitating or life-limiting illnesses. The poor response to our survey was a major limiting factor. However, among the respondents, the majority showed both aptitude and a favourable attitude for PC practice. The inability to identify major barriers for not choosing PC did not support our hypothesis. However, we feel that PPs are a cohort who can be motivated/ encouraged to take up some form of brief, comprehensive courses in PC so that they can be conversant with the specific knowledge and skills needed to practice the multi-dimensional aspects of PC in their own settings.
Keywords
Attitudes-aptitude-barriers-knowledge
Indian pain physicians
Integration of Palliative care with Chronic Pain services
National survey
INTRODUCTION
The WHO defines palliative care (PC) as holistic and compassionate care of patients at any stage of their life limiting illnesses. This also includes care of the caregivers and family. Although patients with cancer are the major beneficiaries of PC, patients with other life limiting illnesses like HIV-AIDS, cardio-respiratory diseases refractory to treatment, chronic kidney diseases and degenerative neurological diseases often require PC when curative treatments are no longer effective.
Chronic pain causes significant morbidity in a large number of patients that is not only physical but also psychosocial. With the development of the bio-psycho-socio-spiritual model of pain, there has been a better understanding of chronic pain and the suffering related to it. The sheer magnitude of the problem has led to development of a new speciality-chronic pain medicine (CPM) which is led is led by specialists referred to as pain physicians (PPs). PPs are capable of having a compassionate and holistic attitude toward managing chronic pain which often includes cancer pain. In India too, like elsewhere in world, chronic pain is being managed by PPs who are mostly anaesthesiologists.[1] Anaesthesiologists learn to deal with “pain” from their early days of training. As PPs, they learn to approach “pain” from a “bio-psycho-social model.”
There is a convergence in the philosophy of managing symptoms, especially pain, between CPM and PC. PC Physicians (PCPs) manage pain in more than 80% of patients with advanced cancers and other life-limiting non-cancer conditions.[2] However, in PC, the “bio-psycho-socio-spiritual model” is applicable to several symptoms other than pain. With an increase in non-communicable diseases and life expectancy in general, patients need long-term care and often, PC towards end of life. There is a dearth of PCPs in India. A majority of the centres are located in urban India. Semi-urban and rural populations are grossly underserved when it comes to PC.
There is a pressing need to make PC accessible across all types of practice settings. This requires identification of potential practitioners who may have the appropriate attitude and aptitude to get trained and provide PC in their practice settings. PPs constitute a large pool of physicians managing cancer pains who could extend their expertise to provide PC.
We conducted a pilot study at the Annual Pain Conference of Indian Society for Study of Pain (ISSP), 2019, held in Bengaluru, India. A ten item questionnaire was developed by us and distributed randomly to 20 PPs who through their responses indicated their attitudes/aptitudes/barriers/ knowledge towards PC. The interest shown by them encouraged us to conduct a more detailed and structured survey[3] to assess the same.
We hypothesised that if adequate opportunity and training were available, many PPs would perhaps be willing to incorporate PC in their practice settings. Therefore, we designed a descriptive cross-sectional cohort study of PPs. We wished to know if the respondents knew the various aspects of PC besides pain; if they favoured enhancing knowledge or skills through education or training and thereby integration of pain and palliative services.
MATERIALS AND METHODS
A structured survey questionnaire (SQ) with ten items was developed. Seven items were closed questions. Two items had multiple possible responses. One item was open to respondents to formulate their own answer.
The SQ was mailed to five PPs, with more than 10 years’ experience in the field, to independently rate and mail their opinion on each framed item for “clarity,” “relevance,” “ambiguity” and “simplicity” using Yaghmale’s 4-point scale.[4] Their suggestions were incorporated.
The SQ was validated using item-content validity index and the scale-level content validity index. The probability of chance universal agreement (pc), with regard to each of the four attributes of content validity and the modified kappa statistic, was calculated [Appendix A-D].[5] The Evaluation criteria for kappa were graded using guidelines described by Cicchetti and Sparrow (1981) and Fleiss (1981).[6,7]
Approval for the survey was obtained from the Institutional Ethics committee. A subject information sheet detailing the purpose of the study, the freedom to participate, the ensuring of confidentiality and the agreeability to implied consent was mailed along with a link to the SQ. The SQ was mailed thrice at an interval of 30 days to ensure maximum participation.
RESULTS
There are 2300 registered members of the ISSP. 1300 members with e-mail addresses were selected for the study. Around 130 mails bounced. Four duplicate responses were deleted. A total of 77 (6.6%) responses received were analysed [Figure 1]. 1089 members (93.4%) did not respond.
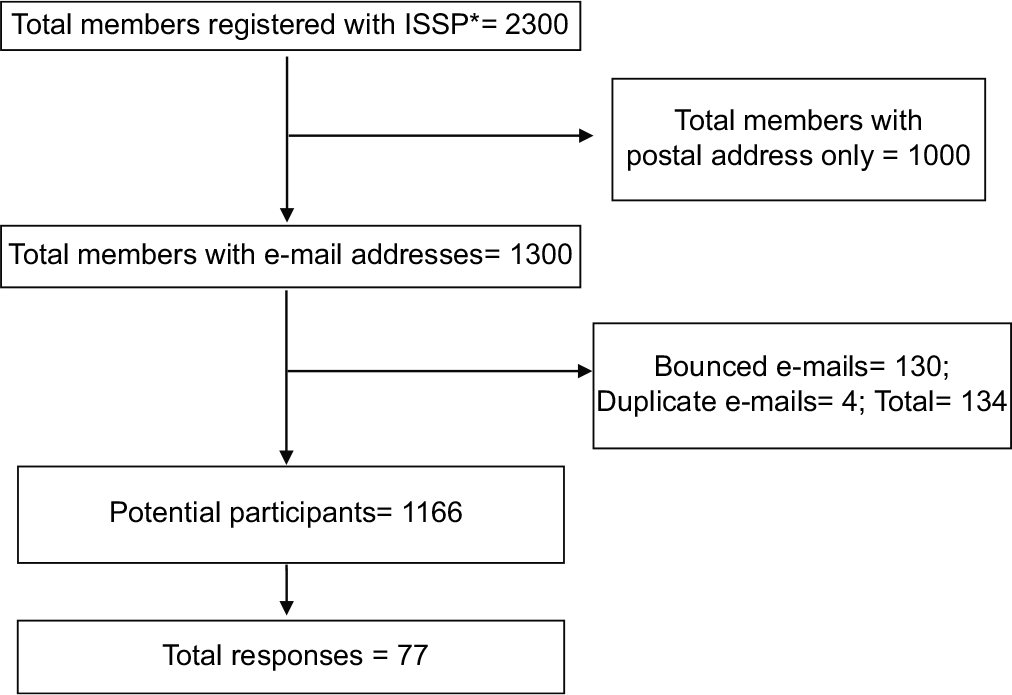
- Flow-chart depicting the selection of respondents. (ISSP*: Indian Society for Study of Pain).
