Translate this page into:
Communication Needs of Patients with Breast Cancer: A Qualitative Study
Address for correspondence: Dr. Mrayam Rassouli; E-mail: rassouli.m@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Since communication is considered to be one of the central concepts in caregiving practices, this study aims to examine the perception of women with breast cancer in terms of their communication needs.
Methods:
In this qualitative study, 20 participants (9 women with breast cancer, 10 of health-care professionals, and one family caregiver) were selected through purposive sampling, and a face-to-face semi-structured interview was conducted with each of them. After data collection, all interviews were transcribed and reviewed, and categories were extracted. The data were analyzed with Conventional Content Analysis of Landman and Graneheim using MAXQDA10 software.
Results:
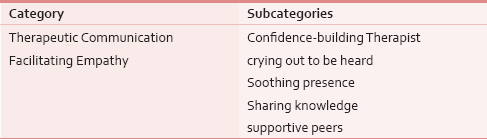
The analysis resulted in two extracted categories: “therapeutic communication” and “facilitating empathy”, and five subcategories: “trust-building therapist”, “crying out to be heard,” “seeking a soothing presence,” “sharing knowledge,” and “supportive peers”.
Conclusion:
Identifying and promoting the communicative needs of patients could lead to a considerably better care of patients under treatment. Therefore, therapeutic communication, as an integral part, should be incorporated into the care plan for patients with breast cancer and their families in the Oncology and Palliative Care wards.
Keywords
Breast cancer
Communication needs
Qualitative study
INTRODUCTION
Breast cancer is one of the most frequent malignancies among Iranian women, thus is the focus of attention of the health authorities due to the challenges of women during reproductive age as well as lower age distribution as compared to other countries.[12] The disease incidence rate has been on the increase in recent years, and studies indicate that the survival of the patients was in the range of 88%, 5 years after diagnosis and 80%, 10 years after diagnosis.[3]
Due to the high energy consumption in the face of cancer diagnosis and treatment, the feeling of instability due to the risk of recurrence, death, complications, financial problems, sexual problems, disruption of daily life, psychological problems such as stress and disruption of the personal, and familial and social interactions, changes occur in the quality of life of the patients with cancer, so much so that they find themselves in a state of uncertainty and extreme helplessness.[4] Therefore, these patients are in desperate need for both spiritual and psychosocial support.[5] Among other needs to mention are the need for a close and intimate relationship, respect from medical team, communicating effectively with medical personnel, and receiving information.[6]
Studies have shown that in the care and support domains, patients face significant unmet supportive care needs.[4] Identifying and addressing the unmet needs of patients with breast cancer are of prominent importance inasmuch as these two factors substantially boost the quality of life.[7] Patients with cancer are in need of comprehensive care.[8] Therefore, it is essential that health-care providers, such as nurses, develop a comprehensive understanding of the needs of patients which per se requires good communication.[9] To provide high quality and safe care for patients, communication and interaction between team members and patients are crucial.[10]
Communication is a form of interactive behavior, and thus professional interactions of health-care team are regarded as a communicative process in providing care to the patient.[11] In some studies, “Communication” has been referred to as the main theme by both the patient and families.[1112] The studies conducted over the past decade view communication as the need resulting in patients’ comfort, provision of quality care, a positive impact on the outcome, and response to treatment of patients.[1314] The results of a study carried out, showed that good relationship with patients has a significant effect on patient's participation in treatment, care and follow-up processes as well as accepting treatment regimen.[15161718] In the absence of proper communication, patients’ needs and priorities will be neglected in the caring process.[18] Therefore, nurses are required to take the nursing care into consideration based on patients’ perceived needs to help remove the concerns of patients.[19]
Given the dramatic rise in the number of women with breast cancer in Iran, and in light of convictions and cultural setting of the cancer women, relating to the problems stemming from lack of feminist symbolism and its concomitant complications, and the fact that there has not yet been any study conducted on the communicative needs of the patients with breast cancer, and taking into account the notion that “communication” is a culture-based conception,[20] researchers are hoping to take the necessary measures to plan care provision modules for these patients by identifying their specific needs and concerns and developing a better understanding of the main concerns of patients so that the medical personnel, while attending to the patients’ main concern, will be able to provide protective measures appropriate for them. This study aims to explain the perception of women with breast cancer in terms of their communication needs.
