Translate this page into:
A Retrospective Study of End-of-life Care Decisions in the Critically Ill in a Surgical Intensive Care Unit
Address for correspondence: Dr. Yi Lin Lee, Department of Anaesthesiology, Singapore General Hospital, 169608, Singapore. E-mail: yilin.lee@mohh.com.sg
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
Progress in medical care and technology has led to patients with more advanced illnesses being admitted to the Intensive Care Unit (ICU). The practice of approaching end-of-life (EOL) care decisions and limiting care is well documented in Western literature but unknown in Singapore. We performed a retrospective cohort study to describe the practice of EOL care in patients dying in a Singapore surgical ICU (SICU). The surgical critical care population was chosen as it is unique because surgeons are frequently involved in the EOL process.
Methods:
All consecutive patients aged 21 and above admitted to the SICU from July 2011 to March 2012, and who passed away in the ICU or within 7 days of discharge from the ICU (to account for transferred patients out of the ICU after end-of life care decisions were made and subsequently passed away) were included in the study.
Results:
There were 473 SICU admissions during this period, out of which 53 were included with a mean age of 67.2 ± 11.1 years. EOL discussions were held in 81.1% of patients with a median time from admission to first discussion at 1 day (IQR 0–2.75) and a median number of ICU discussion of 1 (IQR 1–2). As most patients lacked decision-making capacity (inability to retain and process information secondary to the underlying disease pathology or sedative use), a surrogate was involved: group decision in 27.9%, child in 25.6% and an unclear family nominated member in 20.9%. 28.3% of patients were managed as for full active with resuscitation, 39.6% nonescalation of care, and 32.1% for withdrawal. The main reasons for conservative management (nonescalation and withdrawal of care) were certain death in 52.3%, medical futility with minimal response to maximal care (27.3%), and the presence of underlying malignancy (18.2%). There was no significant difference between race or religion among patients for active or conservative management.
Conclusion:
71.7% of patients who passed away in the ICU or within 7 days of discharge from the ICU were managed conservatively. More timely, EOL discussions and better advance care planning may be needed to improve our patient care for patients on conservative management.
Keywords
Advance care planning
end-of-life
Intensive Care Unit
INTRODUCTION
With a globally aging population and changes in societal attitudes which places a greater emphasis on patient autonomy, the practice of end-of-life (EOL) care in the dying patient is poised for alterations. More frequently than not, the patient himself would not have indicated to his family any thoughts of how he envisions his life to end. This difficult decision is then left to the surrogate decision-maker. In an Asian society, talking about death is often regarded as taboo and frowned upon. Fortunately, this mindset is gradually changing, with the increased awareness of Advanced Medical Directives (AMDs) and legal power of attorneys. Singapore ranks 12th in the 2015 Quality of Death index, suggesting that as a nation, the manner of dying is important to us.[1]
The process of dying is usually a drawn-out process which frequently necessitates complex treatments. This results in increased health-care economics and stresses the health-care system. EOL care practices are greatly influenced by cultural, organizational, and religious differences.[23456] Singapore is a multiracial and cultural society and as such, these practices may vary widely with the different subset of patients we deal with. To determine if this is true, we performed a retrospective cohort study to describe the practice of EOL care in patients dying in a Singapore Surgical ICU (SICU). It is believed that this data will help to guide and improve end-of-life care in the intensive care setting by helping clinicians develop an EOL care model relevant to local values and practice in Singapore, so as to deliver rational and cost-effective critical care.
METHODS
Study design
The study was performed in the SICU of a tertiary public hospital (Singapore General Hospital) in Singapore. The SICU comprises a 10-bed unit in which all surgical patients with the exception of neurosurgical and cardiothoracic patients were warded in. The study center follows a closed model of care, led by a full-time intensivist Anesthesiologist. There is an on-duty specialist registrar at all times, and the nursing ratio was 1:1–2. The surgical critical care population was chosen as it represents a unique situation where the surgeons are frequently involved in the EOL process. Surgical "buy-in" is a concept described where surgeons discuss with high-risk patients their commitment to postoperative care before surgery. This can sometimes interfere with their care in the ICU as there may be differences in care goals with the intensivists.[7]
In our ICU, all admissions have to be approved either by the intensivist or on-duty specialist registrar. New admissions are cared for as for full active resuscitation until an EOL care decision was made by the intensivist and/or in conjunction with the family.
