Translate this page into:
Clinical Impact of Education Provision on Determining Advance Care Planning Decisions among End Stage Renal Disease Patients Receiving Regular Hemodialysis in University Malaya Medical Centre
Address for correspondence: Dr. Albert Hing (Wong); E-mail: alberthing@hotmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Advance care planning (ACP) is a process of shared decision-making about future health-care plans between patients, health care providers, and family members, should patients becomes incapable of participating in medical treatment decisions. ACP discussions enhance patient's autonomy, focus on patient's values and treatment preferences, and promote patient-centered care. ACP is integrated as part of clinical practice in Singapore and the United States.
Aim:
To assess the clinical impact of education provision on determining ACP decisions among end-stage renal disease patients on regular hemodialysis at University Malaya Medical Centre (UMMC). To study the knowledge and attitude of patients toward ACP and end-of-life issues.
Materials and Methods:
Fifty-six patients were recruited from UMMC. About 43 questions pretest survey adapted from Lyon's ACP survey and Moss's cardiopulmonary resuscitation (CPR) attitude survey was given to patients to answer. An educational brochure is then introduced to these patients, and a posttest survey carried out after that. The results were analyzed using SPSS version 22.0.
Results:
Opinion on ACP, including CPR decisions, showed an upward trend on the importance percentage after the educational brochure exposure, but this was statistically not significant. Seventy-five percent of participants had never heard of ACP before, and only 3.6% had actually prepared a written advanced directive.
Conclusion:
The ACP educational brochure clinically impacts patients’ preferences and decisions toward end-of-life care; however, this is statistically not significant. Majority of patients have poor knowledge on ACP. This study lays the foundation for execution of future larger scale clinical trials, and ultimately, the incorporation of ACP into clinical practice in Malaysia.
Keywords
Advance care planning
Cardiopulmonary resuscitation
End-stage renal disease
Hemodialysis
Palliative care
INTRODUCTION
Patients with end-stage renal disease (ESRD) have significantly increased morbidity and mortality. ESRD is a chronic degenerative disease that takes many years to end a patient's life.[1] The National Kidney Foundation of the United States through its Kidney Disease Outcomes Quality Initiative program defines chronic kidney disease (CKD) in adults as evidence of structural or functional kidney abnormalities (abnormal urinalysis, imaging studies, or histology) that persist for at least 3 months, with or without a decrease in glomerular filtration rate (GFR), or decreased GFR, with or without evidence of kidney damage.[2] National Health and Nutrition Examination Survey classifies GFR of <15 mL/min/1.73 m2 as CKD Stage 5 or ESRD.[3]
The main objective of this clinical research is to assess the clinical impact of education on determining advance care planning (ACP) decisions among ESRD patients on regular hemodialysis (HD) at University Malaya Medical Centre (UMMC). The secondary objective is to study the knowledge and attitude of this group of patients toward ACP and end-of-life issues
Literature review
Despite continuing technological advancements, mortality rate remains high among dialysis patients, with 15–25% of deaths resulting from a decision to discontinue dialysis; the second leading cause of death after cardiovascular disease.[4] Comprehensive care of ESRD patients requires not only medical and technical aspects of maintaining patients on dialysis but also in ACP.[5] ACP is important to prepare patients on dialysis and their loved ones for the end-of-life. It is a process of communication among the patients, their families, and professional caregiver, which include, but is not limited to discussing preferences for life-sustaining treatments.[6] Elements of ACP include clarifying patients’ understanding of their illness and treatment options; understanding their values, beliefs, and goals of care; and identifying their wishes.[7]
The majority of ESRD patients in Malaysia succumbed due to cardiovascular diseases. This accounted for 35% of deaths among ESRD patients according to the Malaysian Dialysis and Transplant Registry 2013. About 19% of mortality was due to death at home, and these were believed due to cardiovascular events as well. An interesting fact is that only 1% or 40 patients in 2013 succumbed due to withdrawal of dialysis.[8] Withdrawal of dialysis resulting in death only accounted for 1% of deaths since 2004. This could be because the option of dialysis withdrawal was not made available to patients throughout the duration of illness, and very few nephrologists actually do discuss with their patients about ACP and advanced directives.
