Translate this page into:
Anxiety and Depression: A Cross-sectional Survey among Parents of Children with Cancer
Address for correspondence: Dr. Vahid Pakpour, Department of Public Health Nursing, Faculty of Nursing and Midwifery, South Shariati Street, Tabriz, East Azerbaijan Province, Iran. E-mail: vahidpakpour@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Parents of children with cancer are experiencing high levels of psychological distress. Elevated levels of depression and anxiety following the disclosure of diagnosis affect many aspects of parents’ health.
Aims:
The aim of this study was to assess anxiety and depression of parents of Iranian children with cancer.
Settings and Design:
This descriptive-correlational study was undertaken among 148 parents of children with cancer admitted to a pediatric hospital affiliated to Tabriz University of Medical Sciences, Tabriz/Iran.
Subjects and Methods:
Participants were selected using convenience sampling method. Hospital Anxiety and Depression Scale was used to evaluate patients’ levels of anxiety and depression.
Statistical Analysis Used:
The data were analyzed using SPSS version 13.0.
Results:
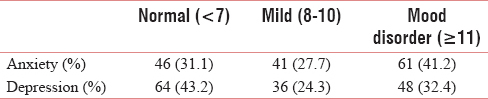
The study findings showed that the mean anxiety and depression scores were 9.63 ± 3.69 and 8.66 ± 4.59 (range score: 0–21), respectively. Additionally, 41.2% (n = 61) and 32.4% (n = 48) of participants had clinical symptoms of anxiety and depression, respectively.
Conclusions:
Parents of children with cancer experienced high levels of anxiety and depression. Effective interventions are essential to improve the mental health of parents of children with cancer. These interventions may include mental health screening, psychological counseling, and training programs to cope with the problems caused by the child's disease.
Keywords
Anxiety
childhood cancer
depression
parents
INTRODUCTION
Over the past few decades, substantial progress has been made in the diagnosis and treatment of childhood cancer. For some cancer types, the chance of 5-year survival rate is more than 90%.[1] Hence, due to increased survival rate of many childhood cancers, the caring role of parents is very important.[2]
Parents are one of the most important sources of emotional support for children with cancer and are in contact with health-care professionals in all phases of the disease.[3] Childhood cancer disrupts the family function[4] and is one of the most intense stressors that parents can have.[5] Parents also experience financial and psychosocial distress due to their children cancer.[6] Daily/role functioning, cancer communication, cancer caregiving,[7] recurrence of the disease,[8] and life-threatening cancer[9] are factors that aggravate the parents’ distress. Childhood cancer may also affect parents’ relationship, which is another reason for elevated anxiety and depression among parents.[2]
The findings of a systematic review by Pitceathly and Maguire showed that family members may experience higher levels of distress than cancer patients.[10] Parents of children with cancer experience high anxiety.[11] Earlier findings showed that the anxiety was often even higher in parents of children with cancer than in children and adult cancer patients themselves.[12] Howard Sharp et al. reported that the prevalence of anxiety and depression among parents of children with cancer was higher than parents of healthy children.[13] Hence, cancer seems to be a family disease rather than a disease that only affect individuals.[6]
It has been acknowledged that it is important to know the psychological needs of parents as well as sick child.[714] According to the findings of earlier studies, parents who suffer emotional problems had serious difficulty in adjustment to childhood cancer.[15] Strain and its manifestations such as anxiety and depressive symptoms had adverse effects on parents’ health. Hence, parents less likely could use effective adjustment strategies to deal with family's normal activities and may experience inadequacy in providing the disease-related needs of children.[16]
To date, studies examining emotional distress of parents of children with cancer were predominantly conducted in developed countries. Such studies are useful for developing supportive and rehabilitation programs for parents of children with cancer. Hence, the present study aimed to examine the level of anxiety and depression among parents of children with cancer.
