Translate this page into:
Concerns and Coping Strategies of Persons Under Institutional Quarantine During SARS-CoV-2 Pandemic
Address for correspondence: Dr. Sushma Bhatnagar, Department of Onco-Anaesthesia and Palliative Medicine, Dr. BRA-IRCH, All India Institute of Medical Sciences, New Delhi - 110 029, India. E-mail: sushmabhatnagar1@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
The World Health Organization has declared severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as a pandemic. The interventions employed by various health authorities in combating the infection may help in eliminating the threat; however, they have long-term cognitive and mental health effects on the population.
Aims:
The primary objective was to assess the prevalent concerns and coping strategies and perspectives in persons suspected of SARS-CoV-2 infection under institutional quarantine in India during the period from April 2020 to May 2020.
Setting and Design:
Its a cross-sectional observational study conducted in the National Cancer Institute, Jhajjar, India.
Methodology:
After ethical clearance, convenience sampling was done. Relevant demographic details were obtained. Health-care professionally administered questionnaire to assess psychological concerns and coping mechanisms. All statistics are deemed to be descriptive only.
Results:
The most common physical concern was fever seen in 37% of respondents, followed by cough in 31% and sore throat in 29%. In terms of emotional concerns, 55.3% of respondents were worried and 43% were anxious and 33% were sad. About 80.6% of participants selected support from family and friends helped them cope during the institutional quarantine. 57% maintained a daily routine, 70% selected praying, and 45% used music as a coping strategy. Only 2% felt that they were unable to cope.
Conclusion:
It highlights that the psychological impact of illness on affected individuals should not be overlooked as it may have the potential to cause major psychiatric morbidity. It also provides a crucial assessment of their coping mechanisms.
Keywords
Coping
emotional
psychological
quarantine
SARS-CoV-2
symptom
INTRODUCTION
The World Health Organization (WHO) has declared severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which started as an outbreak in China and then spread worldwide as a Public Health Emergency of International Concern and then a pandemic. As of May 22, 2020, the epidemic has caused 335,588 deaths out of 5,231,374 confirmed cases worldwide, and 3605 deaths out of 120,532 confirmed cases in India.[1] The incubation period of the infection is between 2 and 27 days with a median of 14 days due to which the WHO and the Center for Disease Control and Prevention (CDC) recommend 14 quarantine days.[2] The WHO and CDC and other health authorities globally are currently focusing on containing the COVID-19 pneumonia pandemic.[3] The intervention measures that are employed by various health authorities and government bodies in combating the infection may help in eliminating the threat during the time of uncertainty; however, the multivariate studies done on the previous outbreaks show that they have long-term cognitive and mental health effects on the population[4] as well as on medical teams.[56] An outbreak of a global pandemic causes fear and concern among many and reportedly influence the cognitive well-being of every individual.7 Previous studies on SARS, MERS and Ebola reveal a severity in emotional distress during the outbreaks of such epidemics.[6891011] The lives of infected individuals, family and friends, and the society are at stake due to the perpetuated potential effects of the SARS-CoV-2 and have serious mental effects.[45] It is vital to study the mental health well-being of the quarantined population and take proactive steps to minimize its detrimental effects during the SARS-CoV-2 pandemic.[4] This study aims to assess such concerns and identify the various coping mechanism used by such individuals and organize relevant mitigation strategies.
METHODOLOGY
The primary objective of the study was to assess the prevalent concerns and coping strategies, and perspectives in persons suspected of SARS-CoV-2 infection, under institutional quarantine in India during the period from April 2020 to May 2020.
Sampling participants
This is a cross-sectional survey conducted on the google documents platform. The pool of participants consisted of approximately 150 individuals admitted in the National Cancer Institute, Jhajjar, India. Eligible participants were enrolled in the study on a first-come, first-serve basis. Participants had to have indicated that they are fluent in English or Hindi to be eligible for this study.
Tools
We used a self-designed questionnaire survey tool which included the demographic details of the participant and questions regarding physical, psychological symptoms and coping mechanisms.
Data collection
Data were collected using the online questionnaire shown in Appendix 1. Following an informed consent form, the health-care professional administered questionnaire asking participants about the background, physical issues that concerned them, their emotional concerns, strategies that helped them maintain their mental well-being. Questions directly regarding physical, emotional concerns, and coping methods allowed multiple responses. Questions addressing the stress and perception regarding quarantine were single response and questions pertaining to their mental well-being were measured on a 5-point Likert scale. The responses were recorded directly on a spreadsheet.