When asked about the aptitude towards PC, 54.54% anaesthesiologists practising CPM replied that they were practising it; 29.9% replied that they would have liked to practise it; 10.39% did not want to practise PC and 5.19% replied that they were unable to practise it [Figure 2].
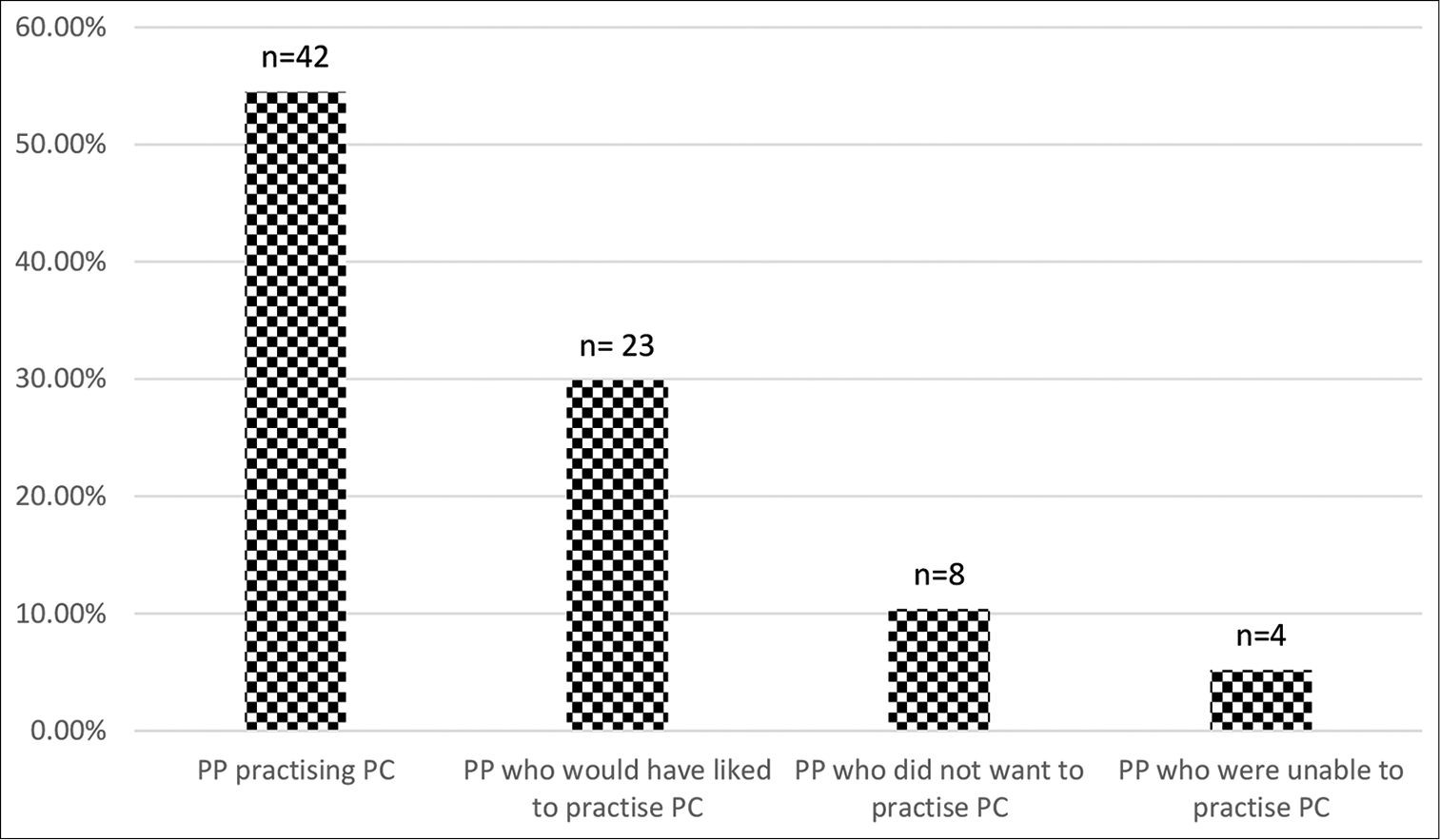
- Interest shown in palliative care practice by the anaesthesiologists primarily practising chronic pain medicine.
As for the number of years of experience in CPM, 45.5% had less than 5 years’ experience; 36.3% had 5–10 years’ experience; 5.2% had 10–15 years’ experience and 12.99% had >15 years’ experience [Figure 3].
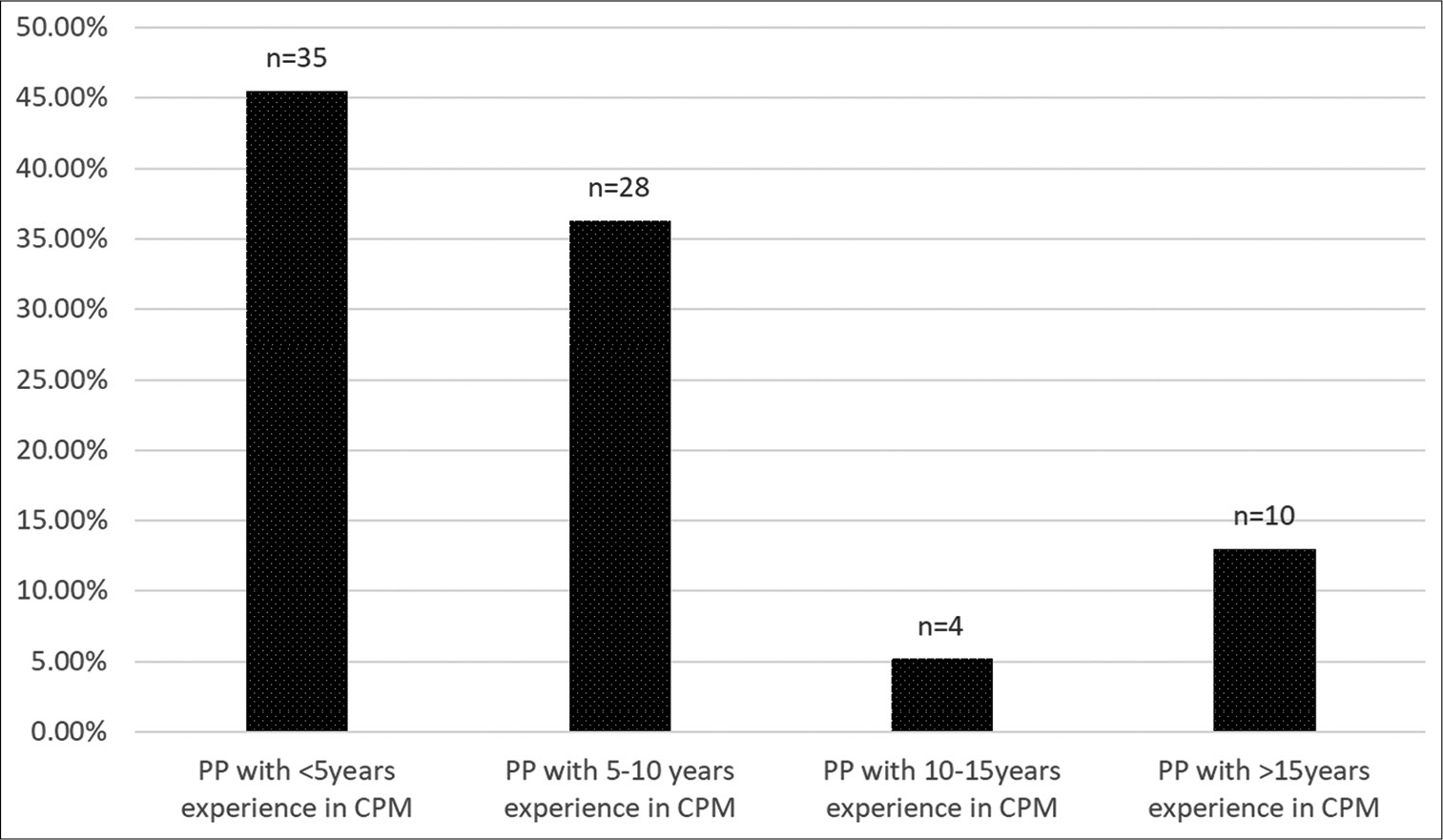
- Experience in chronic pain medicine.
