Translate this page into:
Psychiatric Morbidity, Pain Perception, and Functional Status of Chronic Pain Patients in Palliative Care
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Psychological factors, such as that exist when we experience pain, can profoundly alter the strength of pain perception.
Aim:
The study aims to estimate the prevalence of psychiatric disorders, and its association with perception of pain and functional status in chronic patients in palliative care.
Materials and Methods:
The sample was selected via simple randomisation and post consent were assessed using (1) a semi- structured questionnaire to elicit socio-demographic information and medical data (2) Brief Pain Inventory (3) ICD-10 Symptom Checklist (4) ICD-10-Diagnostic Criteria for Research (DCR) (5) Montgomery Asberg Depression Rating Scale (MADRS) (6) Covi Anxiety Rating Scale (7) Karnofsky Performance Status Scale. Data was analysed using independent sample t test and chi square test.
Results:
The psychiatric morbidity was 67% with depression and adjustment disorders being the major diagnosis. There was a significant association between psychiatric morbidity pain variables (P = 0.000). Psychiatric morbidity significantly impaired activity, mood, working, walk, sleep, relationship, and enjoyment. There was no association between aetiology of pain, type of cancer, treatment for primary condition and treatment for pain and psychiatric morbidity. The functional status of cancer patients was also poorer in patients with psychiatric morbidity (P = 0.008).
Conclusion:
There is a high prevalence of psychiatric illness in chronic pain patients of any aetiology. Psychiatric morbidity is associated with increased pain perception, impairment in activity and poor functional status.
Keywords
Cancer
Depression
Functional status
Pain perception
Psychiatric morbidity
INTRODUCTION
Psychological factors, such as the situational and emotional factors can profoundly alter the strength of pain perception. Consequently, the understanding of pain requires not only understanding of the nociceptive system, but recognition and control of the many environmental and psychological factors that modify human pain perceptions.[1] Chronic pain is defined as one present for more than half of the days of at least a 90-day period.[2] Studies have reported that psychiatric illness varies in chronic pain sufferers and a study of such a group showed that 98% of cases had a Diagnostic and Statistical Manual of Mental Disorders (DSM)-III R diagnosis.[3] Depression has been noted in many studies on pain patients.[4],[5] Results of a study on 215 randomly accessed cancer pain patients indicated that 47% of the patients received a DSM-III diagnosis. Approximately 68% of the psychiatric diagnoses consisted of adjustment disorders, with 13% representing major affective disorders (depression).[6] Review of studies show that the perception of pain in depressed cohorts and depression in pain cohorts are higher than when these conditions are individually examined. Depression and pain share biological pathways and neurotransmitters, which has implications for the treatment of both concurrently.[7] This study aims to estimate the prevalence of psychiatric disorders, and its association with perception of pain and functional status in chronic pain (both cancer and other etiologies), patients attending the outpatient wing of a palliative care clinic.
MATERIALS AND METHODS
The sample was selected via simple randomization by selecting patients with even number from among the patients attending the outpatient Department of Pain and Palliative Care Clinic in Calicut Medical College, Kerala, India. The inclusion criteria were: (1) Patients above age 18 years satisfying the criteria for chronic pain and (2) patients able and willing to give informed consent. The exclusion criteria were: (1) Patients with gross mental retardation or any neurological deficit interfering with the accurate recording of information including dementia and delirium, (2) patients without any identified organic cause for pain, and (3) patients with past history of psychiatric illness (i.e., preceding the onset of pain).
The patients post consent was assessed using (1) a semistructured questionnaire designed to collect sociodemographic information and medical history. (2) Brief Pain Inventory Short Form (BPISF), devised by Charles S. Cleeland, PhD (1991).[8] The tool has nine questions and the ninth question has seven subquestions from A to G. (3) International Classification of Diseases (ICD)-10 Symptom Checklist,[9] a semistructured instrument to record the clinicians’ assessment of psychiatric symptoms and syndromes in F0-F6 categories of the ICD-10 classification of mental and behavioral disorders. The interviewer reliability was found to be high (kappa value = 0.72). (4) ICD-10 Diagnostic Criteria for Research (DCR),[10] provides specific criteria for the diagnosis contained in Clinical Description and Diagnostic Guidelines (CDDG) which was produced for clinical and educational use. (5) Montgomery Asberg Depression Rating Scale (MADRS) developed by Montgomery and Asberg (1979).[11] It has ten items; each rated on a 4-point scale. (6) Covi Anxiety Rating Scale (CARS) devised by Lipman et al. (1979).[12] It is composed of three items. Each item scores on a 5 point (0-4) scale: 0-absent, 1-mild, 2-moderate, 3-severe, and 4-very severe. (7) Karnofsky Performance Status Scale[13] is a numerical scale devised to quantify the patient status in carrying out normal activities and self-care. Devised in 1948 by Karnofsky and Burchenal, it has 11 scores from 0 to 100. Its validity and reliability as an indicator of functional status has been established.[13] Statistical analyses of the variables are done using independent sample t-test and Chi-square test. The data was analyzed using SPSS 15 for Windows (SPSS Inc., 2005).[14]
RESULTS
A total of 176 patients (N = 176) were screened and among them 33 (18.8%) patients did not consent for the study. The most common reasons were increased fatigue and weakness, length of the interview, and stigma related to psychiatric interview. Further, 43 patients had to be excluded based on the exclusion criteria, of this 15 patients were excluded due to acute medical problems intervening with interview, 12 were excluded due to the fact that they did not satisfy the criteria for chronic pain, four were excluded due to delirium, eight were excluded as they had undergone tracheostomy or tongue resection and were unable to give information, and one patient was mentally retarded. So a total of 100 patients (N = 100) were included in the study and data was collected from them.