Ethics approval was obtained by the Local Ethics Committee. The requirement for informed consent was waived as no interventions or procedures were performed on patients.
Inclusion and exclusion criteria
All patients aged 21 and above admitted to the SICU, Singapore General Hospital, Singapore from July 2011 to March 2012, and who passed away in the ICU or within 7 days of discharge from the ICU, were included in the study. We chose to follow patients up to 7 days of discharge from the ICU as patients on conservative measures may be transferred out and pass away in the general ward after the EOL decisions are made.
Patients were excluded if they were < 21 years old or had missing case notes.
Definitions
In our ICU, we usually classify our goals of care as per the following:
-
Active management includes full resuscitation with or without cardiopulmonary resuscitation (CPR)
-
"Full with CPR": all interventions required to sustain life including the use of CPR, vasopressors, antibiotics, ventilation, and renal replacement therapy will be provided to the patient
-
"Full except CPR": as for "full with CPR" but CPR will not be administered
-
-
Conservative management includes withdrawal and nonescalation of therapy
-
"Nonescalation/Withholding": to avoid initiation of new therapy or escalation of existing treatment currently prescribed. CPR will not be performed
-
"Withdrawal": to stop all life-sustaining interventions that are being performed, but treatment aimed at palliation is allowed to continue.
-
The reasons for the above goals of care are divided into:
-
"Certain death": where death is imminent regardless of medical therapy administered
-
"Medical futility": deemed by the attending clinician to be when the patient does not have a realistic chance of response and may be applicable even when death is not imminent.
Data collection methods
Patients were identified from the SICU admission book and data were extracted from case sheets and electronic data by the investigators.
Baseline demographics including age, gender, race, religion, premorbid status, ICU length of stay, origin of admission (elective/emergency surgery, general ward, and emergency department) and systems-based chronic diseases were collected.
We obtained data about the type of ICU care provided to the patient (use of inotropes, presence of tracheostomy, administration of total parenteral nutrition (TPN), ventilator-assisted ventilation, use of renal replacement therapy, and transfusion of blood products) during the course of the patient's ICU stay as well as the care provided at the time of death.
Documented discussions with the patient and/or surrogate were recorded and information with regard to who the surrogate decision-maker was, which member(s) of the ICU team were involved, the mental capacity of the patient, presence of an AMD, patient's verbalized EOL care goals (if any), treatment goals, and their reasons were included in this study.
Statistical analysis
Statistical analysis was performed using IBM SPSS version 23 (Armonk, NY: IBM Corp). Patients were divided into active and conservative groups for subgroup analysis. Those in the active group included patients who were managed as for full with CPR and full except CPR while those in the conservative group included those who were managed as for nonescalation/withholding and withdrawal. Comparisons of categorical data and proportion were performed using the Chi-squared or Fisher's Exact Test when appropriate. Parametric continuous variables were compared using the Student's t-test. Nonparametric variables were compared using the Wilcoxon rank– sum test. Missing data were excluded from the analysis.