Since the 1990s, there has been increasing awareness of the inadequacy of end- of-life care and of the poor knowledge of patients’ wishes about their medical treatment when they lose the capacity to make decisions, causing patients to be treated in a way they would not have chosen.[9] Previous studies suggest that ACP may improve the quality of end-of-life care for patients and families.[7] Despite that, ACP is currently not included in routine clinical care for patients on dialysis.[10] Only 6–35% of dialysis patients have advance directives, which are legal documents with powers and requirements that vary widely from jurisdiction to jurisdiction, and they tend to outline limited treatment options.[4] Even with introduction of educational initiatives aiming to increase awareness of ACP, many still do not complete advance directives.[11]
Although the concept of ACP has been around for many years, it is neither well known nor well utilized in routine clinical practice in Malaysia. ACP services are not available officially but brochures can be obtained through Palliative Care Malaysia website hosted by Hospis Malaysia. To this point, there was no study in Malaysia to look into the percentage of patients admitted terminally ill with advanced directives. A study done in 2007 on 15 elderly Malaysians revealed a lack of knowledge on ACP. Although the majority agreed on the importance of planning for future medical management and having open discussion on end-of-life issues with their doctor, they felt it is unnecessary to make formal written advanced directives.[12]
Sadly for ESRD patients in Malaysia, there are no standards of practice regarding when to initiate or how to facilitate ACP. Patients undergoing dialysis typically do not view themselves as terminally ill and falsely assume they can be kept alive indefinitely on dialysis. Issues relating to death and dying are commonly avoided until late in the illness.[13] A coordinated, systematic model of patient-centered ACP using nonmedical ACP facilitators assists in identifying and respecting patient's wishes about end-of-life care, improves ACP care from the perspective of the patient and the family, and diminishes the likelihood of stress, anxiety, and depression in surviving relatives.[7]
With only one previous study on ACP in Malaysia, we decided to embark on a study to determine whether lack of knowledge impacts on the decision on ACP, and at the same time explore the knowledge and attitude of ESRD patients on ACP. This will help pave information for this specific group of patients, enabling future easier execution of larger scale clinical trials, and ultimately, the incorporation of ACP into routine clinical practice in Malaysia.
MATERIALS AND METHODS
This study was carried out with the approval of University of Malaya Medical Centre Medical Ethics Committee in accordance with the Helsinki Declaration under MECID number 20147–414. The study was also registered under National Medical Research Registry bearing an ID of NMRR-14-960-22404. Written informed consent was obtained from participating patients after they have read the Patient Information Sheet.
Subjects and sample size
Convenience sampling was used and all patients aged 21-year-old and above who were undergoing long-term HD in UMMC and University Malaya Specialist Centre (UMSC) were recruited. Patients’ recruitment was on a voluntary basis. Patients were excluded from the study if they had any of the following: (a) Mentally challenged, (b) deaf or blind, (c) had an acute illness and admitted to the hospital, (d) refused to participate, (e) not on regular dialysis yet.
Study methods
This is a cross-sectional study. The data collection period was from August 2014 till November 2014. A search was conducted to find the most suitable survey form for the ACP study. There were many different versions of ACP surveys online, but none were specifically designed for ESRD patients. The decision was made during an expert panel meeting involving nephrologist, palliative physician, and statistician to utilize Lyon's ACP Survey Form Patient Version in combination with Moss cardiopulmonary resuscitation (CPR) Attitude Survey Form. Written permission was obtained from the authors to utilize these forms with some modifications. Educational brochures were sourced online, but many were in point forms with lengthy explanations, which may not be effective in bringing across the ACP message. Thus, two real life ACP experience stories from the Canadian Hospice Palliative Care Association (CHPCA) online website were used as educational brochure.
The modified survey form and educational brochure were then forward translated to Malay language by a Malay doctor, who is fluent in both English and Malay language. Back-translation to English language was done by a teacher, who is fluent in both English and Malay language. The back-translated version was then compared with the original version, and the differences were examined. We pilot tested the survey form on three independent individuals, whom are staff registered nurses. The survey form was face validated by three independent undergraduate students and content validated by a nephrologist and a palliative physician.
Patients were recruited during their regular HD sessions at UMMC or UMSC. Patients were provided with the pretest survey form and were encouraged to answer on the spot, as each dialysis session is 4 h. However, they were also allowed to complete the survey form at home. Once a patient had completed the pretest survey, the form was collected and the educational brochure was then introduced. Timeframe of 2 days was given for patient to read the educational brochure, and the posttest survey was conducted at the following dialysis session. Again patients were encouraged to complete the posttest survey on the spot.