As for the number of years of experience in PC, 36.4% had <5 years’; 16.9% had 5–10 years’ experience; 10.4% had >10 years’ experience and 36.4% had not practised PC [Figure 4].
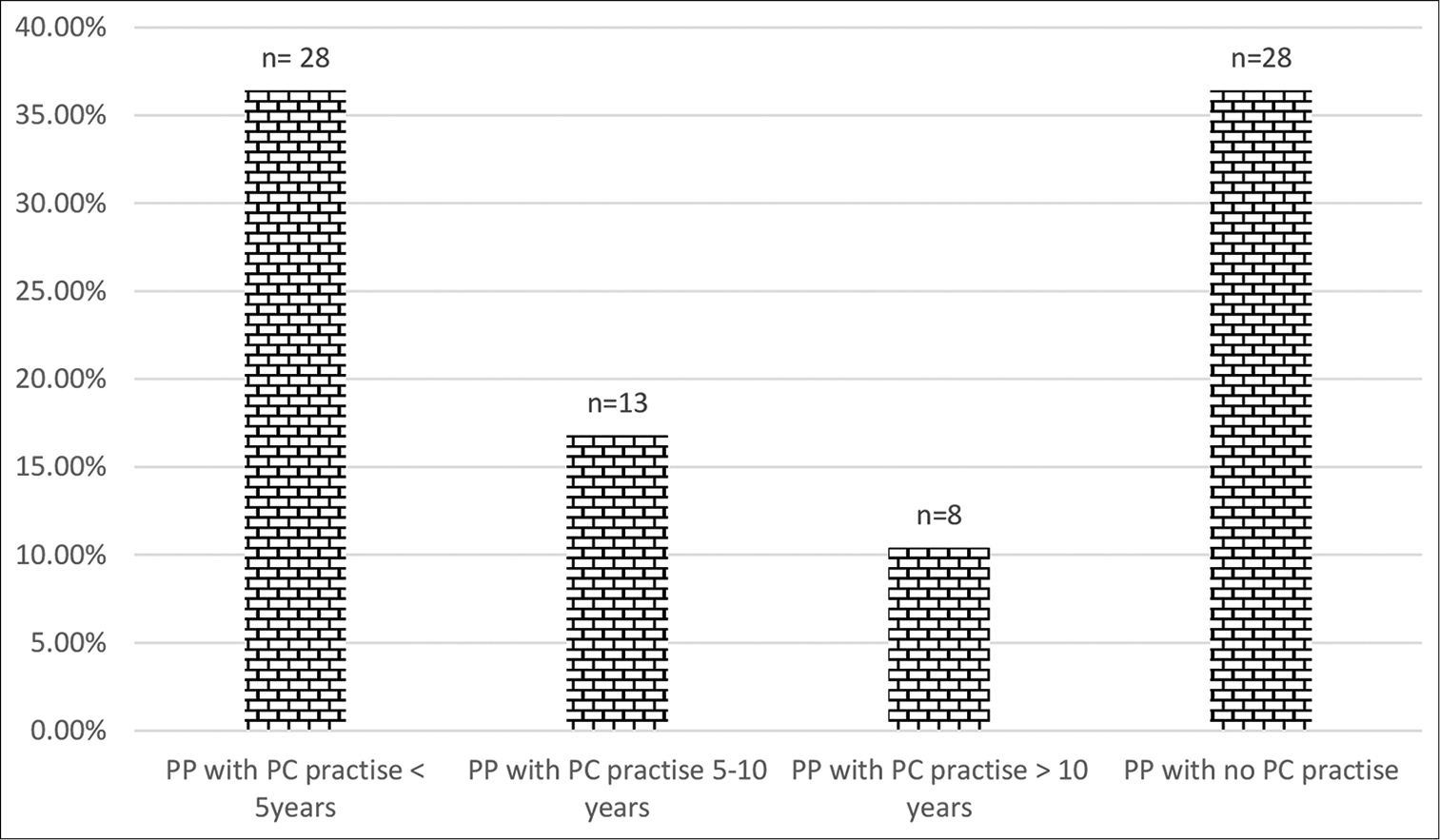
- Experience of pain physicians in palliative care.