RESULTS
Patient characteristics
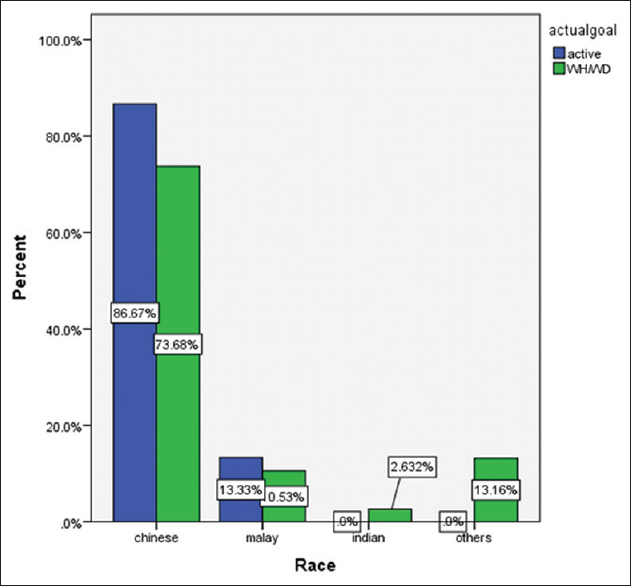
Four hundred and seventy-three patients were admitted to the ICU during the study period. Out of this, 53 patients were recruited in this study with a mean age of 67.2 ± 11.1 years with the baseline demographics shown in Table 1. Forty-one patients (77.4%) were Chinese with Buddhism the most common religion followed by Christianity. Most patients were independent (36 patients, 67.9%), living at home (40 patients, 90.1%) with their families (40 patients, 83.3%). The main spokesperson decreed at admission was their child (30 patients, 56.6%) and their spouse (15 patients, 28.3%). There was no difference in baseline characteristics between those who had active management and those who were treated conservatively.
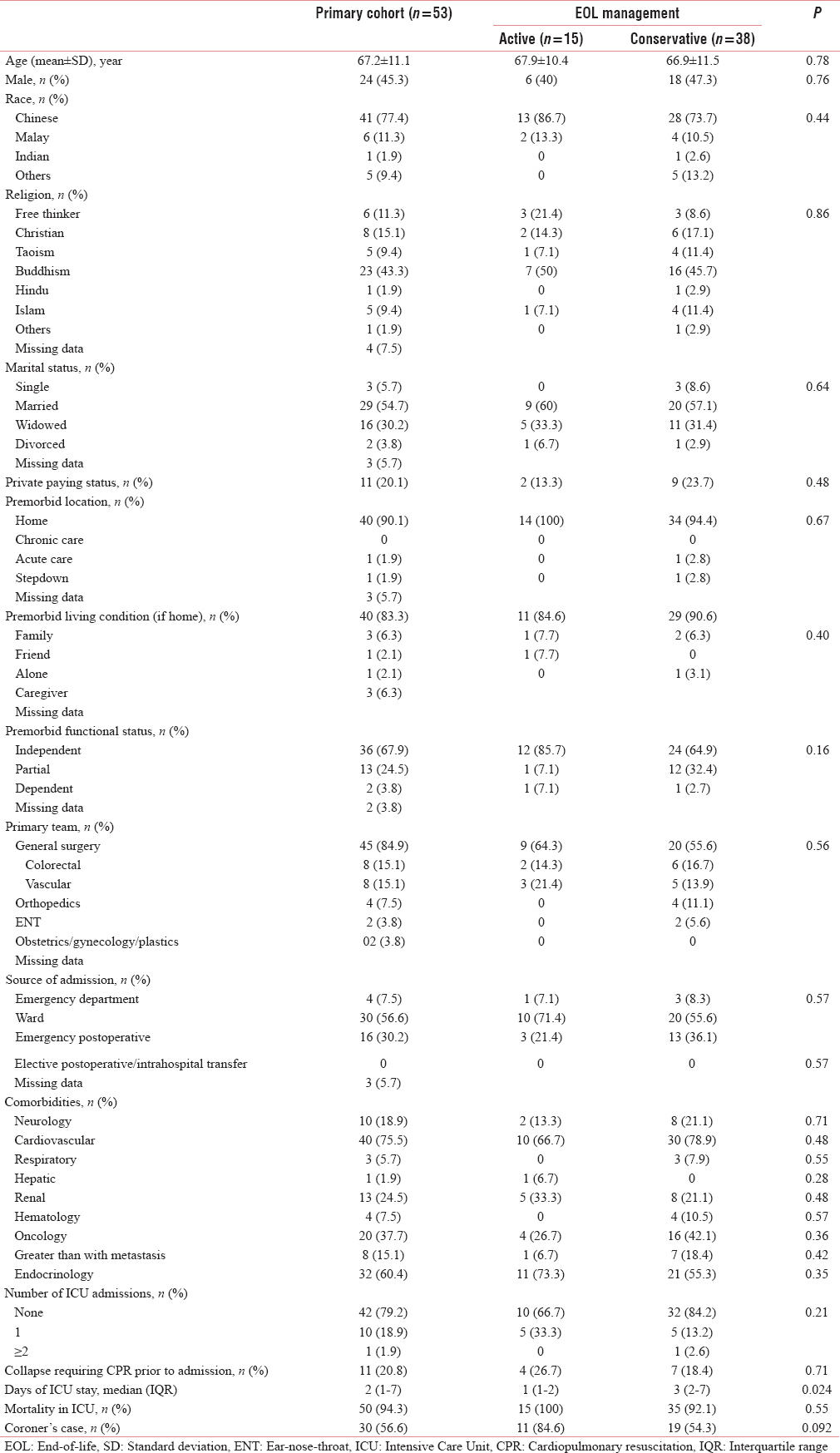
Forty-five patients (84.9%) of patients belonged to the general surgery discipline, and most admissions were directly from the ward (30 patients, 56.6%) and the emergency operating theater (16 patients, 30.2%). The comorbidities of the patients are listed in Table 2, and there was no difference in comorbidities in both groups. The number of ICU admissions and before ICU admission CPR did not affect if patients subsequently received active or conservative care. During their ICU stay, 51 patients (96.2%) received mechanical