METHODS
According to the research question, qualitative research method with the approach of conventional content analysis to explain the understanding of the communication needs of women with breast cancer was used. Conventional content analysis is an inductive approach that aims to describe the phenomenon on the grounds of encoding and extraction of categories from the available data.[21] Using this method, an in-depth investigation of the patients’ real-world experiences and behaviors and an explication of the notion in question have been provided.
Setting and participant selection
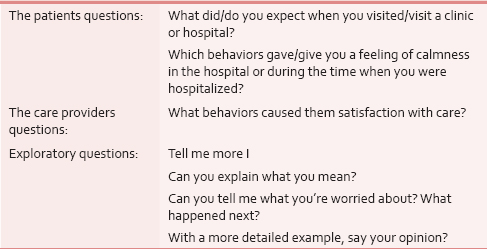
The study population consisted of women with breast cancer referrred to palliative care or oncology wards, their family caregivers, and health-care providers. In this study, the research setting was based on the type of qualitative research, real and natural environments and places where cancer patients were available. This being so, the study was carried out across the Shohada-ye-Tajrish and Taleghani Hospitals of Tehran (capital of Iran) affiliated to Shahid Beheshti University of Medical Sciences as referral centers of cancer patients from around the country. Women diagnosed with breast cancer and their families’ caregivers who knew about the disease and were able to speak Farsi, were selected based on purposive sampling method. The criterion for the selection of care providers was at least 1 year of work experience in the oncology clinics and departments. To collect data, in-depth semi-structured interviews were conducted using open-ended questions. The researcher explained to the participants the aim of the study and after their oral consent to participate in the study; the place of interview was selected after consulting the participants. Since patients were considered the key participants in this study, and to comply with maximum flexibility, we tried samples of breast cancer patients with different demographic characteristics such as age, marital status, education level, elapsed time since the diagnosis, type of treatment (including chemotherapy, radiation, and surgery) as well as their different stages of the disease, i.e., from Grades II, III, and IV and different stages of the disease, i.e., from grade II, III, and IV. Interviews took between 30 and 90 min per session, and from June to July 2015 and continued until data saturation was reached, i.e., no new categories emerges, and to round off analysis.[21] Using central questions, the researcher studied the participants’ experiences and their understanding of the subject to be studied. Sample interview questions from the participants were shown in Table 1.
Data analysis
The process of data analysis was carried out in accordance with the recommended steps by Graneheim and Lundman.[22] Interviews were transcribed and recorded with the permission of the participants and was read many times. Initial codes were extracted. The codes were then merged and classified on the basis of similarities. Finally, both the concept and content of the data were extracted. Data collection and analysis, using MAXQDA 10 software, were done simultaneously.
Following analysis, four criteria of Lincoln and Guba: Credibility, confirmability, dependability, and transferability were used to evaluate the qualitative research.[23] In this study, in a bid to solidify the reliability of data, the researcher was in continuous involvement with the data for 1 year during the study period, and all the data and interview transcripts and the list of categories were reviewed by other researchers with qualitative research background, and coded under control process by the members of each interview. The initial coding of each interview was returned to the interviewee at the early stage of analysis to determine the accuracy of data. However, the confirmability of the data was verified by two auditors familiar with qualitative research. As for the validation of the research, the researcher accurately recorded and reported the research steps and procedures to make it possible to investigate the research by others.
Ethical considerations
To observe ethics in research, an informed consent form was completed by all the participants after seeking approval from the relevant hospitals. At the beginning of the interview, the purpose of research, method of interview, confidentiality of the data, and their freedom to enter or exit the study was explained to the participants. The time and place of interviews were also coordinated with the participants so that they could fit it into their routine schedule and thus having ample time for interview and participation.
RESULTS
In this study, 20 participants consist of 9 women with breast cancer, and 6 physician and 4 oncology nurses and 1 family caregiver were analyzed. The average age of patients was 43/36 years (range 35–61). 8–80 months had passed since the initial diagnosis. Seven of nine patients underwent total mastectomy, one of them underwent breast-conserving surgery and one breast lumpectomy.