This study is subjected to intervention bias as only the Malay language version survey form was utilized, and few of the patients who do not understand Malay are interviewed personally by the investigator. There is also selection bias involved as the sample was all from UMMC and UMSC HD unit.
Demographic data such as age, gender, race, religion, occupation, education level, underlying medical illnesses, cause of renal failure, and duration on HD were included. These data were obtained during the pretest survey.
Biostatistical analysis
All analysis was performed using SPSS version 22.0 (International Business Machines Corp). For demographic characteristics of patients, the categorical variables were presented in frequency with percentages, whereas the numerical variables were presented in mean with standard deviation. For most parts of the survey, descriptive analysis was used, and results were described in terms of percentages and mean. Pearson's Chi-square test and Fisher's exact test were used to determine association between knowledge and attitude of patients on ACP. As the collected data for the pretest and posttest survey were predominantly paired nominal data, McNemar-Bowker test was utilized. A P < 0.05 is considered statistically significant.
RESULT AND DATA ANALYSIS
There were a total of 80 patients on HD at UMMC and UMSC during the study period. About 22 patients were excluded due to various reasons. These include those who are mentally challenged (3), those who refused to participate (7), blind/deaf/mute (6), those who were admitted to the ward with an acute illness,[3] and those who were not yet on regular dialysis (3). A total of 58 patients were recruited during the study period from August 2014 to November 2014, with 2 dropouts during the study. Social demographic data of patients were shown in Table 1. The mean age of participants was 59.5 ± 10.9, with the youngest participant at the age of 30 and the oldest at the age of 83. Majority (69.6%) of participants fell between the age group of 46–60 years old. The distribution of gender is fairly equal, with 32 (57.1%) male participants and 24 (42.9%) female participants. There were 39 (69.6%) Malays, 10 (17.9%) Chinese, and 7 (12.5%) Indians. Muslims consisted of 69.6% (n = 39) of the study population, whereas Hindus and Christians took up 10.7% (n = 6). Buddhists consist of 5.4% (n = 3) and others were 3.6% (n = 2). Half of the participants (51.7%) are retired, and among the 29 retirees, 25 are pensioners. Around 12 participants are working, and their occupation consists of accounting (1), business (2), lecturer (2), engineer (1), nurse (1), police (1), executive (1), teacher (1), driver (1), and contractor (1).
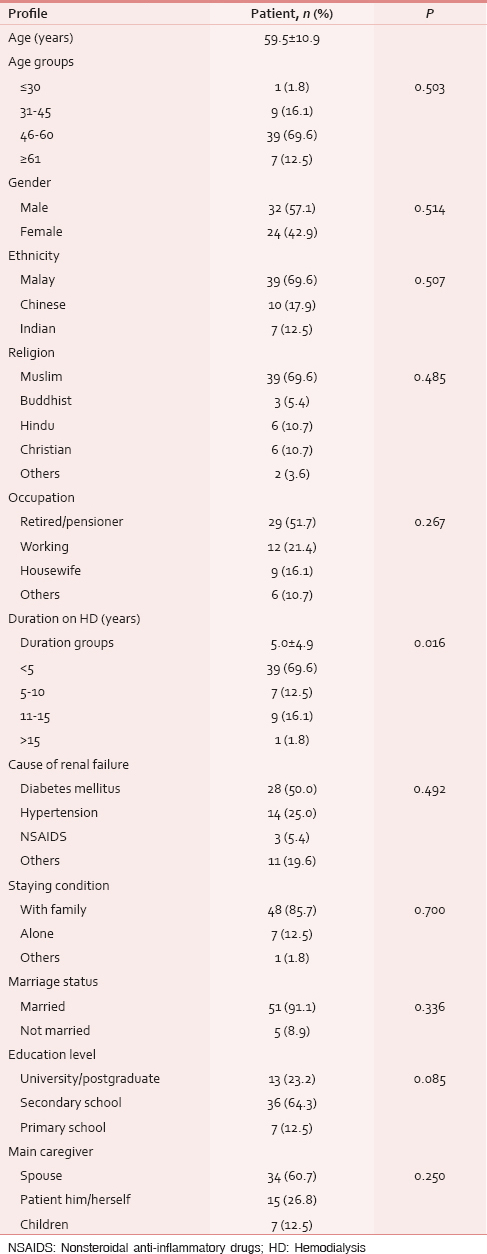
With regards to the duration of HD, majority has undergone HD for <5 years (69.6% or n = 39), with mean years on HD of 5.0 ± 4.9. The longest surviving participant on HD has a record of 21 years on dialysis. Figure 1 demonstrates the distribution of participants’ HD duration by groups. Half (n = 28) of the patients suffered from diabetes mellitus which was the main cause of renal failure. A quarter of the participants had ESRD due to hypertension (n = 14), and nonsteroidal anti-inflammatory drugs usage contribute to 5.4% (n = 3) of the study population. Figure 2 is a pie chart demonstrating the cause of renal failure among participants.