ventilation; 45 patients (84.9%) inotropic support; and 30 patients (56.6%) transfusion of blood products. The death occurred in the ICU in 50 patients (94.3%). The median length of stay to death in the ICU was 2 days (IQR 1–7). Patients who were in the active group were more likely to have a significantly shorter length of ICU stay and a higher likelihood of them requiring a coroner's inquiry compared to those in the conservative group.
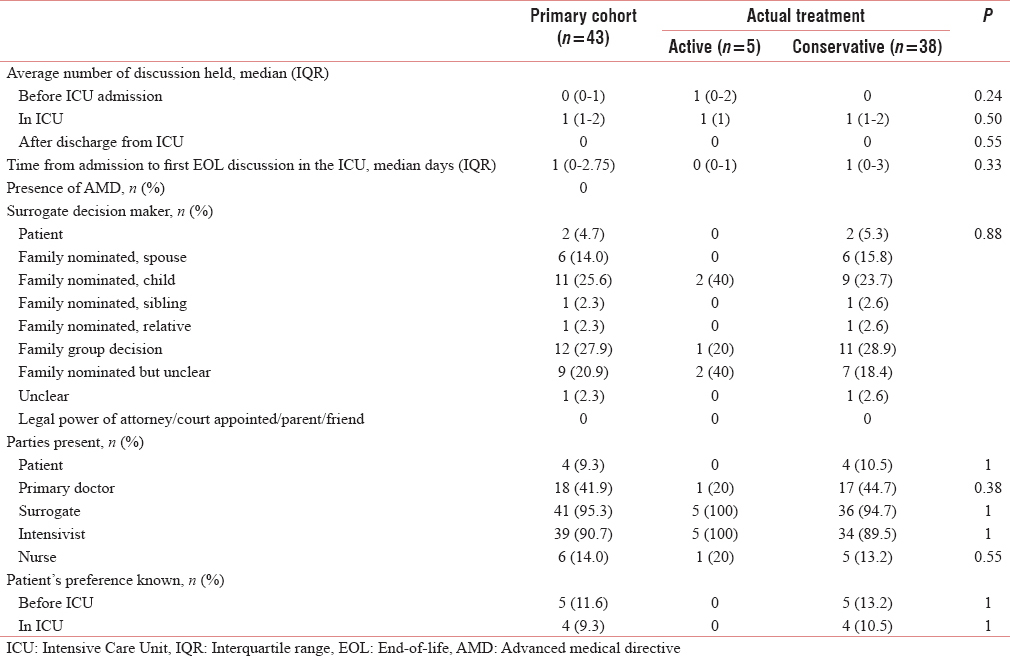
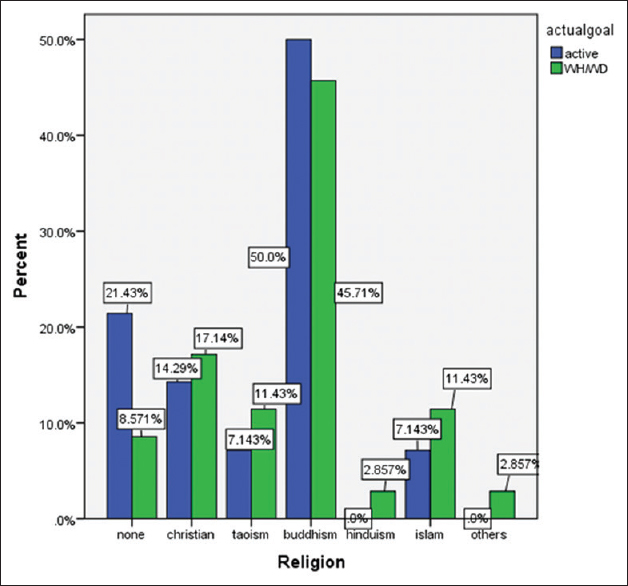
Frequency and types of end-of-life decisions
In our study, end-of-life discussions were held in 43 patients (81.1%) [Table 2]. Most discussions were held within the ICU itself with a median number of 1 (IQR 1–2), compared to before and after ICU admission where the median falls to 0. None of the patients studied had an AMD in effect. The surrogate decision-maker of the family was often a group decision (12 patients, 27.9%) followed by the child (11 patients, 25.6%) and an unclear family nominated member (9 patients, 20.9%). In these discussions, the intensivist was frequently involved (39 patients, 90.7%) although involvement by the primary team doctors was surprisingly low at 41.9% (18 patients), nursing at 14.0% (6 patients), and the patient at 4.7% (4 patients). Only 2 patients were documented to have preservation of their mental