When we sought to elicit reasons for the attitudes or aptitudes of PPs towards PC, the single response chosen by 49.4% was their in-built attitude towards human suffering; 9% chose personal reasons; 18.1% chose inability to integrate PC; and, 10.4% maintained that they did not want to practise PC. 10.4% chose both the essential attitude and personal reasons, while 2.6% chose personal reasons but being unable to practise [Table 1].
| Reason for opting for PC | Numbers (n) and (%) |
|---|---|
| You had the essential attitude to address the multi-dimensional aspect of suffering in terminal illness | n=46 (59.74) |
| Personal reasons (gain knowledge/“inner calling”/seeing a close associate’s suffering/having to decide on withholding treatment) | n=17 (22.07) |
| Not applicable because I haven’t been able to integrate it in my chronic pain practice | n=16 (20.78) |
| Not applicable presently, as I don’t want to practice palliative care | n=8 (10.40) |
For a question that sought to understand barriers of PPs towards PC, 16.8% highlighted their work-place not being an established PC service-provider; 15.58% felt that they lacked the necessary knowledge/skills and 14.29% felt that PC is stressful and time-consuming. About 12.98% felt that the lack of an ear-marked place like a clinic was the barrier while 9.09% felt that PC was not financially viable. A small percentage – 7.79% felt that it was difficult to invest time in gaining knowledge about PC and 6.49% felt that getting referrals was difficult. 7.79%, though not associated with PC, worked in places which had well-functioning PC departments. 40.26% re-affirmed that they were practising PC and had no barriers [Table 2].
| Response item | Number (n) and (%) |
|---|---|
| Lack of knowledge/skills in palliative care | n=12 (15.58) |
| Perception that addressing other domains of palliative care as being too stressful and time consuming | n=11 (14.29) |
| Investing time to gain the required knowledge is difficult | n=6 (7.79) |
| Palliative care is not financially viable as the public knowledge about the scope and benefits of palliative care is scant | n=7 (9.09) |
| Getting referrals is difficult | n=5 (6.49) |
| Most pain physicians lack their own clinic and hence cannot provide a one-stop place for patients needing palliative care also | n=10 (12.98) |
| Your work-place is still not an established service-provider for palliative care | n=13 (16.88) |
| Your work-place has a well-functioning palliative care department and, so, you haven’t actually given it a thought | n=6 (7.79) |
| Not applicable as I practise palliative care | n=31 (40.26) |
As for the preference of training methodology, 51.9% chose institutional courses, 29.9% chose correspondence courses and one respondent chose a certificate course for PC conducted in Trivandrum. About 16.9% chose the item – “not applicable” [Figure 5].
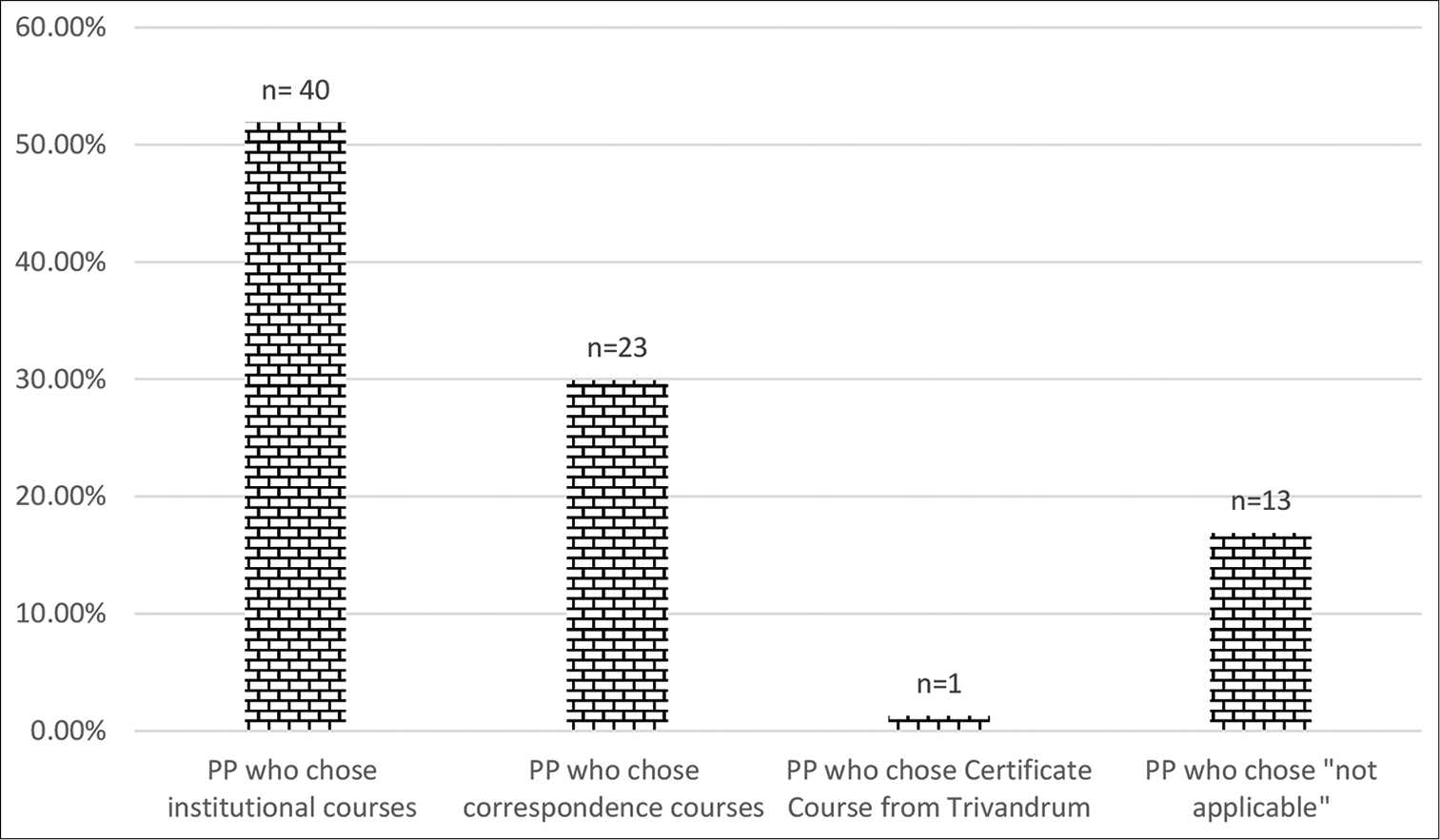
- Choice of training methodology in palliative care.
In the SQ, we wished to find how much time the PPs were willing to spend on training in PC. 50.6% were willing to spend 3 months; 14.3% preferred 6–12 months and 13% preferred 1–2 years of training. About 22% did not wish to answer as they did not want to practise PC [Figure 6].