SUBJECTS AND METHODS
This descriptive-correlational design study was conducted in a pediatric cancer center affiliated to Tabriz University of Medical Sciences, Tabriz, Iran. The study population included all the parents (mothers or fathers) whose child was admitted to the center with cancer diagnosis in 2014 and met the following criteria: (a) Having confirmed cancer diagnosis in child; (b) parents be at least 18 years old; (c) child be at most 16 years old; (d) willing to participate in the study; and (e) at least 3 months passed since they were aware of diagnosis. The sample size (n = 138) was calculated based on a pilot study of twenty parents of children with cancer. Considering sample attrition of 10%, a convenience sample of 155 parents was invited to participate in the study. Overall, 148 parents of children with cancer accepted to be enrolled (response rate = 95%).
Before the data collection, the study proposal was approved by Hematology-Oncology Research Center and Regional Ethics Committee of Tabriz University of Medical Sciences. Next, researchers were referring to the hospitalization ward and outpatient clinic of pediatric cancer center. Parents who met criteria for the study were identified and all eligible samples were invited to participate. After being presented the basic information, willing parents were asked to fill the questionnaire or participate in a private interview for data collection. All samples who participated in the study gave informed consent.
The instrument for data collection composed of two parts. The first part was to collect the demographic characteristics of parents and their children including age, gender, education, and job. The second included Hospital Anxiety and Depression Scale (HADS) developed by Zigmond and Snaith in 1983.[17] This questionnaire consisting of 14 items on a 4-point Likert scale (range 0–3) is divided into two subscales. The first subscale is a 7-item anxiety subscale used to assess anxious mood, and the second subscale is a 7-item depression subscale used to assess depressive mood. Each item is classified according to a 4-point Likert scale ranging from 0 (strongly disagree) to 3 (strongly agree). The total score in each subscale is 0–21 points with scores categorized as follows: normal 0–7, mild 8–10, and ≥11 indicate anxiety and depression. This questionnaire was used in many studies in different contexts[1819] and its validity and reliability was confirmed in Iran.[20]
For using the scale, HADS was translated into Persian and then, its accuracy and fluency were confirmed by a translator expert in both Persian and English. The scale's face and content validity were assessed and verified by the expert panel that constituted 15 members. Some minor changes were applied according to expert recommendations. The final version of the questionnaires was tested for reliability in a pilot study involving twenty parents of children with cancer. Cronbach's alpha coefficient values for anxiety and depression subscale were 0.76 and 0.80, respectively.
Data were analyzed using the SPSS statistical software package(SPSS Statistics version 16, SPSS, Chicago, IL, USA). Some demographic and disease-related characteristics of parents and their children were described using descriptive statistics such as the frequency, percentage, mean, and standard deviation (SD). Nonparametric inferential statistics (Mann–Whitney and Kruskal–Wallis) were used to evaluate associations between study variables. P < 0.05 was considered statistically significant.
RESULTS
The mean age of participating parents was 36.08 ± 2.08 years (range: 21–49 years). Most of them (79.1) were female. The average number of children per family was 2.08 ± 1.05 (range: 1–5). The mean of time passed since awareness of cancer diagnosis was 13.62 ± 12.73 months (range: 3–72 months). The mean of children age was 10.18 ± 2.56 (range: 6–15 years). Most of the children (64.2%) were undergoing chemotherapy. The mothers were often the caregiver of children (81.1%). Other demographic and disease-related characteristics of parents and their children are shown in Tables 1 and 2.


Mean scores of anxiety and depression of parents were 9.63 (SD: 3.69) and 8.66 (SD: 4.59), respectively. Nearly 41.2% (n = 61) and 32.4% (n = 48) of participants had clinical symptoms of anxiety and depression (score ≥11), respectively. Table 3 shows the participants’ psychological status based on HADS classification.