capacity in the ICU. Mental capacity was determined by the intensivist and involved the patient being lucid and able to retain information and communicate their thoughts. There was no difference in who the surrogate decision-maker was in both groups. Patients’ race and religion did not affect their EOL management [Figures 1 and 2]. Patients who had expressed their preference for EOL care were respected for it, and all belonged to the conservative group.
- Distribution of patients of religion to end-of-life management plan.
- Distribution of race to end-of-life management plan.
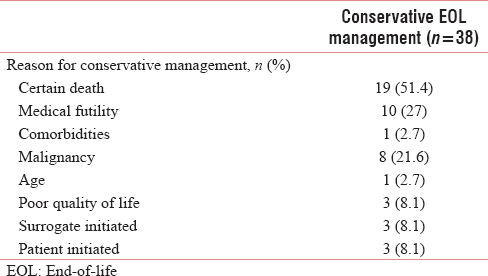
In 88.4% of cases (38/43 patients), the discussed EOL plan mirrored the actual plan. Among the study cohort, 38 patients (71.7%) were deemed for nonescalation of care or withdrawal due to imminent death (19 patients, 51.4%), medical futility with minimal response to maximal care (10 patients, 27%), and the presence of underlying malignancy (8 patients, 21.6%) [Table 3]. The decision for conservative therapy due to imminent death often occurs later during the patient's ICU stay as the disease progresses and the patient's status becomes more distinct. This is because critically ill patients are admitted in the early stages for resuscitation and may later deteriorate and be determined to likely perish despite maximal medical treatment.