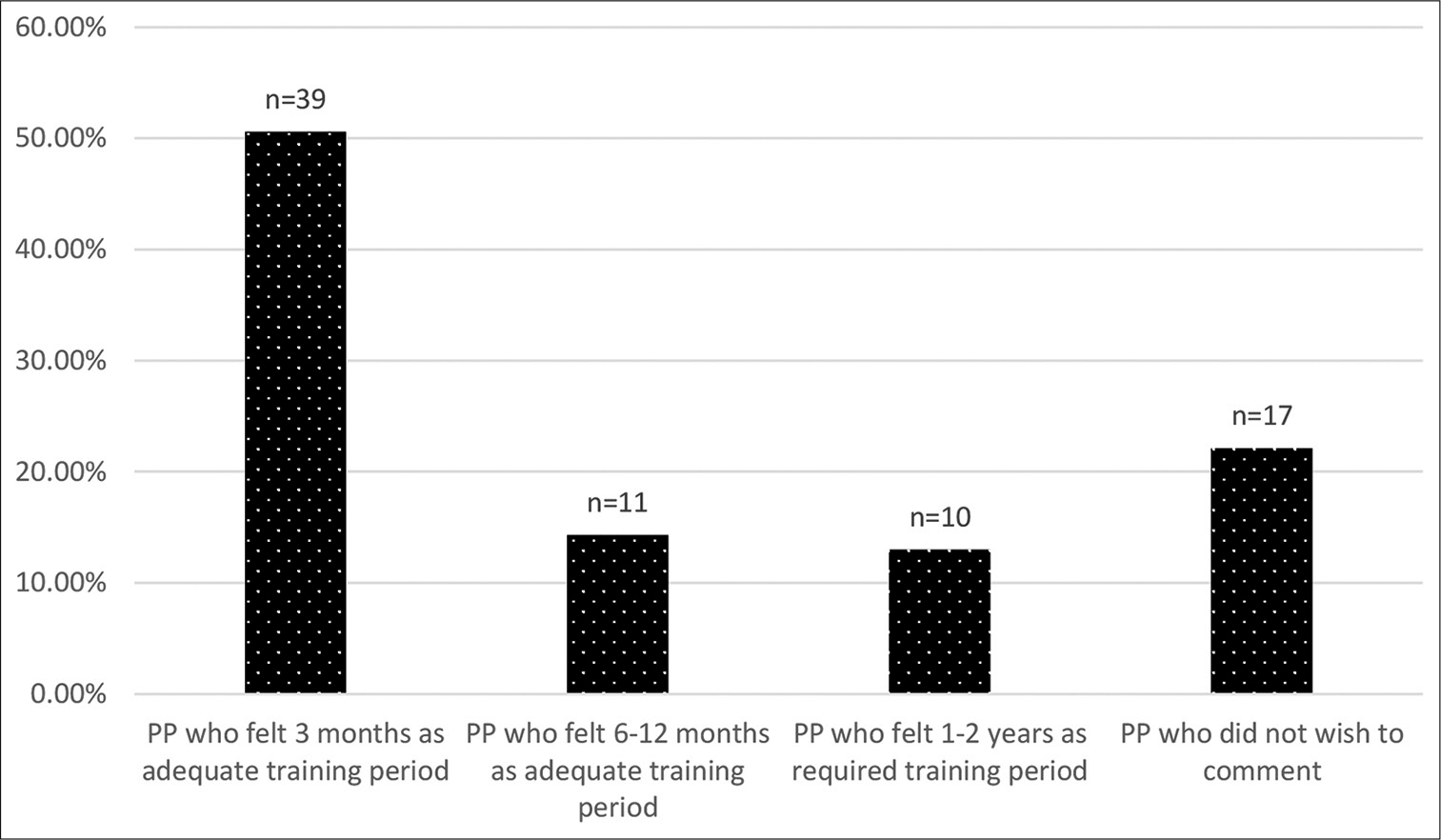
- Duration of training period deemed adequate to acquire necessary palliative care skills.
Another question asked, was related to the general impression that PC was not financially viable. 27.3% felt that PC was financially viable while 31.2% felt that it was not. About 41.6% said that they could not give an opinion [Figure 7].
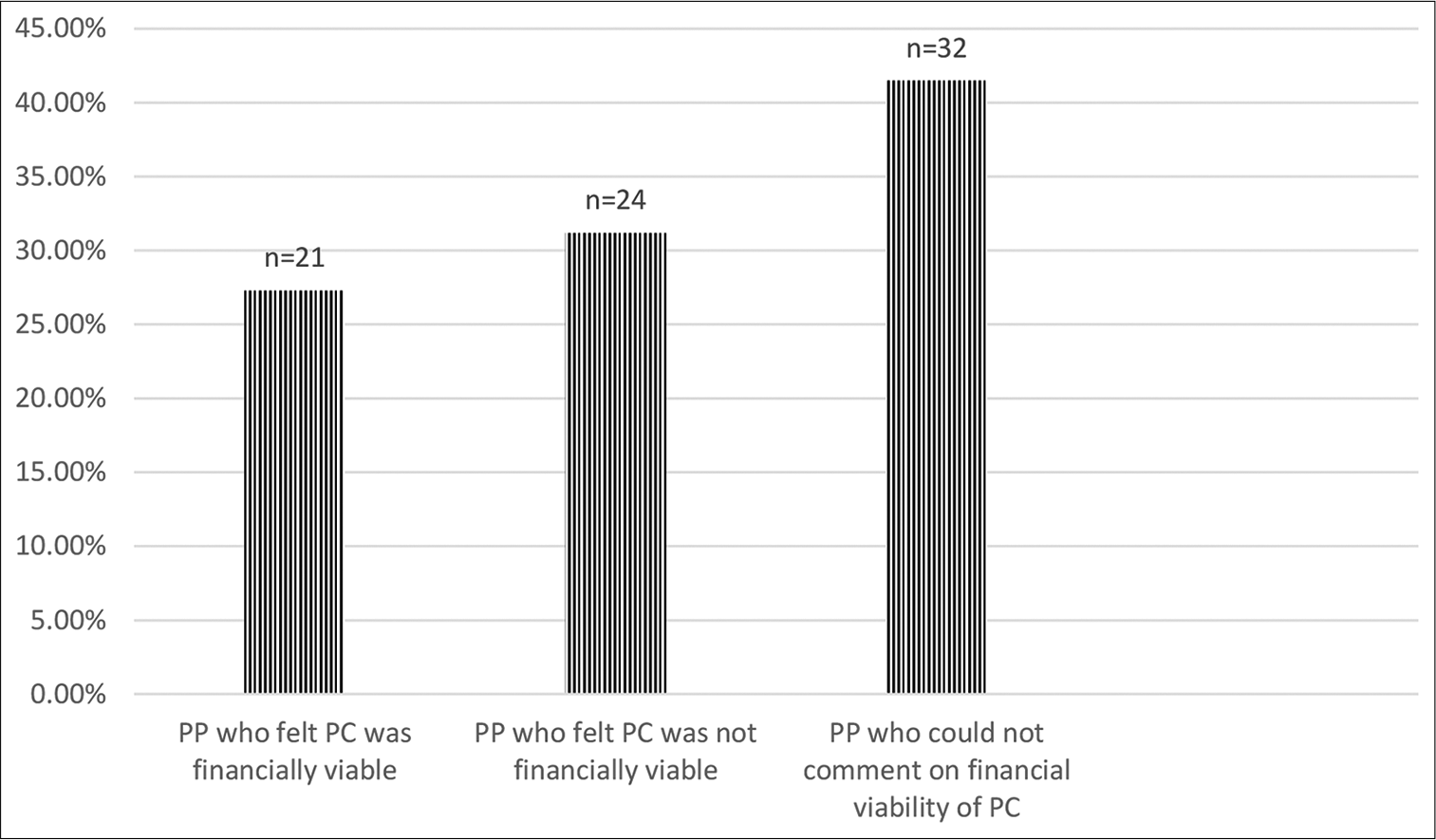
- Financial viability of palliative care as perceived by pain physicians.