The sample consisted of 67 males and 33 females, with a mean age of 51.23 years (standard deviation (SD) =12.6). Majority of the cases were from a low socioeconomic status (82%). Seventy-six percent of the sample was married and 11% was unmarried, while the rest were widowed or divorced/separated (13%). Eighty-three percent belonged to a rural background while 17% were urbanites. Of the sample, 66% had cancer pain while 34% had pain due to a noncancerous etiology. Of the cancer patients, 16% had a family history of cancer. Lung cancer was the most common cancer in the group (25.7%) followed by oral cancer (10.6%), stomach cancer (10.67), breast cancer (9.1%), and pharyngeal carcinoma (6.1%). Of the noncancerous etiology, intervertebral disc prolapse (IVDP) formed the major diagnostic group (55.9%) followed by peripheral vascular disease (PVD) at 21.6% and diabetic neuropathy at 8.8%. Fifty-seven percent of the patients were treated with opioid analgesics, 30% with opioids and adjuvants, and the rest with nonsteroidal anti-inflammatory drugs (NSAIDs) (9%) and adjuvants alone (4%). There was no difference between the cancer and noncancer pain groups in terms of sociodemographic variables.
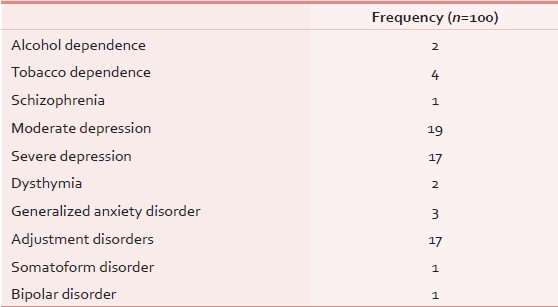
Sixty-seven percent of the sample had a psychiatric diagnosis with depression being the major diagnosis (36%) followed by adjustment disorders (17%) [Table 1]. The prevalence of alcohol and tobacco dependence as a comorbidity to another axis I disorder was 12 and 17% respectively, with 5% having dependence on both substances.
Forty-two males (69%) and 25 females (75.8%) had psychiatric diagnosis. The analysis of the data using Chi-square test showed that this difference among the groups was not significant (χ2= 1.71, P = 0.91). There was no association between socioeconomic status and psychiatric morbidity (χ2= 2.13, P = 0.64). Psychiatric morbidity did not show a significant association with marital status (χ2= 4.43, P = 0.22) There was also no significance in terms of age and psychiatric illness (t = 0.05, P = 0.95). Of the primary diagnosis, 46 (69.7%) patients with cancer and 21 (61.8%) patients with noncancer pathology had psychiatric morbidity. There was no significant difference among the cancer and noncancer pain group as far as the prevalence of psychiatric morbidity was concerned (χ2= 0.64, P = 0.42). However, a significant difference was seen in terms of the distribution of various psychiatric disorders [Table 2].

There was no association between the duration of pain and psychiatric morbidity. There was a significant association between the worst pain perceived and psychiatric morbidity (8.57 vs 7.51, t = 2.76, P = 0.000). Similarly, psychiatric morbidity was associated with a higher score on the least pain perceived (2.12 vs 0.94, t = 3.43, P = 0.000). The patients with psychiatric morbidity also had higher average pain scores (5.58 vs 4.52, t = 4.02, P = 0.000) and significantly high current pain score (4.28 vs 3.16, t = 2.77, P = 0.007). Pain relief experienced by patients with psychiatric morbidity was significantly lesser (71.34 vs 88.49%, t = −5.43, P = 0.000). Psychiatric morbidity was associated with a significant impairment of activity, mood, working, walk, sleep, relationship, and enjoyment [Table 3].