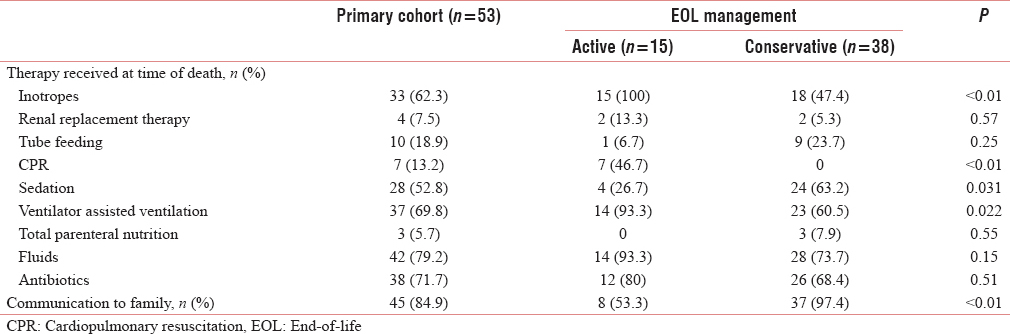
At the time of death, 50 patients (94.3%) were given intravenous fluids/TPN/tube feeding, 69.8% (37 patients) remained on ventilator support, 62.3% (33 patients) on inotropes, and 52.8% (28 patients) on sedatives [Table 4]. Patients who were placed on active EOL management were more likely to receive at the time of death inotropes, CPR, sedation, and ventilator-assisted ventilation although communication with the family was significantly poorer.
DISCUSSION
In this single-center, single ICU retrospective study, we found that 71.7% of patients dying in the SICU were confined to either treatment withdrawal (32.1%) or withhold (39.6%). There did not appear to be any significant difference in EOL management among different religions or races.
While patient autonomy is well established in Western society, its role in the Asian context is complicated. Singapore law[8] believes in the "individual autonomy" model whereby patients themselves have the right to know about their conditions and make their own decisions. However locally, families (especially of elderly patients) expect to be the first to know, and they will subsequently decide how much information to disclose to the patient.[910] While this generally stems from good intentions, in the case of EOL care, collective decision-making by the family may not always be in concordance to the patient's true wishes. It is startling to know that one-third of surrogates’ decisions run discordant to patients’ wishes[11] and up to 60% of physicians would overrule incompetent patients’ previously documented wishes.[12] The strong emphasis of filial piety based on the practice of Confucianism may also make it difficult for families to decide to withdraw or withhold therapy for the patient.
One way to mitigate this is the role of advance care planning (ACP) and the AMD. ACP is held in conjunction with the patient, caregivers, family members, medical team, to enable the patient to make informed decisions on his future health care, should he losses the ability to participate in these therapy decisions.[13] This has been shown to improve patients’ quality of life at the end, as well as patients and their families’ satisfaction as they have less stress, anxiety, and depression.[14] Detering et al.[14] in his prospective, randomized controlled trial also found that patients were not only interested in ACP, but they expected their medical team to initiate discussions. The AMD is a legally binding document that can be signed by any person aged 21 years and above with mental capacity. It acts to inform the medical team of the person's wish to avoid any life-sustaining therapy in situations where death is imminent. Unfortunately, population awareness and uptake of the AMD and ACP appears to be low,[151617] with only 37.9% expressing knowledge of the AMD, and 0.4% actually signing the form.[18] While the AMD ensures that patients receive the care they prefer during their EOL phase, studies have failed to show that AMDs improve medical or EOL care.[192021] However, ACP use is associated with significant cost savings of 25%![22]
It is hence important to engage patients early, particularly if they are elderly, have disseminated oncological disease or severe end-organ dysfunction with regards to ACP. In our study, most of the EOL discussions were held during patients’ ICU stay (median 1 (IQR 1–2)) and only 4.7% of patients were involved in their final EOL care decision-making. While this could be contributed by the fact that patient admitted to the ICU are critically ill, often sedated, and therefore unable to participate actively in their own care, this value is similar to another local study published in 2011 which shows that the general ward patient involvement in EOL care was at a dismal 6.2%.[17] Could this be due to the paternalistic approach in the Asian community? In contrast, Foo et al. found that in Singapore, 80% of the elderly would actually like to play an active role in their EOL decisions.[11] While there is no doubt the significance of patients’ wishes and/or their families’ and surrogates’ on EOL care, a large Asian study showed that only 43.9% of intensivists were comfortable holding a discussion on EOL care.[23] Perhaps, the limitation, therefore, lies in the varying practices of the intensivists. Hence, this emphasizes a greater need for clinicians to gain skills in such discussions so that these discussions can be conducted with their patients earlier while they still have adequate mental capacity.