We allowed the respondents to self-evaluate their knowledge and competency in the various domains of PC in the penultimate question. The responses are tabulated in Table 3.
| Key domains addressed in palliative care | Have knowledge and skills in PC | Have knowledge but need skills in PC | Need knowledge and skills in PC | Not applicable |
|---|---|---|---|---|
| Number (n) (%) | Number (n) (%) | Number (n) (%) | Number (n) (%) | |
| Other organ symptoms (CNS, cardiac, GIT) | n=23 (29.9) | n=27 (35.1) | n=17 (22) | n=10 (13) |
| Spiritual distress | n=19 (24.7) | n=25 (32.5) | n=25 (32.5) | n=8 (10.3) |
| Psycho-social issues (depression, finances) | n=20 (26) | n=26 (33.8) | n=22 (28.6) | n=9 (11.6) |
| Communication of “bad prognosis” to patient &/or family | n=30 (39) | n=26 (33.8) | n=13 (16.9) | n=8 (10.3) |
| End-of-Life (EOLC) | n=20 (26) | n=22 (28.6) | n=27 (35.1) | n=8 (10.3) |
| “Shared decision making” with your patient and their family | n=28 (36.4) | n=22 (28.6) | n=19 (24.7) | n=8 (10.3) |
| “Care-giver distress” | n=18 (23.4) | n=25 (32.5) | n=26 (33.8) | n=8 (10.3) |
When asked for their opinion about the feasibility of a full-fledged multi-disciplinary team in PC, 32.5% felt that it was feasible and 6.5% felt that it was not feasible. About 53.2% felt that it was only partially feasible. About 7.8% did not wish to comment [Figure 8].
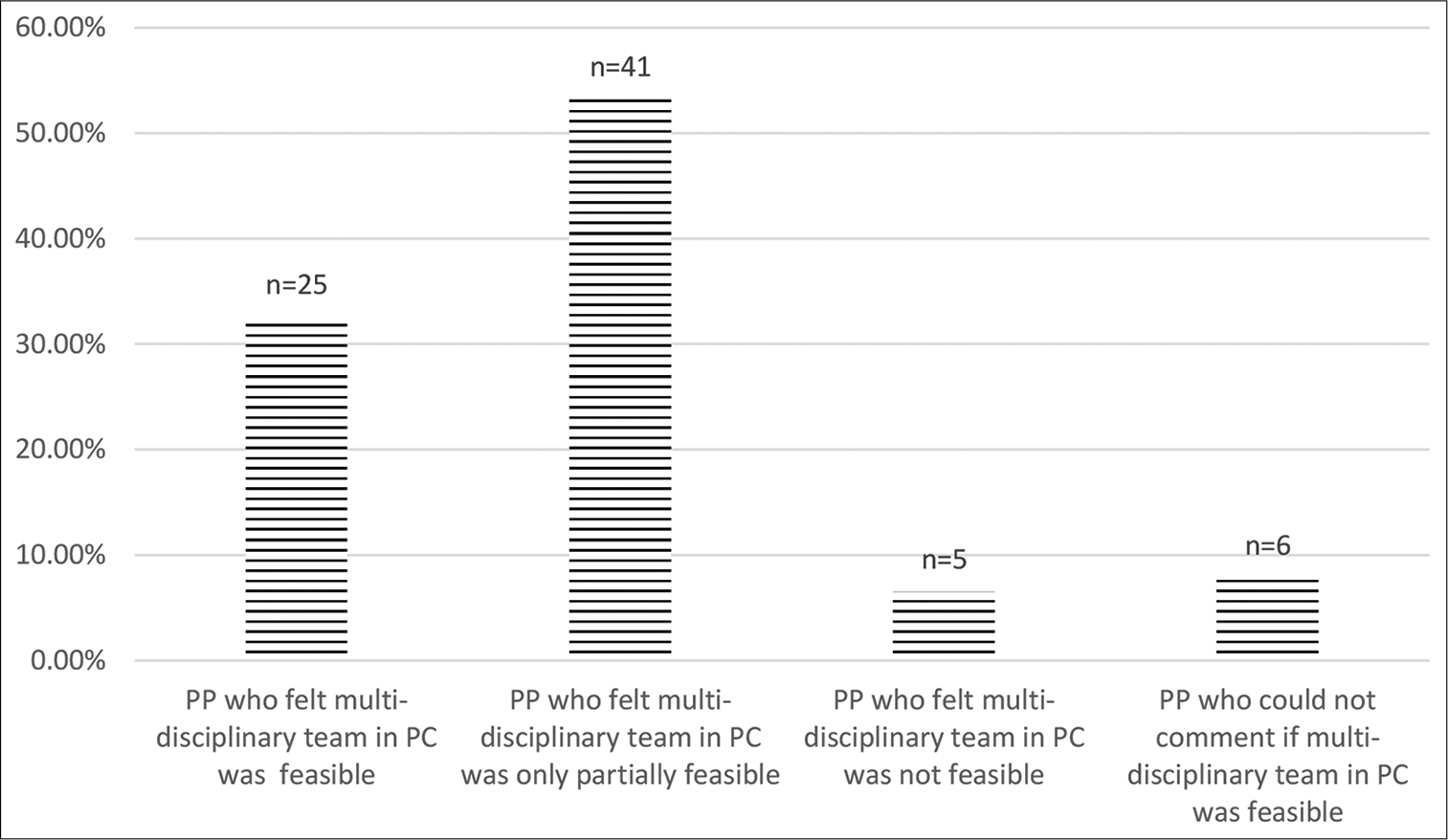
- Opinion of pain physicians about feasibility of organising an ideal palliative care team.
DISCUSSION
PC and CPM share the common goals of reaching out to patients and addressing their suffering so as to improve their quality of life (QoL). In settings where PC is available, pain is managed by PCPs. Hoskin (2006) has reported that 10–30% of patients with advanced cancer still have recalcitrant pain, despite optimised use of systemic analgesics. In these cases, the special skills of PPs to perform interventions for pain relief may be utilised.[8] PPs are responsible for managing cancer pains in a majority of hospital set-ups which have facilities to access various modalities of cancer treatment but lack Specialist PCPs and services. This is therefore, an area where motivating PPs to add on PC in their practice could be considered as the right step because they could be instrumental in achieving the goal of comprehensive cancer care in their institutions.