Since most of the data were not normally distributed, nonparametric inferential statistics (Mann–Whitney and Kruskal–Wallis) were used. The finding showed no significant difference between the mean of mothers’ and fathers’ anxiety and depression scores. There was also no significant difference between anxiety score and parents’ education and job, type of medical treatment, type of caregiver, and child education. However, there was a significant difference between the mean of depression scores with father's job (P = 0.041) and type of caregiver (P = 0.026). No effects of parents’ education, mothers’ job, type of medical treatment, and child education on reported levels of depression were found.
DISCUSSION
Parents are recognized as one of the main sources of emotional support for children with cancer.[14] However, the caring ability of parents whose child has/had cancer depends on how they manage to cope with the diagnosis and its consequences.[3] The finding of this cross-sectional study indicates high levels of anxiety among parents of children with cancer. In our study, 42% of mothers and 35% of fathers had anxiety disorder. Fotiadou et al. found that 68% of mothers and 37% of fathers of children with cancer were at risk for clinical symptoms of anxiety.[21] They attribute these differences to traditional caregiving roles of mothers. As well, women tend to report pain and discomforts more than men. In a study conducted in the USA, Rodriguez et al. reported higher levels of distress among parents of children with cancer.[7] Norberg and Boman reported severe distress among parents of children with cancer in the first year after diagnosis. However, they found that high levels of parents’ anxiety and depression were still eminent up to 2.5 years after diagnosis, which indicates the importance of uninterrupted parents’ support.[22]
In our study, about 70% of parents had mild and high level of anxiety. The findings of previous studies also showed that parents of children with cancer had high levels of psychological distress.[722] The findings of Kazak et al's. study showed that almost parents of all children with cancer reported posttraumatic stress symptoms during medical treatments.[23] In a study by Basher et al. in Bangladesh, 49% of parents of children with cancer had anxiety and up to 22% of parents for whom 7–12 months had passed since diagnosis reported severe psychological distress.[14] However, the levels of child distress also had a direct impact on severity of parents’ psychological disorders.[24]
In other countries, it has been estimated that one of the general populations had anxiety disorder.[25] Although there is no evidence regarding the prevalence of anxiety in the general population in Iran, the findings of this study showed high levels of anxiety among parents of children with cancer. This indicates the importance of continual attention to the psychosocial needs of parents following a child's cancer diagnosis.
As mentioned before, there was no significant difference between mother's and father's levels of anxiety which is consistent with the findings of earlier studies.[2126] In fact, nowadays, parenting tasks are shifting toward both parents and they are equally participating in the child care duties. Hence, the experience of child cancer is as traumatic for fathers as for mothers and it is important to pay attention to father's psychological needs. The findings of Valizadeh et al. showed that caring responsibility of fathers was prominent in emotional dimension and mothers burden more demands of physical care.[27]
As another finding of the study, 31% of mothers and 35% of fathers had symptoms of depression. Congruent to our findings, Wrosch et al. found that a depressive symptom of parents of children with cancer was surpassed those of parents of healthy children.[28] Norberg and Boman also reported high levels of depression among parents of children with cancer.[22]
In our study, there was a significant difference between the mean of depression score and father's job. In Wrosch et al's. study, educated fathers reported lower levels of depression than illiterate counterparts.[28] The study finding highlights the importance of continuous emotional support that should be paid to parents of children with cancer. Nurses’ support could help the parents to effectively cope with the diagnosis and carry out their responsibilities for the care of the child.
Limitations
Despite the strength of this study, it also has some limitations. First, we only examined the anxiety and depression of parents and other aspects of their distress were not assessed. Parents’ psychological responses might have been influenced by quality of care received by this cancer center which limits the generalization of our findings to other medical centers. In addition, as we had no access to the children's medical records, most of the required data such as medical treatments and time elapsed since diagnosis were collected based on parent's report. Hence, recall bias is possible. In addition, most of our participants were mothers which may have different emotional responses than fathers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Improved survival for children and adolescents with acute lymphoblastic leukemia between 1990 and 2005: A report from the children's oncology group. J Clin Oncol. 2012;30:1663-9.