Religion is believed to play a huge role in how patients view death. In a multiracial and religious society like ours, we have to take this in consideration during EOL discussions. For the Chinese, death is a taboo subject and any discussion about it is believed to be associated with bad luck.[24] In contrast, Muslims tend be more accepting of death and see death as predetermined and is a gateway to the afterlife.[25] In Taoism, death is also seen as a continuum of life and is often described as "a release from the body" and is accepted as a part of life.[26] Similarly, Buddhists believe in samsara which is a cycle of death and rebirth.[27] To them, life ceases to exist when the good karma accumulated from the previous life has been fully utilized. Besides religion of our patients, studies have also shown that the religion of the physicians may affect EOL decisions. The ETHICUS study found that Muslim physicians were more likely to withhold rather than to withdraw treatment.[34] Our study, however, failed to detect a significant difference between EOL management for both groups.
One-third of the patients in the conservative EOL care group were partially dependent or dependent on others for their daily function. This is congruent with the systematic review done by Frost which identified factors for a more conservative approach on EOL care to be more advance age, systemic illness, and limited functional status.[28] The decision for this could be because these patients are likely to have poor quality of life even after recovery from the critical illness, the potential for a prolonged hospitalization stay and rehabilitation period and the increased burden on the family to care for such patients.
Patients who received conservative EOL care tended to have better communication with the medical team and a longer length of stay. The median time from admission to first EOL discussion was 0 (IQR 0–1) versus 1 (IQR 0–3) days for the active versus conservative group. This could be attributed to the fact that the prognosis of these patients may not have been obvious from admission, and more time was required before an EOL discussion and decision was made. Therefore, this allowed the ICU team greater time to build rapport with the family before broaching the topic of conservative EOL care. Unfortunately, all patients who received a tracheostomy also belonged to the conservative group. This is likely due to the fact that patients for conservative EOL care tended to stay in the ICU for a longer period, hence, necessitating this invasive procedure. It is possible that an earlier EOL discussion with the inclusion of the use of invasive therapy may help to reduce an unnecessary procedure and also health-care costs.
Limitations
While this is the first known study on the practice of end-of-life care in patients dying in the ICU in Singapore, it is limited by its small sample size and the fact that this is a single center, single unit ICU study. This affects the ability of the study to be extrapolated to other patient populations such as medical, neurosurgical, and cardiothoracic critically ill patients. In addition, APACHE scores were not collected, so we are unable to determine how severely ill our patients are compared to other international studies. Further studies with larger sample size in multicentered centers will help to expand on our findings.
CONCLUSION
In summary, conservative EOL care decisions are made more than 2/3 of the time in the ICU with high congruence between the discussed decision and actual plan in place. In addition, there does not appear to be any significant differences in age, comorbidities or whom the surrogate-decision-maker is on patients’ EOL care. An improved ACP may help to guide patients on their preference for EOL care which may hence result in improved patient and family satisfaction.