- Distribution of participants by hemodialysis duration groups

- Causes of renal failure among participants
Out of 56 participants, 48 (85.7%) stays with their immediate family, whereas 7 (12.5%) stays alone. Almost all participants (n = 51 or 91.1%) were married. About 7 (12.5%) participants only studied till primary school, while 36 (64.3%) studied till secondary school. About 13 (23.2%) participants are university/postgraduate level education. Most participants quoted spouse as their main caretaker (60.7%). About 15 (26.8%) participants take care of themselves, and the remaining 7 (12.5%) were taken care of by their child/children.
The primary objective of this study is to look at the clinical impact of education on ACP decisions among participants. Questions pertaining to CPR and intubation were introduced preeducation as well as posteducation. Only 3.6% (n = 2) of participants had heard of ACP and had actually prepared written advanced directives. Around 75% (n = 42) of participants had never heard of ACP before. However, most of the participants (69.6%) had verbally discussed end-of-life care with their spouse at some point of time. Higher educational level among participants did not seem to affect the frequency of end-of-life discussions (P = 0.658), nor does it affect the plans for future health (P = 0.840).
When asked on the importance of early preparation of ACP, 36 (64.3%) of participants gave a positive response while the rest thought it was not important. There was no statistically significant difference in participants’ opinion after exposure to the educational brochure (P = 0.152). On whether a participant will start making plans for ACP after the survey, similar results were obtained. Around 67.9% (n = 38) of patients expressed plans to prepare ACP while the rest had no plans. After educational brochure exposure, there was no statistically significant difference in terms of plans for ACP (P = 0.146). The decision for CPR or intubation in the event of cardiorespiratory collapse outside of dialysis center did not show any statistical significance pre- and post-educational brochure (P = 0.146). Hence, it is the decision for resuscitation in the event of cardiorespiratory collapse during dialysis (P = 0.754). However, although statistically not significant, generally there was an upward trend in the percentage of importance posteducational brochure, especially for importance and plans for ACP and CPR decision outside of dialysis. This is shown in Table 2.

Questions on cardiorespiratory collapse revealed some interesting results. The majority (n = 42) of participants knew what is CPR, and 48.2% (n = 27) had seen CPR been done on a real patient before. Only 69.6% (n = 39) of participants wanted CPR in the event of cardiorespiratory collapse outside of dialysis center, but more (82.1%), n = 46, wanted resuscitation in the event of cardiorespiratory collapse during HD. This difference is statistically significant (P = 0.001). However, when given the chances of survival in the event of cardiorespiratory collapse was <10%, almost half of the participants, n = 27 (48.2%) chose not for CPR. This is statistically significant at P ≤ 0.001.
Almost half of the participants think the best time to discuss end-of-life issues is when they are well and healthy (48.2%, n = 27), and 91.1% (n = 51) wants their family members to be involved in end-of-life decision-making. Doctors (n = 51) are preferred to nurses (n = 2) and psychologists (n = 1) in terms of discussing with patients about end-of-life issues. Participants generally trust the treating doctor and hospital to respect and execute their end-of-life wishes (76.8%). About 82.1% (n = 46) of participants believe their families would understand their end-of-life wishes and 87.5% (n = 49) believe their families will respect and execute their wishes.
When it comes to thoughts about death and dying, 41.1% of participants felt comfortable discussing death. However, in reality, half of the participants rarely or never discuss end-of-life issues with their families (48.2%). Out of 56 participants, 49 participants agreed that dying is an important process in life, but when given an option to know beforehand the exact dying date, 25 (44.6%) stated they do not want to know the date. Financial issues (53.6% not concerned) and burden to family (42.9% not concerned) does not seem to be an important consideration in the context of end-of-life thoughts.