Data analysis
Findings of the participant responses were analyzed. Categorical variables have been summarized as counts and percentages. All statistics are deemed to be descriptive only as the participant cohort was not derived from random selection.
RESULTS
Participants characteristics
From the pool of 150, the total sample size analyzed included, 103 participants. Those who did not give consent and those who did not understand English or Hindi were excluded. Of the 103 participants who completed the survey questionnaire, 82.5% were male and 3% were transgender respondents [Table 1]. Most of the participants were young and middle-aged adults, with 43.7% belonging to 30–50 years of age, closely followed by 38.5% of participants being <30 years of age. In terms of work background, 48.5% of respondents were self-employed, around 20% were employed in the government sector. Considering geographical distribution, there was not much difference in representations from north and south India, with 49.5% and 43% of participants, respectively.
| Sample characteristics | n (%) |
|---|---|
| Total (n) | 103 |
| Age | |
| <30 | 40 (38.8) |
| 30-50 | 45 (43.7) |
| 50-65 | 16 (15.5) |
| >65 | 2 (1.9) |
| Sex | |
| Male | 85 (82.5) |
| Female | 15 (14.6) |
| Transgender | 3 (2.9) |
| Work background | |
| Self-employed | 50 (48.5) |
| Employees (Govt) | 20 (19.4) |
| Employees (NGO) | 3 (2.9) |
| Professionals | 17 (16.5) |
| Student | 6 (5.8) |
| Homemakers | 3 (2.9) |
| Unemployed | 2 (1.9) |
| Others | 3 (2.9) |
| Geographical distribution | |
| North India | 51 (49.5) |
| South India | 44 (42.7) |
| East India | 4 (3.9) |
| North-East India | 3 (2.9) |
| Outside India | 1 (1) |
Physical and emotional concerns
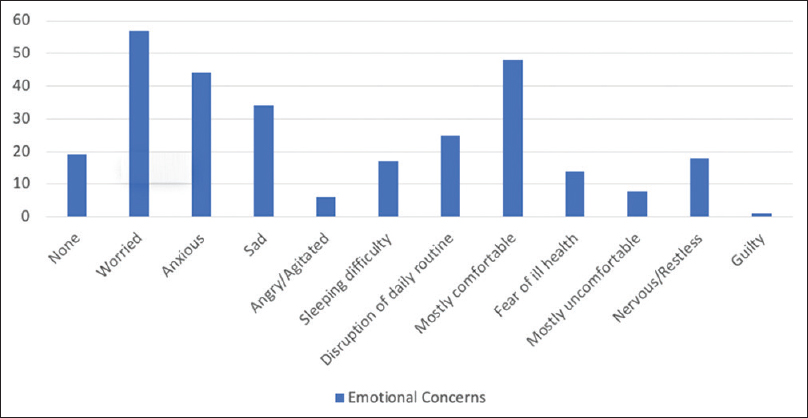
The most common physical concern was found to be fever seen in around 37% of respondents, closely followed by cough seen in 31%, then sore throat seen in 29%. A significant proportion at 27.2% did not have any physical concerns. Breathing difficulty, a significant morbidity was seen in 11.7% [Figure 1]. In terms of emotional concerns [Figure 2], 55.3% of respondents were worried and 43% were anxious and 33% were sad. A significant number of participants, that is, 46.6% were mostly comfortable.

- Physical concerns
- Emotional concerns
Coping mechanisms and mental health well-being
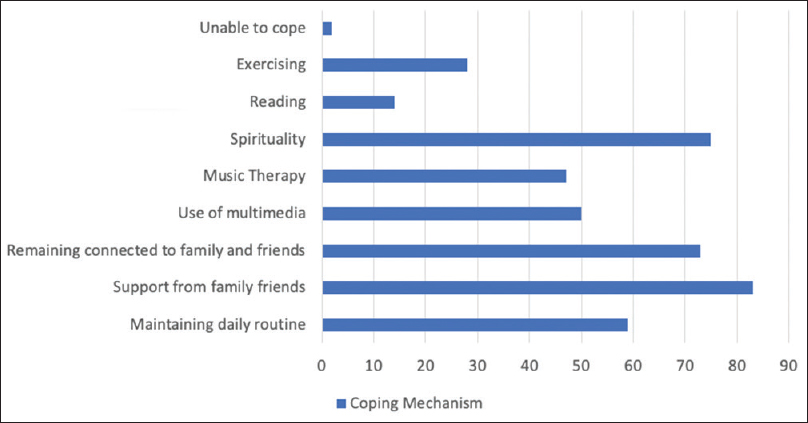
A vast majority, 80.6% of participants selected support from family and friends helped them cope during institutional quarantine and approximately 71% remained connected to family and friends during this period. Around 57% maintained a daily routine as a coping strategy, despite being institutionalized. About 70% of the respondents selected praying is what helped them cope better. The use of music as a coping strategy was found in 45% of participants. Only 2% of respondents felt that they were unable to cope [Figure 3].