A total of clinical nurses were recruited (3 females and 1 male) from oncology ward and supportive/palliative care clinic of the Shohada-ye Tajrish and Taleghani hospitals (affiliated to Shahid Beheshti University of Medical Sciences), holding a bachelor's degree in nursing and married. Furthermore, six physicians (2 general practitioners from cancer Clinic, 2 surgeons, and 2 oncologists) whose work experience ranged from 3 to 21 months (average 10 months) were included.
After continuously analyzing and comparing the data and the subcategories, two main categories: “therapeutic communication” and “facilitating empathy” were extracted which is the outcome of the experience and understanding of the participants. The description is as shown in Table 2.
Therapeutic communication
The need to establish communication between the health-care team and patients is important so much so that it helps streamline treatment; as viewed by the participants. The participants need to communicate with patients, and their health-care team is of paramount importance to keep pace with, and thus improve treatment. “Trust-building therapist,” “soothing presence,” and “crying out to be heard” are the subcategories forming the main category.
Trust-building therapist
Trust is the fundamental factor in any relationship. A sound patient–physician relationship based on trust, reduces patients’ fears and anxiety, thus will lead to their satisfaction and preservation of their spirit.
“The very first time I went into get my pathology report, my legs became numb from knees down, and sat on the stairs fearing that it was cancer that knocking the door. The doctor said in a comforting and kind tone that I was facing a disease which should be worked out in tandem….it would be completely cured if you wanted so. With complete serenity on the side of the doctor, I got the feeling it was not meant to have a mortal fear of cancer.” (P1)
To the participants, good humor and friendly behavior mainly account for factors in building trust between the patient and the therapist. The most important conduct which the patients expect from their doctors and caring nurses, in the process of chemotherapy, was the practice code of ethics and appropriate treatment; the patients need “cheerfulness,” “sincerity,” and “good temper.” Patients’ experiences show that whenever treatment is associated with kindness and cheerfulness, the patient would experience a sense of trust toward the health-care team.
“Just the physician coming in cheerfully and asking me how you are today Miss Maryam…feels great…having trust for cancer patients are everything.” (P4)
During the course of the research, some of the participants believed that doctors’ ill temper and failure of initiate communication were the main obstacles of the treatment follow-up: “Every patient has a particular problem with this disease, and doctors do not set the scene for the patient to tell her improper conduct.” (P3)
Believing the pain and discomfort of the patient and being sensitive to the needs and conditions was a demand by other patients.
“I used to go to hospital. my oncologist was very cranky and didn't spend enough time for none of her patients. I could not even say I had mouth sores. She said everybody has the same problems, It is not just you, so stop moaning. since then, I stopped seeing her.” (P7)
Soothing presence
To the patients, physical presence and availability of health-care providers, particularly nurses, caused relief and maintained morale and satisfaction in them. Patients expressed a soothing presence of the nurse through words such as availability, talking, touching and caring, and paying attention to their questions and expressed their appeals. “The nurse was by my bedside anytime I needed her.” (P5)
A nurse with 19 years of work experience in the oncology ward believed that understanding the needs of patients and presence is in a way an art of nursing. She says: “A woman who has cancer, and underwent multiple courses of treatment, might not wish to communicate. Here, the situation calls for her facility to understand the patient and the patient, on the other hand, comes to the conclusion that we will be beside her till the end.” (P7)
Nurse's presence at the bedside is so important that it leads to trust, intimacy, and mutual peace. Patients believe that nurses’ absence causes a feeling of loneliness and anxiety.
“One night I was suffering from severe nausea. The caring nurse kept coming to my bedside hundred times until morning. I am dead sure she did not sleep the whole night. She held my hand and asked how I felt. the pain diminished. the following day I was keen to see my nurse again.” (P3)
As also asserted by the care providers, physical presence and availability of the nurse will have an important role in calming the patient, to the extent that it is part and parcel of the nursing major mission statement. “These patients are very sensitive. emotionally imbalanced, and are often agitated and anxious. I always try to sit and talk with them anytime I am free because it is very closely intertwined with our mission. the important thing is that you are available to patients and check them up from time to time, and feel them when you are next to him/her even for 2 or 3 min or 3 min.” (N9)
Crying out to be heard
Of other communication needs associated with cancer patients, pointed out over and over, is the need to understand the patient by the treatment team, especially nurses. A patient admitted at the final stages of her illness, being understood by the nurse helps reduce pain and increases the hope of recovery.
