Translate this page into:
A Rare Case Report: Carcinoma Pancreas with Hepatocellular Carcinoma
Address for correspondence: Dr. Vikas Yadav; E-mail: drvikasyadav@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Synchronous double malignancies involving different organs are relatively rare and uncommon finding. We report an interesting case of double malignancy in which a patient exhibited synchronous two separate carcinomas, pancreatic and hepatocellular carcinoma (HCC). Patient was a 64-year-old male who presented primarily with symptoms pertaining to the biliary obstruction and ultrasound of abdomen revealing pancreatic head mass. HCC was detected incidentally during the investigations for carcinoma pancreas.
Keywords
Hepatocellular carcinoma
Pancreatic carcinoma
Synchronous double malignancy
INTRODUCTION
Due to the aid of modern radiologic diagnostic tools, mass screening, increasing patient age and improving survival rates for patients with neoplastic disease, there has been an increase in the rate of detection of multiple synchronous and metachronous primary cancers. Synchronous double primary malignant tumor of pancreas and liver has never been reported in review literature. Here is a case with synchronous pancreatic head carcinoma and hepatocellular carcinoma (HCC).
CASE REPORT
The present case report is about a 64-year-old diabetic, non-alcoholic male patient who visited our hospital with the chief complaint of anorexia, malaise and icterus since 2 months for which he was evaluated outside with routine blood investigations showing raised serum bilirubin (6.5 mg/dl) and ultrasound reporting of hypo echoic mass (28.7 mm × 33 mm) in the head of pancreas.
There was no remarkable family history. On admission, patient was in good general health and vital signs were within the normal limits. On physical examination, the sclera was icterus. The abdomen was soft, but tender in the right upper quadrant. Routine blood examination showed the following: White blood cell, 10,200 cells/uL; hemoglobin, 12.1 g/dl; platelet, 218,000/mm3; blood glucose, 209 mg/dl; total bilirubin, 10.2 mg/dl; direct bilirubin, 6.2 mg/dl; alkaline phosphatize, 271 IU/l; serum glutamic-pyruvic transaminase, 101 IU/l; serum glutamic-oxaloacetic transaminase, 67 IU/l; and gamma-glutamyl transpeptidase, 343 IU/l. Viral markers were negative. Tumor marker assays showed raised alpha-fetoprotein 51.99 ng/ml (normal 0-8.5), carcinoembryonic antigen was 4.2 ng/ml (normal 0-5) and carbohydrate antigen 19-9 (CA 19-9) was markedly raised 65,919 U/ml (normal 0-37).
A triple phase contrast enhanced computed tomography (CT) scan of the abdomen revealed 3.5 cm × 3.2 cm × 4.0 cm hypo-enhancing mass in the pancreatic head with upstream extrahepatic and bilobar intrahepatic biliary radicles dilatation [Figure 1a], multiple small peripancreatic and mesenteric nodes. Liver showed multiple nodular lesions (metastasis) of varying sizes with differential characteristics [Figure 1b], one of the large relatively defined mass in segment 7 of the liver is showing subtle arterial phase enhancement [Figure 1c] and washout in portal venous phase [Figure 1d] likely HCC. Upper gastrointestinal endoscopy was normal.

- Heterogenous ill-defined soft-tissue attenuation mass involving the pancreatic head and uncinate process (a) with multiple liver metastases (b) incidentally noted one of the large relatively defined mass in segment 7 of the liver is showing subtle arterial phase enhancement (c) and washout in portal venous phase (d) likely hepatocellular carcinoma
Thus, the provision diagnosis was carcinoma head of pancreas with multiple liver metastases synchronous with HCC? Ultrasonography guided fine-needle aspiration was taken from pancreatic mass, non-enhancing and enhancing liver SOL for confirmation.