Most participants, n = 38 (67.9%) chose to pass away at home, and another 11 (19.6%) chose to pass away in hospital. With regards to terminal pain, 73.2% of participants will only take pain medicines when the pain is severe. Most (69.6%) would prefer to take painkillers at the lowest amount possible and save higher doses for worse pain in the future. Around 58.9% of respondents were worried with analgesic overdose. Participants tend to have a mixed opinion on issues of analgesics addiction and also whether the treating doctor will believe and treat their pain accordingly.
Nearly 64.3% (n = 36) of participants deemed themselves to be religious, and they frequently rely on religion to help them face their fears. Three-quarter of participants (n = 41) frequently attends religious or spiritual services. The level of religiousness does not seem to affect the frequency of end-of-life discussions among participants (P = 0.664). About 76.8% (n = 43) of participants are likely to attend funerals or memorial services of a loved one, friend, or classmate. Only 12.5% (n = 7) are likely to avoid medical checkups due to fear of doctor finding “something serious.” Around 64.3% (n = 36) are likely to speak freely to loved ones about death and dying, and 87.5% (n = 49) do not mind visiting a friend or relative who has recently lost a loved one. However, only 13 (23.2%) of participants are likely to preplan their own funeral.
When dealing with own dying, majority thinks it is important to have friends or family visiting them. Honest answers from the treating doctor, comfort from religious services or persons, fulfilling personal goals or pleasures, and understanding of end-of-life treatment choices were also deemed important by participants. Table 3 shows the important aspects when dealing with dying and the distribution of choices by percentage. Being able to stay at home when near dying, planning of own funeral, preparing advance directives, review own life story with family, and having a doctor visiting participant at home seems to be of less importance comparatively.

On thoughts about dying; being physically comfortable, at peace spiritually, having a sense of own worth and value, and saying everything needed to family members are the priorities of participants. Furthermore, important but to a lesser extent were being pain-free, not burdening loved ones, and dying a natural death. Being off ventilators as well as knowing how to say goodbye are of less importance comparatively. Table 4 relates the issues on thoughts about dying and the distribution of choices by percentage.

DISCUSSION
The level of familiarity and dissemination of ACP remains limited in the general population despite efforts of implementation.[14] A study on 15 elderly Malaysian patients in 2007 revealed a lack of knowledge on ACP.[12] Up to date, there was no study in Malaysia that looks into aspects of end of life and ACP among ESRD patients on regular HD.
Three-quarter of the study participants have never heard of ACP before, which is not surprising. Although about 64.3% thought that ACP is important, only 3.6% actually prepared written advanced directives. This finding is similar to a study done in 2011 in Spain, where only 5.3% of patients had advanced directives.[14] Approximately, 70% of participants have discussed end-of-life issues with spouse at some point of time, but there was no official decision or written directives on the exact plan of action in the event of cardiorespiratory collapse.
ACP educational brochure clinically impacts participants’ opinion on the importance of ACP and alters the plans for ACP preparation. This is shown by the increasing percentage of importance chosen by participants posteducational brochure. The percentage of patients who chose for CPR and intubation in the event of cardiorespiratory collapse outside of dialysis also increased posteducational brochure. However, these results were found to be statistically not significant, likely because of the small study sample size. The educational brochure was conveyed in the form of real-life stories and elements of ACP were not directed injected into participants’ minds. We chose to use real-life stories from CHPCA website as ACP itself is a very broad topic and reading the entire ACP brochure could be very taxing for participants. Using stories would get messages across to readers more easily than just showing brochures. Concept of ACP is new and some participants may find it difficult to comprehend, thus resulting in no statistically difference in the choice of resuscitation and ACP plans pre- and post-education.
Most of the participants studied till secondary school. Educational level does not seem to affect the frequency of end-of-life discussions nor does it affect the plans for ACP. This result is in line with a study in Spain which showed that level of education does not affect end-of-life decisions.[14] Another study in Saudi Arabia showed that in higher education group, relatively more participants (48.5%) become uncertain of their end-of-life decisions, which includes decision for CPR.[15] ACP decisions and planning were not affected by how religious a person is, and this is also reflected in the Saudi Arabia study.[15]
Significantly more participants wanted CPR in the event of collapse during dialysis when compared to collapse, not during dialysis. A study in Canada revealed that 86% of regular dialysis patients wanted to continue dialysis at their current health state.[16] Dialysis is a remarkable, life-prolonging therapy, as well as by definition a death-delaying treatment.[17] This concept is probably the reason that affected more participants to choose CPR in the event of collapse during dialysis.