“Grinding my teeth, morphine had no effect on the severe bone pain and my nurse understood me very well. She told me I should beat cancer, many patients were cured in this way. If there is hope, the drugs would work better…this made me feel less pain.” (P6)
“Based on my experience, there ought to be a strong relationship with mutual understanding between the patient and the care provider. I had a patient who was in her final stage of her disease, after talking to her, I could see a smile on her face….in other words, she was happy. Nurses are duty-bound to create hope for the future in them by developing positive thoughts.” (N4)
Facilitating empathy
Despite having disease-related functional limitations and social activities, most patients underlined the need to communicate with their peers about sharing experiences acquired during disease process including the treatment signs and complications as well as the influence of peers in boosting morale and thus help them overcome social withdrawal and isolation. Therefore, another category which was extracted in this study was labeled facilitating empathy, which itself is divided into two subcategories: “sharing knowledge” and “supportive peers.”
Sharing knowledge
Patients believe that sharing and transferring one's knowledge, acquired personally in the course of treatment, at individual level is the core component of individuals’ knowledge dynamics and will lead to an increase in the overall knowledge of individuals.
“I always told the people around me or other patients about what symptoms I experienced when I was on Tamoxifen.” (P5)
“I’ll be glad to tell other patients about the experiences I learned thus far…. I think that's helping them a lot.” (P6)
Supportive peers
Patients and caregivers often find ways to talk with people who have similar experiences to help them out with accepting and realizing the symptoms they might encounter during the course of the disease.
“The news of my breasts having been removed made me feels desperate. I blurted out that it would be much better for me to die. but then I found out that there were many folks out there just like me and I am not the only one. I got into a conversation with one of the ladies and gradually accepted the truth…. my spirit was there again.” (P2)
One family caregiver (patient's daughter) of one of the patients, on the issue of guiding and helping another patient's companion, says: “I came to know a lady at the hospital prayer room whose mother suffered from breast cancer too. She explained to me about the complications of the disease and what she has done for her mother…and that which doctor was better. She even gave me her cell phone number just in case.” Patient's daughter.
“Being with other ladies who have similar conditions (whose breasts have been removed) are very good. there should be a place to get together and express our problems, or even on a sight-seeing tour…this way the spirit of joy and happiness comes back to us.” (P3)
“We, a couple of ladies, decided to cooperate with a charity and do everything that we could for the others…tell them that they are not alone and we can defeat cancer…. what I mean is that these types of groups are very helpful so much so that folks like me will be able to make it back to the predisease life.” (P5)
“The development of this type of group was supported by close association of people who have experienced cancer in that it facilitates sharing experiences with each other and thus helps reduce fear as well…. we should help and bring patients together.” (P10)
DISCUSSION
The purpose of the present study was to explore the perception that patients with breast cancer had regarding their communications needs. Main categories emerged from the analysis of the participants’ experiences relating to the communication needs of the patients with breast cancer including “therapeutic communication” and “facilitating empathy.”