On microscopic examination
-
Smears from the enhancing liver lesion was hypercellular, comprise thickened trabeculae and groups lined by atypical hepatocytes with transgressing blood vessels and partial entrapment by endothelial cells at the periphery. There were few stripped nuclei seen in the background. The atypical hepatocytes show enlarged, hyperchromatic, markedly pleomorphic nuclei with irregular distribution of nuclear chromatin, prominent eosinophilic nucleoli, focal nuclear vacuolization and abundant granular eosinophilic cytoplasm with cholestasis [Figure 2a–c]. On immunohistochemistry-Tumor cells was positive for glypican 3 and hepatocyte specific antigen [Figure 2d]. Histochemistry-trabeculare are reticulin poor. Above features are diagnostic of HCC
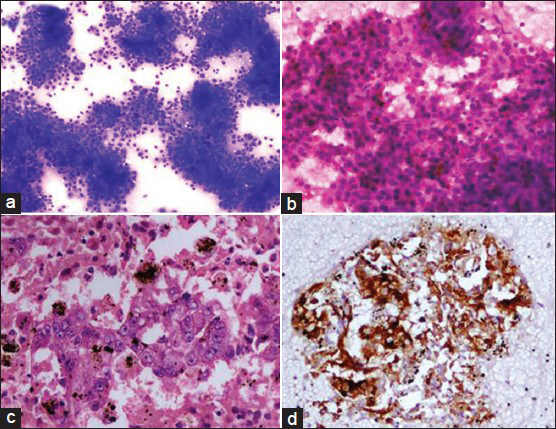 Figure 2
Figure 2- Fine-needle aspiration from the enhancing liver lesion. (a) Cellular smear with thickened trabeculae (Geimsa stain, ×100) (b) thickened trabeculae with vascular transgression, partial endothelial wrapping, bile stasis and malignant nuclear features of hepatocytes (H and E, ×200) (c) cell block preparation showing malignant hepatocytes with bile stasis (H and E, ×200) (d) cell block preparation with glypican 3 positivity (×200)
-
Smears from the non-enhancing Liver lesion showed few small groups and acini of atypical epithelial cells, admixed with sheets and clusters of benign hepatocytes. These atypical epithelial cells show enlarged, hyperchromatic, markedly pleomorphic nuclei with high N:C ratio, irregular nuclear membrane, coarse chromatin and scanty cytoplasm suggestive of metastatic adenocarcinoma [Figure 3a].
 Figure 3
Figure 3- (a) Fine-needle aspiration from other liver lesion showing metastatic adenocarcinoma (large arrow) closely admixed with benign hepatocytes (small arrow) (Geimsa stain, ×200) (b) FNA from pancreatic head mass showing adenocarcinoma (Geimsa stain, ×200)
-
Smears from the pancreatic lesion showed few small groups and acini of atypical epithelial cells. These atypical epithelial cells show enlarged, hyperchromatic, markedly pleomorphic nuclei with high N:C ratio, irregular nuclear membrane, coarse chromatin and a fair amount of vacuolated cytoplasm suggestive of adenocarcinoma [Figure 3b].
Patient was diagnosed as carcinoma pancreas with multiple liver metastases synchronous with solitary HCC. The conclusive stage of the pancreatic cancer was TNM stage IV {T2, N1, M1} whereas that of the HCC was Barcelona Clinic Liver Cancer (BCLC) stage A and TNM stage I {T2, N0, M0} according to Union for International Cancer Control classification. Percutaneous transhepatic biliary drainage followed by metallic stenting was done and planned for single agent gemcitabine based palliative chemotherapy once total serum bilirubin came down below 3 mg/dl.
DISCUSSION
In reviews of the literature the overall frequency of multiple primary malignancies is between 0.73% and 11.7% respectively.[1] There are several proposed contributing factors toward multiple malignancies i.e. heredity, constitution, environmental, immunological, carcinogenic viruses, radiological and chemical treatments factors[2] but still exact mechanism is not clear. It is very important to rule out metastasis before labeling multiple primary malignancies.
Incidence of pancreatic cancer associated with other organ malignancies is 1.2-20.0%, with malignancies predominately of the stomach, colon, thyroid and genitourinary tract.[3456] However, synchronous carcinoma head of pancreas and HCC never reported in review literature.