Generally, participants chose for CPR in the event of cardiorespiratory collapse, but when provided with only 10% survival chance, about 48.2% of participants chose not for CPR. This result is similar to a study done on dialysis patients’ attitudes about CPR, where approximately 50% of patients undergoing chronic dialysis voted against CPR if this were to result in coma, persistent vegetative state, severe dementia, or terminal illness.[18] Sufficient to say, patients often poorly understand medical care,[19] including CPR and may overestimate their probabilities of survival.[202122]
Half of the participants prefer to discuss end-of-life issues when they are physically well and healthy. Most (91.1%) prefer to involve closest family members for end-of-life discussions. This percentage is significantly higher than a Spanish study where 60% of patients had empowered a family member to represent them for end-of-life decisions.[14] Doctors are preferred person to initiate ACP discussions. Patients welcome ACP and expect health professionals to initiate discussions.[1923]
When participants are dealing with dying, almost all wanted an honest answer from the treating doctor. Many a times, family members worry with the impact of diagnosis on patients. It is not uncommon for family members to thwart a doctor's attempt at disclosure of terminal illness diagnosis to the patient.[24] This study actually shows that majority of patients wish to know more about their problem and diagnosis, as well as available treatment options that they can choose from. Comfort from religious services is still an important element in dealing with dying although the level of religiousness does not affect the decision on end-of-life care. Besides, the above, having family and friends visiting is also an important element in dealing with dying.
Dying with dignity seems to be the most important consideration when participants were thinking about death. This includes dying with a sense of own worth or value, being at peace spiritually, saying everything wanted to family members and also being physically comfortable. A study on CKD stage 4–5 patients in Northern Alberta Renal Program evaluated end-of-life care preferences, and most patients preferred care focused on decreasing pain and suffering.[25]
There are confounding factors in this study that impacts on ACP decisions, the most significant being the duration of HD for patients. The P value was found to be significant at P = 0.016. This means patients are more likely to engage in ACP planning and discussions if they are recently started on dialysis. The rest of the factors such age, gender, ethnicity, occupation, causes of renal failure, staying condition, and marriage status did not show any statistically significant association.
An interesting point which was not covered in this study is the option for dialysis withdrawal, which was discussed extensively during literature search. Each year, more than 10,000 deaths in the United States are preceded by decisions to withdraw from dialysis. The American Society of Nephrology and Renal Physicians Association, after a laborious process that included a comprehensive literature search, evidence critique, and peer review, published practice guidelines for withholding and withdrawing dialysis.[262728] A study on preferences for dialysis withdrawal in the United States showed that dialysis preferences vary widely with age and ethnicity.[29]
Issues of dialysis withdrawal need to be discussed very carefully before carried out. Considerations for dialysis withdrawal will be those who may benefit from withdrawal, for example, poor prognosis, poor quality of life, intractable pain, and progressive malignancy, when dialysis is technically difficult or impossible. Discussion needs to be done on goals of care, quality of life on dialysis, possible symptoms, and their palliation. Most importantly is the option of dialysis withdrawal, and the decision is completely reversible anytime.[17]
CONCLUSION
The educational brochure on ACP clinically impacts on patients’ preferences and decisions toward end-of-life care; however, this is statistically not significant. Majority of patients have poor knowledge on ACP, and very few had ACP in writing. Patients generally understood their medical condition poorly, resulting in overestimation of survival probability post-CPR. This study lays the foundation for execution of future larger scale clinical trials, and ultimately, the incorporation of ACP into clinical practice in Malaysia. “How people die remains in the memories of those who live on,” and this is the reason why ACP is so important toward a patient's end-of-life care.
Limitation and suggestions
This study is limited by its small sample size. The study population is confined to UMMC and UMSC dialysis patients, which consisted mostly of UM staff, so it is not representative of the general ESRD population in Malaysia. The survey form used is not specifically designed for the purpose of this study; thus may have its limitations in terms of achieving the objectives of the study. Educational brochure for ACP is selected based on real life ACP stories and not ACP information leaflet. This may lead to inadequate transmission of ACP information to participants. Future larger scale studies consisting of bigger sample size and more dialysis centers would be more representative of the general ESRD population. Moreover, perhaps a look into the development of an ACP survey forms specifically for ESRD population and inclusion of dialysis withdrawal discussions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Palliative dialysis in end-stage renal disease. Am J Hosp Palliat Care. 2011;28:539-42.