One of the main categories in this study was “therapeutic communication” which is regarded as an interaction interspersed with trust, respect, and good manners, being amiable and approachable among health-care personnel, especially doctors and nurses in providing care for patients with breast cancer and especially women who underwent mastectomy. However, a couple of issues raised by the participants in the study were discussed including aspects such as trust-building care provider, crying out to be heard, and soothing presence. Participants in the study expected medical team to listen to them, and understand their needs, believing that trust was the cornerstone of the therapeutic communication to improve the quality of primary medical care provision imbued with satisfaction. When patients realize that their health-care needs are neglected by the health-care providers, they would be disheartened, and lose hope down the road. Hence, these findings shed light on the importance of understanding the communication needs of patients. Therapeutic communication means utilizing specific strategies to encourage patients to express feelings and ideas, transference, acceptance, and respect for the patient.[24] Therapeutic communication is the process of initiating interpersonal communication toward providing better care and compatibility with both disease and treatment, with a view to developing the best possible quality of life in women with mastectomy.[7] Communications are the core requirement for setting the health-care goals. Yet, studies have shown that patients are not satisfied with the mode of communication established between them and their physicians.[25] In line with the results, the study by Esbensen et al., attributed the related factors to effective communication between medical staff and patients, doctor's good temper, empathy, and listening of the treatment team to the problems of patients, talking to the medical team, especially nurses, having the skills to communicate effectively to the presence of the nurse.[26] In addition, the ability of physicians to build trusting relationship accounts for one of his communicative skills.[27] Furthermore, physician manner and answering to patients’ questions are the main factors involved in building trust in them. These findings are consistent with the results reported in other studies.[2829] In Iran, doctors are patients’ confidante, and since time immemorial, patients expect the doctors to restore their health after God. Hence, physician's establishing good relationship with patients and making them sure of their health condition is the patients’ greatest need. On the other hand, as in this context, the relationship between doctor and patient is very limited because doctors are reluctant to disclose any diagnosis of cancer to the patient. Therefore, proper relation between them cannot be established upfront.[30]
In connection with the subcategories crying out to be heard and soothing presence, participants regard the need for nurse's constant presence and empathy, in the treatment course of disease and care, as one of the factors boosting morale, hope in the future, and calmness. In line with our study, the results of the research by Molazem et al., 2011,[31] indicate that patients comfortable at the nurse's presence and availability. The need for nursing presence is the main theme in a study by Yagasaki and Komatsu which is considered an important factor in chemotherapy so that the nurses are expected to be present for developing and coordinating patient care programs as well as facilitating interpersonal relationships among health-caregivers, whereas being proactive in the arena of preventive care and projecting the future needs of patients including checking the side effects.[32] Bright believes that the presence of a nurse, even a physical presence minus therapeutic action at times when treatment and palliative care fall short of the patient's needs, can change the quality of care from the patient's perspective.[33]
As viewed by the participants in the study, the nurse-patient communication is an intrinsic characteristic of the nursing mission and that, as a strong factor, provides calmness and recovery in patients. Therefore, sympathy on the part of nurses with patients has been viewed as one of the fundamental needs by cancer patients.[34] From the point of view of participants in the study, it means understanding concerns of patients by physicians or nurses, indicating the subcategory of “crying out to be heard.” In addition, it has been pointed out that to develop clinical communication with patients and their families, nurses should try to a spirit of empathetic communication.[35] As such, it can be said that for a mutual relationship and trust between the patient and the nurse both sides need to adapt to their needs, and thus develop a fair relationship based on honesty and empathy.
Facilitating empathy is another category extracted during the study. Most participants have noted the desire and the need for communication with peers, saying that sharing experiences and describing symptoms to peers boosts morale and helps to have a sense of usefulness and a deeper social interaction. To confirm these findings, ample evidence shows that social support, including peer support, is known to be the key element in reducing stress caused in the wake of cancer experience.[36]
In addition to highlighting the role of peers in the present study, patients with breast cancer beleive that sharing their experiences with their peers would boost morale and raise awareness. Most of the participants in this study preferred to communicate with their peers obtain information about the disease; they compare their own situation with them, learn from and teach them, and build morale and respond reciprocally. Toward that end, several studies on cancer patients indicate the positive role of peer support groups, stating that those patients who join cancer support groups are more active, and exercise more appropriate adaptive (coping) strategies to better control the disease and its complications.[3738] On the other hand, the formation of peer groups is considered effective as it can lead to an increase in knowledge, cancer patients’ satisfaction with quality of care, a sense of hope, improved personal relationships, expansion of social protection as well as being liked and accepted by others under similar conditions, and reduced social isolation.[3940] Experiencing psychosomatic disorders caused by diagnosis and treatment of cancer will pave the way for positive psychological changes; in other words, the development of posttraumatic growth in the cancer patients.[41] The need to communicate with peers, in the current study, is in a way suggestive of posttraumatic growth in survived patients. In a study of cancer patients, a high level of growth has been evidenced.[42] Previous studies had also shown that cancer patients in terms of “Relating to Others” have experienced degrees of their growth.[43] Current study also suggests that the need to communicate with peers in the cancer patients was even higher, and this is quite indicative of a rise in the level of attention and communication with individuals in Iran when they face problems including cancer. Despite the need felt by cancer patients for a high-profile presence of peers, there exist no support programs for cancer survivors and their families in Iran including psychosocial support and peer support programs. That may be due to the lack of guidelines, policy-making (planning), and professional training for care providers.[44]
One limitation of this study was that the qualitative research results cannot be generalized to the society, but can help prioritize the care provision for the cancer patients as well as the caring method, attitude, and interactions on the part of the health-care personnel.