- [Google Scholar]
- Providing care to a child with cancer: A longitudinal study on the course, predictors, and impact of caregiving stress during the first year after diagnosis. Psychooncology. 2015;24:318-24.
- [Google Scholar]
- The care of my child with cancer: Parents’ perceptions of caregiving demands. J Pediatr Oncol Nurs. 2002;19:218-28.
- [Google Scholar]
- Association of health-related quality of life with resilience among mothers of children with cancer: A cross-sectional study. Iran J Pediatr Hematol Oncol. 2016;6:84-91.
- [Google Scholar]
- Early avoidance of disease- and treatment-related distress predicts post-traumatic stress in parents of children with cancer. Eur J Oncol Nurs. 2011;15:80-4.
- [Google Scholar]
- Relationships between parenting self-efficacy and distress in parents who have school-aged children and have been treated with hematopoietic stem cell transplant or have no cancer history. Psychooncology. 2016;25:339-46.
- [Google Scholar]
- Cancer-related sources of stress for children with cancer and their parents. J Pediatr Psychol. 2012;37:185-97.
- [Google Scholar]
- Symptoms of posttraumatic stress in parents of children with cancer: Are they elevated relative to parents of healthy children? J Pediatr Psychol. 2009;34:4-13.
- [Google Scholar]
- Cancer-related parental beliefs: The family illness beliefs inventory (FIBI) J Pediatr Psychol. 2004;29:531-42.
- [Google Scholar]
- The psychological impact of cancer on patients’ partners and other key relatives: A review. Eur J Cancer. 2003;39:1517-24.
- [Google Scholar]
- Parents of children with cancer: At-risk or resilient? J Pediatr Psychol. 2015;40:914-25.
- [Google Scholar]
- Predictors of psychological functioning in children with cancer: Disposition and cumulative life stressors. Psychooncology. 2015;24:779-86.
- [Google Scholar]
- Rethinking Experiences Of Childhood Cancer: A Multidisciplinary Approach To Chronic Childhood Illness: A Multidisciplinary Approach to Chronic Childhood Illness. UK. Glasgow: Bell & Bain Ltd, McGraw-Hill Education (UK); 2005.
- [Google Scholar]
- A Rasch analysis of the Hospital Anxiety and Depression Scale (HADS) among cancer survivors. Psychol Assess. 2013;25:379-90.
- [Google Scholar]
- The Hospital Anxiety And Depression Scale: A meta confirmatory factor analysis. J Psychosom Res. 2013;74:74-81.
- [Google Scholar]
- The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:14.
- [Google Scholar]
- Optimism and psychological well-being among parents of children with cancer: An exploratory study. Psychooncology. 2008;17:401-9.
- [Google Scholar]
- Parent distress in childhood cancer: A comparative evaluation of posttraumatic stress symptoms, depression and anxiety. Acta Oncol. 2008;47:267-74.
- [Google Scholar]
- Posttraumatic stress symptoms during treatment in parents of children with cancer. J Clin Oncol. 2005;23:7405-10.
- [Google Scholar]
- Association between parent and child distress and the moderating effects of life events in families with and without a history of pediatric cancer. J Pediatr Psychol. 2014;39:1049-60.
- [Google Scholar]
- Depression and anxiety in the United States: Findings from the 2006 behavioral risk factor surveillance system. Psychiatr Serv. 2008;59:1383-90.
- [Google Scholar]
- Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J Pediatr Psychol. 2004;29:211-9.
- [Google Scholar]
- Determinants of care giving burden in parents of child with cancer at Tabriz children medical and training center. J Clin Nurs Midwifery. 2014;3:13-20.
- [Google Scholar]
- Adaptive self-regulation of unattainable goals: Goal disengagement, goal reengagement, and subjective well-being. Pers Soc Psychol Bull. 2003;29:1494-508.
- [Google Scholar]