In India, since only a few medical colleges have been successful in establishing PC as a speciality,[9] the turn-over of specialist doctors is also low. One way to overcome this deficiency would be to conduct short and frequent training programs in PC that seeks to empower interested specialists of other disciplines.
This survey was conducted with the objective of obtaining views of PPs about PC. The response from the PPs was not satisfactory. We had <10% responses, despite encouraging even those not practising PC to respond so as to identify reasons for their disinterest. There could be many reasons for the poor response we had (93%). PPs may not be interested in PC or they may not be interested in surveys or they may be uncomfortable in responding to some items in the SQ. However, the disinclination to respond to our survey was too large to be dismissed as disinterest in surveys or a lack of comfort level in responding to questions; it probably reflects more, a general apathy or lack of awareness about PC. Response to surveys about PC has generally been poor in India. In a survey at a leading Indian medical institution, only 186 of 2800 (6.64%) doctors responded to a survey about awareness and knowledge of PC.[10] Kelly et al. (2003), in their publication that described the good practices of conducting and reporting a survey research, claimed that questionnaire-based surveys are usually received “cold” and the response rate is low ≈ 20%.[3]
Among the respondents to our survey, only 14 were practising CPM for more than 10 years while the rest had been practising for 5–10 years. More than half were already involved in the practice of PC. A third would have liked to practise PC. Apart from the categorical responses of “practising” and “do not want to practise” that showed aptitude, we received four responses as “unable to practise PC” which implied there could be other contributory factors despite interest. We also observed that although eight respondents categorically said that they did not want to practise PC, they still showed interest by participating in the survey.
When responses were specifically sought for the number of years of PC practice, seven respondents who had practised PC, as claimed in the earlier question, refrained from giving the specific duration that they had practised it for. This suggested that they might have discontinued PC practice – the reasons perhaps would have been chosen in the question that discussed barriers.
More than three-fourths showed interest and inclination to practise PC – an encouraging trend! Half of them felt that they had the necessary aptitude to practise PC while a few indicated a personal reason like inner calling or exposure to a cancer death in the family which motivated them. Some had both – the necessary aptitude for PC as well as exposure to personal factors. Two respondents, despite having both, were unable to practise PC.
Half of the respondents were practising PC – few of whom seemed to be practising despite obstacles. The other half cited various reasons for poor motivation to practise PC but there was no single dominant factor. Lack of knowledge and skills and stress in practice were major reasons cited. Sparse referrals and poor financial incentives were the dampeners for some. Lack of space, infrastructure and teams was another reason cited. Some cited inability to find time to get trained and acquire the requisite knowledge and skills.
In response to the item, where the respondents self-assessed their competency in PC, 62.3% respondents had the requisite “knowledge” but half of them claimed that they lacked the “skills.” About 27.6% respondents agreed that they had neither knowledge nor skills and 10.8% were steadfast in not wanting to consider PC. From the responses, it appeared that the participants had significant gaps in knowledge and skills in several key areas of PC such as spirituality, end-of-life issues and addressing of care-giver issues.
In a survey conducted among 375 doctors working with the Indian Border Security Force, Butola (2014)[11] found that 75.5% of the overall 56% responses received reflected lack of awareness of the basic concept of PC and hence, was the most important barrier. This is in contrast to only 15% of the respondents in our survey who said that they were deficient in their knowledge about PC. This could probably be because our survey involved the opinion of a specialised cohort. Likewise, the level of awareness and knowledge was found to be high among anaesthesiologists who were the maximum respondents (50% of 186 physicians) in a survey conducted at an apex tertiary care cancer hospital in India.[12] The analysis of that survey even showed that when the responses were segregated according to the hierarchical status of the medical professionals, 50% were Senior Residents (younger age group) of which 50% were anaesthesiologists.
Overall, in our survey, more than three-fourths of the respondents showed inclination towards gaining education in PC. This is similar to the figures seen in the survey conducted by Patel et al. (2019)[12] where 75% of 186 respondents belonging to different medical disciplines evinced interest in getting educated in PC.
A majority of the PPs chose institutional courses to gain more knowledge and skills, perhaps reflecting a need for a more customised and integrated curriculum.[10,13-15] Half of them wanted the training period to be less than 3 months. A small percentage was ready to invest more time. The challenge for curriculum developers lies in providing adequate knowledge and hands-on skills in a short duration, especially since all the respondents were already practising pain management. In a survey that was conducted to assess the acceptability of online training in PC, substantial interest was reported by Kiss-Lane et al. (2019).[16]
One third of the respondents in this survey felt that PC was not financially viable. An equal number; however, felt that it was viable. In an increasingly commercialised medical practice, this aspect probably has an important bearing for medical graduates who are in the process of choosing a specialisation.[9,15,17] To most practitioners of PC, striking a balance between providing quality patient care and getting appropriate remuneration is always a subtle, ethical dilemma.[18] The PPs can probably surmount this dilemma by continuing the more remunerative chronic pain management practice while at the same time providing quality PC.
Bhatnagar et al. (2016) proposed an Integrated Pain and Palliative Medicine model applicable at different levels of health care in India. Its basis appeared to be solely, the symptom of pain which was seen to be an indicator of the need and outcome measure of PC. Similarly, in a survey conducted by Bhadra et al., (2013),[19] about 74% of 648 respondents who were specialists in various disciplines believed pain control to be the primary aim of PC.
The objectives of PC are, however, multidimensional and are not limited to the management of pain. The WHO specifies in its definition of PC that it is “an approach towards patients with life-threatening illness and their care-givers” which focuses on “prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.” As indicated in our survey, half of the PPs had successfully integrated PC in their practice. There was a significant degree of motivation in the rest. In our opinion, the initial contact with cancer patients while managing their pain can be considered as a starting point for making an attitudinal change towards considering rendering holistic PC also. A complete integration of all aspects of PC with CPM may be of large benefit to society and policymakers may find it easier to make PC available more widely.
In an informal survey, we found that there are approximately 18 corporate and private hospitals in Bangalore, a city of 1.2 core population. 15 have Oncological services, nine have chronic pain management services; but only five have Specialist PC services of which, one has the Medical Oncology team rendering PC. Among the 11 private medical colleges and one government medical college, only two private medical colleges have PC services. There is only one hospice with Specialist PC services. There are three private pain clinics- none of which offered PC services; there are two rehabilitation centres which have PC services but are managed by Generalist PCPs. This survey is indicative of the paucity of PC services in even urban centres where cancer care is widely available.