Pancreatic carcinoma is one of the most aggressive malignancies with overall 5 year survival below 5%.[7] Mainstay curative treatment for pancreatic carcinoma is surgery which is possible in less than 20% of patients.[8] Nearly 80% of pancreatic carcinoma present with either locally advanced unresectable or with distant metastasis and managed with palliative chemotherapy with or without radiotherapy.
HCC mainly present with underlying cirrhosis in more than 90% of the case.[9] Treatment strategy is tailored on the basis of the extent of tumor burden and underlying liver reserve. Curative treatment options for HCC are resection, transplantation and percutaneous ablation and are reserved to selected patients bearing an early or very early HCC. Only 30-40% of patients with a newly diagnosed HCC can undergo curative treatments in the west.[10] Liver transplantation is the only definitive treatment for both HCC and the underlying liver disease with 5 year survival rates exceeding 70% with Milan Criteria. Surgical resection is reserved to single lesion with preserved liver function and without portal hypertension with survival of more than 70% at 5 years.[11] HCC patients who are not suitable for curative treatment the survival is very poor.
The prognosis of patients with multiple primary malignant malignancies should be determined independently by the stage of each malignancy. For treatment purpose most aggressive and advanced cancer to be addressed first. The prognosis of patient in our case will depend on the behavior of pancreatic carcinoma.
In our case, only single lesion (size less than 3 cm) of HCC was detected on imaging and staged as BCLC stage A. As per BCLC guidelines treatment for small solitary HCC lesions (BCLC Stage O and A) is hepatic resection or radiofrequency ablation or liver transplant with a median 5 year survival of nearly 70%. Carcinoma pancreas is more advanced with multiple liver metastases in our case and has a poor prognosis with average survival of 6 months. In such situation, it is not advisable to treat HCC with a radical approach. Until date only Sorafinib is approved for palliate treatment in an advanced stage (BCLC stage C). Gemcitabine is a standard drug for metastatic pancreatic carcinoma and also have some advantage in HCC in phase II trials.[12131415] No literature available on the combination of Sorafinib with Gemcitabine and also theoretically it will be a very toxic regimen and hence single agent Gemcitable is planned in our case.
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Multiple primary malignant neoplasms: Case report and a comprehensive review of the literature. Am J Clin Oncol. 2003;26:79-83.
- [Google Scholar]
- Synchronous triple early cancers occurring in the stomach, colon and gallbladder. Asian J Surg. 2003;26:46-8.
- [Google Scholar]
- Study of cases with double carcinoma of the stomach and pancreas. Jpn J Cancer Clin. 1977;23:1306-14.
- [Google Scholar]
- A case of synchronous double cancers of the pancreas and stomach. Kurume Med J. 2000;47:169-71.
- [Google Scholar]
- Clinical significance of multiple cancers including pancreatic cancer: Report on 12 cases. Gan No Rinsho. 1982;28:165-7.
- [Google Scholar]
- Synchronous or metachronous double cancers of the pancreas and other organs: Report on 12 cases. Surg Today. 2000;30:718-21.
- [Google Scholar]
- Hepatocellular carcinoma: Rising incidence, changing therapeutic strategies. Wien Med Wochenschr. 2006;156:404-9.
- [Google Scholar]
- Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: Resection versus transplantation. Hepatology. 1999;30:1434-40.
- [Google Scholar]
- Prospective randomised phase II study of gemcitabine at standard or fixed dose rate schedule in unresectable hepatocellular carcinoma. Br J Cancer. 2003;89:1865-9.
- [Google Scholar]
- A phase II trial of gemcitabine in patients with advanced hepatocellular carcinoma. Cancer. 2002;94:3186-91.
- [Google Scholar]
- Treatment of advanced hepatocellular carcinoma with biweekly high-dose gemcitabine. Oncology. 2001;60:313-5.
- [Google Scholar]
- Phase II study of gemcitabine in patients with advanced hepatocellular carcinoma. Cancer. 2000;89:750-6.
- [Google Scholar]