CONCLUSION
In this study, the need for effective communication based on trust and ethical standards associated with nurses’ presence has been highlighted by patients diagnosed with breast cancer. Therefore, considering the results, the gravity of identifying communicative needs of patients and their families by health-care personnel for the purpose of maintaining health, and developing as well as improving effective coping skills are highlighted. In addition, the interaction between nurses and doctors has to be addressed in depth to improve the quality of patients’ quality of care.
Given the role of peer groups in support of patients with breast cancer, initiation of group treatment methods, based on sharing experiences with each other, and communication skills training workshops, to raise awareness and develop therapeutic communication skills for both nursing and therapy team, are recommended.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Health expenditure in initial diagnostic and treatment approach to non-metastatic breast cancer in Iran. Iran J Breast Dis. 2013;6:14-25.
- [Google Scholar]
- Cancer in Iran. Cancer Research Center, Shahid Beheshti University of Medical Sciences. Tehran: Dar Alfekr; 2008.
- Discovery of hidden patterns in breast cancer patients data using data mining to examine the data with a real data set. Iran J Breast Dis. 2015;8:59-64.
- [Google Scholar]
- Prevalence and correlates of the unmet supportive care needs of individuals diagnosed with a haematological malignancy. Acta Oncol. 2015;54:507-14.
- [Google Scholar]
- Iranian cancer patients’ perception of spirituality: A qualitative content analysis study. BMC Nurs. 2012;11:19.
- [Google Scholar]
- The Information needs of women who have undergone breast cancer surgery in the west of Turkey. J Cancer Educ 2005:1-6. DOI: 10.1007/s13187-015-0965-2
- [Google Scholar]
- Quality of life among patients with primary, metastatic and recurrent cancer. Eur J Cancer Care (Engl). 2009;18:84-96.
- [Google Scholar]
- Predictors of change in unmet supportive care needs in cancer. Psychooncology. 2010;19:508-16.
- [Google Scholar]
- Factors influencing communication between the patients with cancer and their nurses in oncology wards. Indian J Palliat Care. 2014;20:12-20.
- [Google Scholar]
- Nurse-physician communication in the long-term care setting: Perceived barriers and impact on patient safety. J Patient Saf. 2009;5:145-52.
- [Google Scholar]
- Frequency of nurse-physician collaborative behaviors in an acute care hospital. J Interprof Care. 2012;26:115-20.
- [Google Scholar]
- Collaboration, credibility, compassion, and coordination: Professional nurse communication skill sets in health care team interactions. J Prof Nurs. 2006;22:180-9.
- [Google Scholar]
- Patient opinion of the doctor-patient relationship in a public hospital in Qatar. Saudi Med J. 2011;32:293-9.
- [Google Scholar]
- Facilitating goals-of-care discussions for patients with life-limiting disease – Communication strategies for nurses. J Hosp Palliat Nurs. 2012;14:251-8.
- [Google Scholar]
- Communication and medication refill adherence: The diabetes study of Northern California. JAMA Intern Med. 2013;173:210-8.
- [Google Scholar]
- Medication communication between nurses and patients during nursing handovers on medical wards: A critical ethnographic study. Int J Nurs Stud. 2012;49:941-52.
- [Google Scholar]
- Nurse practitioner communication and treatment adherence in hypertensive patients. J Nurse Pract. 2011;7:654-9.