- [Google Scholar]
- Definition and classification of chronic kidney disease: A position statement from kidney disease: Improving global outcomes (KDIGO) Kidney Int. 2005;67:2089-100.
- [Google Scholar]
- National Kidney Foundation practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Ann Intern Med. 2003;139:137-47. Erratum in: Ann Intern Med 2003;139:605
- [Google Scholar]
- Facilitating advance care planning for patients with end-stage renal disease: The patient perspective. Clin J Am Soc Nephrol. 2006;1:1023-8.
- [Google Scholar]
- Supportive Care for the Renal Patient (1st ed). New York: Oxford University Press; 2004. p. :1-267.
- The creation of an advance care planning process for patients with ESRD. Am J Kidney Dis. 2007;49:27-36.
- [Google Scholar]
- The impact of advance care planning on end of life care in elderly patients: Randomised controlled trial. BMJ. 2010;340:c1345.
- [Google Scholar]
- 21 st Report of the Malaysian Dialysis and Transplant Registry 2013: Death and Survival on Dialysis. Ch. 3 2013:32-48.
- Beyond autonomy: Diversifying end-of-life decision-making approaches to serve patients and families. J Am Geriatr Soc. 2005;53:1046-50.
- [Google Scholar]
- Factors influencing dialysis patients’ completion of advance directives. Am J Kidney Dis. 1997;30:356-60.
- [Google Scholar]
- The views of older Malaysians on advanced directive and advanced care planning: A qualitative study. Asia Pac J Public Health. 2007;19:58-67.
- [Google Scholar]
- Hope and advance care planning in patients with end stage renal disease: Qualitative interview study. BMJ. 2006;333:886.
- [Google Scholar]
- Exploring the opinion of CKD patients on dialysis regarding end-of-life and advance care planning. Nefrologia. 2011;31:449-56.
- [Google Scholar]
- Factors associated with decision-making about end-of-life care by hemodialysis patients. Saudi J Kidney Dis Transpl. 2010;21:447-53.
- [Google Scholar]
- Life-sustaining treatment preferences of hemodialysis patients: Implications for advance directives. J Am Soc Nephrol. 1995;6:1410-7.
- [Google Scholar]
- Practical considerations in dialysis withdrawal: “To have that option is a blessing”. JAMA. 2003;289:2113-9.
- [Google Scholar]
- Dialysis patients’ attitudes about cardiopulmonary resuscitation and stopping dialysis. Am J Nephrol. 1989;9:245-51.
- [Google Scholar]
- Controlling death: The false promise of advance directives. Ann Intern Med. 2007;147:51-7.
- [Google Scholar]
- How misconceptions among elderly patients regarding survival outcomes of inpatient cardiopulmonary resuscitation affect do-not-resuscitate orders. J Am Osteopath Assoc. 2006;106:402-4.
- [Google Scholar]
- The influence of the probability of survival on patients’ preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994;330:545-9.
- [Google Scholar]
- Resuscitation decision making in the elderly: The value of outcome data. J Gen Intern Med. 1993;8:295-300.
- [Google Scholar]
- Advance directives for medical care – A case for greater use. N Engl J Med. 1991;324:889-95.
- [Google Scholar]
- Diagnosis disclosure in cancer patients – When the family says “no!”. Singapore Med J. 2002;43:533-8.
- [Google Scholar]
- End-of-life care preferences and needs: Perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:195-204.
- [Google Scholar]
- National Kidney Foundation. Initiation or Withdrawal of Dialysis in End Stage Renal Disease: Guidelines for the Health Care Team. New York: National Kidney Foundation; 1996.
- Renal Physicians Association; American Society of Nephrology Working Group. A new clinical practice guideline on initiation and withdrawal of dialysis that makes explicit the role of palliative medicine. J Palliat Med. 2000;3:253-60.
- [Google Scholar]
- Clinical practice guideline on shared decision-making in the appropriate initiation of and withdrawal from dialysis. The Renal Physicians Association and the American Society of Nephrology. J Am Soc Nephrol. 2000;11:1340-2.
- [Google Scholar]
- Preferences for dialysis withdrawal and engagement in advance care planning within a diverse sample of dialysis patients. Nephrol Dial Transplant. 2010;25:237-42.
- [Google Scholar]