Financial support and sponsorship
The study was funded by departmental resources.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The Economist Intelligence Unit. The 2015 Quality of Death Index - Ranking palliative care across the world 2nd edition. Available from: http://www.lienfoundation.org/sites/default/files/2015%20Quality%20of%20Death%20Report.pdf
- [Google Scholar]
- A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med. 1998;158:1163-7.
- [Google Scholar]
- End-of-life practices in European Intensive Care Units: The Ethicus Study. JAMA. 2003;290:790-7.
- [Google Scholar]
- Reasons, considerations, difficulties and documentation of end-of-life decisions in European Intensive Care Units: The ETHICUS study. Intensive Care Med. 2008;34:271-7.
- [Google Scholar]
- Attitudes towards ethical problems in critical care medicine: The Chinese perspective. Intensive Care Med. 2011;37:655-64.
- [Google Scholar]
- End-of-life decisions in ICU and cultural specificities. Intensive Care Med. 2005;31:506-7.
- [Google Scholar]
- Surgical "buy-in": The contractual relationship between surgeons and patients that influences decisions regarding life-supporting therapy. Crit Care Med. 2010;38:843-8.
- [Google Scholar]
- Understanding Health Law. Singapore Medical Association March. 2001. Available from: https://www.sma.org.sg/UploadedImg/files/CMEP/Health%207.pdf
- [Google Scholar]
- Sharing death and dying: Advance directives, autonomy and the family. Bioethics. 2004;18:87-103.
- [Google Scholar]
- Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist. 2005;45:634-41.
- [Google Scholar]
- Discrepancies in end-of-life decisions between elderly patients and their named surrogates. Ann Acad Med Singapore. 2012;41:141-53.
- [Google Scholar]
- Factors considered in end-of-life care decision making by health care professionals. Am J Hosp Palliat Care. 2013;30:354-8.
- [Google Scholar]
- The impact of advance care planning on end of life care in elderly patients: Randomised controlled trial. BMJ. 2010;340:c1345.
- [Google Scholar]
- An exploratory study of the knowledge, attitudes and perceptions of advance care planning in family caregivers of patients with advanced illness in Singapore. BMJ Support Palliat Care. 2013;3:343-8.
- [Google Scholar]
- Knowledge, attitudes and practices of the Advance medical directive in a residential estate in Singapore. Ann Acad Med Singapore. 2010;39:424-8.
- [Google Scholar]
- End-of-life care in the general wards of a Singaporean hospital: An Asian perspective. J Palliat Med. 2011;14:1296-301.
- [Google Scholar]
- News. Parliamentary Question and Answer. Advance Medical Directive. Available from: http://www.moh.gov.sg/mohcorp/parliamentaryqa.aspx?id=20348
- [Google Scholar]
- A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT principal investigators. JAMA. 1995;274:1591-8.
- [Google Scholar]
- Beyond advance directives: Importance of communication skills at the end of life. JAMA. 2005;294:359-65.
- [Google Scholar]
- Controlling death: The false promise of advance directives. Ann Intern Med. 2007;147:51-7.
- [Google Scholar]
- Potential influence of advance care planning and palliative care consultation on ICU costs for patients with chronic and serious illness. Crit Care Med. 2016;44:1474-81.
- [Google Scholar]
- Withholding and withdrawal of life-sustaining treatments in Intensive Care Units in Asia. JAMA Intern Med. 2015;175:363-71.
- [Google Scholar]
- 2011. Available from: http://www.scmp.com/article/985624/taboos-things-we-dont-talk-about
- Spiritual aspects of end-of-life care for Muslim patients: Experiences from Iran. Int J Palliat Nurs. 2005;11:468-74.
- [Google Scholar]
- The Afterlife. Available from: http://www.personaltao.com/teachings/taoism/the-afterlife/
- Teachings in Chinese Buddhism. Available from: http://www.buddhanet.net/cbp2_f7.htm
- Patient and healthcare professional factors influencing end-of-life decision-making during critical illness: A systematic review. Crit Care Med. 2011;39:1174-89.
- [Google Scholar]