- [Google Scholar]
- Current status of palliative care – Clinical implementation, education, and research. CA Cancer J Clin. 2009;59:327-35.
- [Google Scholar]
- Ethical issues in the end of life care for cancer patients in iran. Iran J Public Health. 2013;42:188-96.
- [Google Scholar]
- Knowledge, attitude and performance of academic members regarding effective communication skills in education. J Educ Health Promot. 2012;1:42.
- [Google Scholar]
- Qualitative Research in Nursing: Advancing the Humanistic Imperative. (5th ed). Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
- [Google Scholar]
- Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105-12.
- [Google Scholar]
- Competing paradigms in qualitative research. Handbook of qualitative research. 1994;2:105.
- [Google Scholar]
- Perspectives on care at the close of life. Initiating end-of-life discussions with seriously ill patients: Addressing the “elephant in the room”. JAMA. 2000;284:2502-7.
- [Google Scholar]
- Being given a cancer diagnosis in old age: A phenomenological study. Int J Nurs Stud. 2008;45:393-405.
- [Google Scholar]
- Recipients’ perspective on breaking bad news: How you put it really makes a difference. Patient Educ Couns. 2005;58:244-51.
- [Google Scholar]
- Patient trust: Is it related to patient-centered behavior of primary care physicians? Med Care. 2004;42:1049-55.
- [Google Scholar]
- Interventions for improving patients’ trust in doctors and groups of doctors. Cochrane Database Syst Rev. 2006;9:CD004134.
- [Google Scholar]
- Cancer care in countries in transition: The Islamic Republic of Iran. In: Silbermann M, ed. Palliative Care in Countries and Societies in Transition. New York: Nova Scientific Publishe, Springer; 2016. [In press]
- [Google Scholar]
- Improvement in the nursing care quality in general surgery wards: Iranian nurses’ perceptions. Scand J Caring Sci. 2011;25:350-6.
- [Google Scholar]
- The need for a nursing presence in oral chemotherapy. Clin J Oncol Nurs. 2013;17:512-6.
- [Google Scholar]
- 2012. Presence in Practice: A Critical Hermeneutic Analysis (Unpublished dissertation) Department of Nursing, University of San Francisco, California. :50-56. Available from: http://gateway.proquest.com/openurl?url_ver=Z39.88-2004&res_dat=xri:pqdiss&rft_val_fmt=info:ofi/fmt:kev:mtx:dissertation&rft_dat=xri:pqdiss:3549766
- A comprehensive model for optimizing empathy in person-centered care. Patient Educ Couns. 2013;93:209-15.
- [Google Scholar]
- Nurses’ perspectives on the care provided to cancer patients. Cancer Nurs. 2010;33:E1-8.
- [Google Scholar]
- Implementing a one-on-one peer support program for cancer survivors using a motivational interviewing approach: Results and lessons learned. J Cancer Educ. 2014;29:91-8.
- [Google Scholar]
- Cancer support groups: A critical review of empirical studies. Psychooncology. 2007;16:379-400.
- [Google Scholar]
- Effects of supportive-expressive group therapy on survival of patients with metastatic breast cancer: A randomized prospective trial. Cancer. 2007;110:1130-8.
- [Google Scholar]
- How do patients who participate in cancer support groups differ from those who do not? Psychooncology. 2006;15:321-34.
- [Google Scholar]
- What do cancer support groups provide which other supportive relationships do not? The experience of peer support groups for people with cancer. Soc Sci Med. 2006;62:2565-76.
- [Google Scholar]
- Exploring the links between physical activity and posttraumatic growth in young adult cancer survivors. Psychooncology. 2011;20:278-86.
- [Google Scholar]
- Posttraumatic growth and its dimensions in patients with cancer. Middle East J Cancer. 2014;5:23-9.
- [Google Scholar]
- Posttraumatic growth after cancer: The importance of health-related benefits and newfound compassion for others. Support Care Cancer. 2012;20:749-56.
- [Google Scholar]
- Palliative Care in the Islamic Republic of Iran. In: Silbermann M, ed. Palliative Care to the Cancer Patient: The Middle East as a Model for Emerging Countries. New York: Nova Scientific Publisher; 2014.
- [Google Scholar]