The duration of pain was significantly more in the noncancer group (19.8 months vs 10.6 months, P = 0.001). The pain variables did not vary between cancer and noncancer group. Sleep and enjoyment were significantly impaired in the cancer pain group [Table 4].

Psychiatric morbidity was independent of the type of cancer (χ2= 24.99, P = 0.41). Psychiatric morbidity did not show an association with the treatment offered for their primary condition and pain treatment [Tables 5 and 6]. There was also no significant difference in the pain treatment modalities offered for cancer or noncancer etiology [Table 7].



The functional status of cancer patients as measured by the Karnofsky score was significantly poorer in patients with psychiatric morbidity (58.04 vs 67.62, t = −2.73, P = 0.008).
DISCUSSION
Of the total 176 screened, 18.8% did not consent for the study and illness severity, perceived benefits, and discomfort of a lengthy interview contributed to this. A study shows that several aspects of the ethical design of clinical pain research that appear to be important to patients, including the potential benefits for subjects, the benefits for future patients, and the risks and burdens of research participation influence consent.[15] Patients also showed reservation to sign the consent form; a study done earlier shows that most patients think that the consent form is a legal document and thought it had medicolegal implications.[16]
Psychiatric diagnosis was present in 67% of the chronic pain patients. The results are similar to a study that showed 62% patients met ICD-10 diagnostic criteria for psychiatric disorder.[17] However it is much lower than a study on chronic pain which reported DSM-III diagnosis in 98%.[3] The results are slightly higher than the study done in a pain clinic population which showed that 32% of the patients had sufficient symptoms to be classified as psychiatric cases on the Present State Examination (PSE), a further 22% had minor neurotic symptoms and features of illness behavior.[7] The most common diagnosis was depression (36%), followed by adjustment disorder (17%). This differs from earlier studies which show that commonest diagnoses were organic disorders followed by neurotic and stress-related disorders and depression (27, 16, and 16%, respectively).[17] The incidence of depression is almost twice that was reported in the earlier study. This was however closer to another study which reported 29% depression in chronic pain.[18] The neurotic disorders prevalence in the current study (20%) however was similar to that in the study quoted (16%).
Dysthymia was also lower at 2%, while another study showed 7% prevalence.[18] Adjustment disorders constitute 25.4% of the psychiatric morbidity; this is far less than a report which showed that approximately 68% of the psychiatric diagnoses consisted of adjustment disorders.[3] Alcohol dependence (2%) was similar to earlier study which reported 2% prevalence.[18] Somatoform disorder (somatoform autonomic dysfunction) was seen only in 1% which was lower than an earlier study which reported 12% prevalence.[18] But this earlier study did not exclude psychiatric pain.
There was no significant association between any of the sociodemographic factors and psychiatric morbidity. Though a higher proportion of women had psychiatric illness (75.8%), this was not significant. Studies have reported higher psychiatric morbidity in women.[18],[19] There was no relation between domicile, marital status, and psychiatric diagnosis. This is in contrast to a report that psychiatric morbidity in pain is more in females, urbanites, and married.[20] Age did not show any significant difference among the two groups, but reports show increasing psychiatric morbidity with increasing age.[21],[22] There was also no significant difference in terms of the primary diagnosis of cancer and noncancerous pain in terms of psychiatric morbidity, and 69.7% of cancer and 61.8% of noncancer group had psychiatric illness. However, there was a significantly higher prevalence of depression in cancer group. This echoes the finding that patients whose pain is of cancerous origin report higher levels of cognitive and behavioral disturbances and feel more hopeless and worried.[23] Psychiatric morbidity is not associated with duration of pain; earlier study showed an increase of pain intensity fatigue psychological adaptation and disability with increased duration of pain, especially greater than 6 months.[24]
There was however a significant difference between the groups in terms of the pain intensity, pain relief, and all variables relating to functional impairment. This is corroborated by earlier studies which show that there is increased pain reported in patients with comorbid psychiatric disorder.[7],[25] In the subgroup of cancer pain, those with psychiatric morbidity showed lower Karnofsky scores. Similar findings have been reported in earlier studies.[26] However, the cause-effect relationship in terms of the relation between psychiatric illness and functional impairment is difficult to deduce due to their mutually contributory nature.