An obstacle to this impending integration at all levels of health-care or at all levels of health-care providing set-ups is probably the revenue generating potential of PC services. There is a large category of patients who choose to pay for curative treatments of cancer as is evidenced by growth of cancer specialties in corporate and private hospitals. Although many of these practice settings avail the services of PPs, they do not encourage PC services because of concerns about costs and returns. There is ample evidence to suggest that PC services complement and add value to overall cancer services even when patients are undergoing specific treatments for the underlying diseases. PC is underutilised even by cancer specialists due to reservations and prejudice. It should be noted that this category of patients may be willing to spend on PC services as well.
India is a vast country and the availability of PC services is a problem identified by many experts and policy makers in the field. Jain (2018) while discussing the prospects of PC in India has said < 2% of our population has access to PC.[20] Services need personnel and in this context, it is probably essential to identify which other allied medical fields can integrate PC practise and then, adopt ways to assess the inclinations in the personnel belonging to these fields. The final end-point, however, will be the assessment of knowledge and competencies of the interested and have methods of filling gaps or enhancing skills in the identified domains.
Our survey focussed on PPs. PPs render expertise in managing complex pain syndromes with analgesics and/or procedural interventions. On the other hand, PCPs largely depend on the WHO ladder for managing all types of cancer pain. Opioids are known to cause undesirable side effects that affect the QoL. This adds on to the already existing poor QoL affecting patients in advanced stages of the disease. Procedural interventions for pain are known to quickly reduce pain by virtue of being more site-specific. It thereby allows a reduction of drug dose and its side-effects.
The World Health Assembly adopted a resolution, “Strengthening of PC as a component of comprehensive care throughout the life course” in May 2014. It recommended integration of PC into core health systems for all ages and diseases. However, Gomez-Batiste et al. (2017), in their manual of guidelines prompted the WHO about the lack of global information on education and training plans in PC.[15] They have pointed out that the core concepts of PC should be inserted in undergraduate and postgraduate curricula and, proposals should focus on achieving “specialisation” status as well as directives to accommodate other allied disciplines which have specific competencies relevant to PC. They conclude that the ultimate outcome consequent to “change” in the four targets – attitudes, knowledge, skills and behaviour should impact patients, families, organisations and society.
With regard to the concluding question in our survey, a majority of the respondents felt that a multi-disciplinary team in PC was only partially feasible. True to the prevailing circumstances, it will be difficult to motivate fulltime participation of various specialists in PC teams. At best, it is likely to be a part of larger multidisciplinary care set-ups like medical institutions.
CONCLUSION
We conducted this national-level survey to assess the attitudes-aptitudes-barriers-knowledge of PPs towards PC. The sample size is admittedly small. We expected a significant response rate given the fact that the bio-psycho-social model is the working principle for PPs too and hypothesised that many would show interest in the practice of PC and if not, would at least participate and enable us to identify barriers. Many who participated in the survey were already practising PC which introduced another element of bias.
While a search of literature did not yield qualitative information as to what motivates a physician towards PC, it would still be interesting to know the influencing factors such as demographics (age, gender, urban/rural, institution/private and hierarchical position in practice) and dispositional characteristics of medical practitioners. This was a limitation of our survey too – we did not collect any data that would help us understand the impact of demographics/disposition.
The global scenario is similar. Policy-makers, from regional to global levels are strategizing on options to popularising PC since it supports the dualistic model of cure and care that are necessary for both, chronic-debilitating or life-limiting illnesses. Hence, on the concluding note we feel that a larger survey targeting the unresolved questions about the acceptability of PC among PPs may help in tapping the large pool to expand the scope of availability of PC services.
Acknowledgements
Dr Balabhaskar, Dr Pradeep Dongare, Dr Lakshmi Vas, Dr Mary. Abraham, Dr Raghu Thota, Indian Society for Study of Pain, the consultants who gave their expert opinion and all the survey respondents. We also wish to acknowledge Mrs Arathi Bhargav for editing the manuscript.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Aspiring pain practitioners in India: Assessing challenges and building opportunities. Indian J Palliat Care. 2018;24:93-7.
- [Google Scholar]
- Pain and symptom management in palliative care and at end of life. Nurs Outlook. 2012;60:357-64.
- [CrossRef] [Google Scholar]
- Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003;15:261-6.
- [CrossRef] [Google Scholar]
- Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30:459-67.
- [CrossRef] [Google Scholar]
- Developing criteria for establishing interrater reliability of specific items: Application to assessment of adaptive behavior. Am J Ment Defic. 1981;86:127-37.
- [Google Scholar]
- Statistical methods for rates and proportions (2nd ed). New York: John Wiley; 1981.
- [Google Scholar]
- Cancer pain: Treatment overview In: Mc Mahon SB, Koltzenburg M, eds. Wall and Melzack's Textbook of Pain (5th ed). Edinburgh: Elsevier Churchill Livingstone; 2006. p. :1141-57.
- [Google Scholar]
- Integrated pain and palliative medicine model. Ann Palliat Med. 2016;5:196-208.
- [CrossRef] [Google Scholar]
- A study on knowledge, attitude, and practices regarding palliative care among doctors in border security force. Prog Palliat Care. 2014;22:272-9.
- [CrossRef] [Google Scholar]
- A survey of medical professionals in an apex tertiary care hospital to assess awareness, interest, practices, and knowledge in palliative care: A descriptive cross-sectional study. Indian J Palliat Care. 2019;25:172-80.
- [CrossRef] [Google Scholar]
- Board certification in palliative care for U.S. physicians. Officers and trustees of the American board of hospice and palliative medicine. J Pain Symptom Manage. 1999;17:309-10.
- [Google Scholar]
- Official certification of doctors working in palliative medicine in Europe: Data from an EAPC study in 52 European countries. Palliat Med. 2007;21:683-7.
- [CrossRef] [Google Scholar]
- Building Integrated Palliative Care Programs and Services London, England: Worldwide Hospice Palliative Care Alliance; 2017.
- [Google Scholar]
- Palliative care clinicians and online education in India: A survey. BMJ Support Palliat Care. 2019;9:e35.
- [Google Scholar]
- Pain services and palliative medicine-An integrated approach to pain management in the cancer patient. Br J Pain. 2014;8:163-71.
- [CrossRef] [Google Scholar]
- A Call for Integrated and Coordinated Palliative Care. J Palliat Med. 2018;21:S27-9.
- [Google Scholar]
- Awareness of palliative care among doctors of various departments in all four teaching medical colleges in a Metropolitan city in Eastern India: A survey. J Educ Health Promot. 2015;4:20.
- [CrossRef] [Google Scholar]
- Palliative care in India: Trials, tribulations, and future prospects. J Mahatma Gandhi Inst Med Sci. 2018;23:55-8.
- [CrossRef] [Google Scholar]