There was no significant difference among the groups in terms of the specific etiology for pain. There are no studies on chronic pain with varied etiology. There was also no difference in psychiatric morbidity with respect to the type of cancer. This contradicts an earlier meta-analysis that showed significant differences among groups of cancer patients with regard to tumor site in terms of psychiatric illnesses.[27] There was no difference also in terms of the treatment modalities like radiotherapy, chemotherapy, surgery, etc., among the groups. Studies have however reported that administration of chemotherapeutic agents is associated with depression and psychiatric morbidity.[28] There was also no significant difference among the groups in terms of the treatment modalities for pain. Studies show that corticosteroids which are used as adjuvants for pain treatment can result in psychiatric morbidity and opioids including morphine are drugs associated with dependence.[29] The study being directed to a clinic population, is not truly representative of chronic pain population. The study was limited by a small sample size and there is need for larger studies before the results can be generalized. The study excluded organic psychiatric illnesses like delirium and dementia due to obvious limitations in the eliciting of information regarding pain variables and functional status questions.
CONCLUSION
There is a high prevalence of psychiatric illness in chronic pain patients of any etiology (cancer and noncancer). Psychiatric morbidity significantly impairs activity, mood, working, walk, sleep, relationship, and enjoyment. Psychiatric morbidity is associated with increased pain perception, and also poor functional status. However, the cause-effect relationship in terms of the relation between psychiatric illness and functional impairment is difficult to deduce due to their mutually contributory nature. Psychiatric morbidity is not associated with type of cancer, treatment modality used for cancer, and treatment regimens for pain management. This study therefore puts forth the need for a closer assessment and treatment of psychiatric disorders, a very prevalent comorbidity of chronic pain. The improvement in pain perception and functional status offered by the treatment of psychiatric comorbidities can help instill greater self-esteem and independence in chronic pain patients. This would not only improve the treatment compliance and treatment outlook, but also has significant prognostic implications.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Narcotic maintenance of chronic pain. Medical and legal guidelines. Postgrad Med. 1983;73:81.
- [Google Scholar]
- Psychiatric illness and chronic low back pain: The mind and spine-which goes first? Spine (Phila Pa 1976) 1973:66-71.
- [Google Scholar]
- Multiple pains and Psychiatric disturbance An epidemiologic investigation. Arch Gen Psychiatry. 1990;47:239-44.
- [Google Scholar]
- The detection of psychiatric illness and psychological handicaps in a British pain clinic population. Pain. 1989;36:63-74.
- [Google Scholar]
- The prevalence of psychiatric disorders among cancer patients. JAMA. 1983;249:751-7.
- [Google Scholar]
- Depression and pain comorbidity: A literature review. Arch Intern Med. 2003;163:2433-45.
- [Google Scholar]
- The Brief Pain Inventory, Copyright 1991 Charles S. Cleeland, PhD Pain Research Group.
- ICD-10 Symptom Checklist for Mental Disorders (Version 1.1). Geneva, Division of Mental Health: World Health Organization; 1994.
- The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. Geneva: World Health Organization; 1993.
- A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382-9.
- [Google Scholar]
- Karnofsky and ECOG performance status scoring in lung cancer: A prospective, longitudinal study of 536 patients from a single institution. Eur J Cancer. 1996;32:1135-41.
- [Google Scholar]
- Statistical Package for Social Sciences Version 15. SPSS Inc. Chicago, IL: South Wacker Drive, 11th Floor; 60606-6412
- Beyond informed consent: The ethical design of pain research. Pain Med. 2001;2:138-46.
- [Google Scholar]
- Informed consent: Using a structured interview changes patients’ attitudes towards informed consent. J Laryngol Otol. 1993;107:775-9.
- [Google Scholar]
- The characteristic of persistent pain in psychological illness. J Psychosom Res. 1965;9:291-8.
- [Google Scholar]
- Comorbidity of pain-associated dysfunction and depressive symptoms in connection with sociodemographic variables: Results from a cross sectional epidemiological survey in Hungary. Pain. 2001;93:115-21.
- [Google Scholar]
- Psychiatric aspects of chronic intractable pain. Indian J Psychiatry. 1983;25:173-9.
- [Google Scholar]
- Adaptation to metastatic cancer pain, regional/local cancer pain and noncancer pain: Role of psychological and behavioural factors. Pain. 1998;74:247-56.
- [Google Scholar]
- Electronic diary assessment of pain, disability and psychological adaptation in patients differing in duration in pain. Pain. 2000;84:181-92.
- [Google Scholar]
- Evaluation of the relationship between depression and fibromyalgia syndrome: Why aren’t all patients depressed? J Rheumatol. 2000;27:212-9.
- [Google Scholar]
- Psychological sequelae of cancer diagnosis: A meta-analytical review of 58 studies after 1980. Psychosom Med. 1997;59:280-93.
- [Google Scholar]
- American Cancer Society Award lecture. Psychological care of patients: Psycho-oncology's contribution. J Clin Oncol. 2003;21:253-65s.
- [Google Scholar]
- Corticosteroids in cancer: Neuropsychiatric complications. Cancer Invest. 1989;7:479-91.
- [Google Scholar]