- Coping mechanisms
Despite facing multiple difficulties during the institutional quarantine, 67% felt this was a necessary measure under the given circumstances, and around 14% said that they were not stressed at all. Approximately 12% felt that their life had become difficult during the quarantine. Almost 50% of respondents felt calm and their life is under well control, while a significant 40% were neutral about it. Only 14% were worried and felt that life is totally disrupted and a significant majority of 43% believed that it was not so. Approximately 46% disagreed that they had changed as a person and 38% had a neutral opinion about it. 58.3% felt that they did not need any counselling, but a significant 33% of participants responded that they did need it [Table 2].
| Psychological perceptions | n (%) |
|---|---|
| This quarantine | |
| Is an opportunity to help others | 20 (19.4) |
| Has made life difficult | 12 (11.7) |
| Is necessary | 69 (67) |
| Is unnecessary | 7 (6.8) |
| My life is under control: | |
| Strongly agree | 9 (8.7) |
| Moderately agree | 43 (41.9) |
| Neutral | 42 (40.8) |
| Moderately disagree | 9 (8.7) |
| My life is disrupted | |
| Moderately agree | 14 (13.6) |
| Neutral | 45 (43.7) |
| Moderately disagree | 38 (36.9) |
| Strongly disagree | 6 (5.8) |
| Quarantine has influenced | |
| Personality change | |
| Strongly agree | 2 (1.9) |
| Moderately agree | 14 (13.6) |
| Neutral | 39 (37.9) |
| Moderately disagree | 40 (38.8) |
| Strongly disagree | 8 (7.8) |
| Would value some counselling | |
| Yes | 8 (7.8) |
| No | 60 (58.3) |
| Maybe | 35 (33.9) |
DISCUSSION
Institutional quarantine was started to combat the rising cases of SARS-CoV-2 in the country. This survey was an attempt to conduct an assessment of physical symptoms, emotional and psychological experiences, and coping mechanisms among patients suffering from SARS-CoV-2 in a short time frame. There was a significant male gender predominance amongst the participants. Regarding findings from survey questions, the most common physical concern was fever and cough, which is consistent with the multi-centric Chinese data.[12] A significant 27% of participants of the study on institutional quarantine did not have any physical concern at all despite being in an institutional quarantine. These results are consistent with the epidemiology of the disease, where a significant number of infected individuals remained asymptomatic.[12]
A majority of patients were worried, anxious, sad, and agitated, indicating a significant presence of some psychological distress. Psychological distress is known to occur in response to situations of extreme sudden stress, such findings are seen in seen in previous research as well.[8] The possible contributor could be acute changes imposed on their daily life by policy decisions to contain the highly infective SARS-CoV-2 virus, which is still novel. Individuals put on sudden quarantine may view it as life-limiting event. It is important to acknowledge that they were residing within quarantine space which had very limited indoor spaces with all basic necessities catered to, but yet in very unfamiliar environment. These, along with misconception and poor level of awareness regarding the illness, can contribute to stress. The difficulty in sleeping that many respondents experienced could be attributed to this sudden loss of familiar environment and also to disruption of daily routine, an observation which in itself is a potential cause of distress among patients. A significant proportion of the population responded as not having any stress at all, which is an interesting finding considering a majority of respondents found quarantine a necessary intervention. These responses corroborate well with logotherapeutic basis for accepting difficult situations by “finding a meaning.” Logotherapy states that if a person knows the “why,” he can manage any “how.”[15] This finding also suggests the need for integrating awareness activities whereby those in quarantine are made aware about how they are contributing to community health by following the norms.
The most common coping strategy was found to be staying connected to family and friends. The significant role of family support in alleviating the loneliness and psychological distress has been demonstrated well in earlier research.[7] and reaffirmed in this study. Leisure coping activities such as reading, yoga, listening to music, use of social media are adaptive coping strategies commonly used to respond to psychosocial environmental demands. Music has a proven positive impact on the psychobiological system.[13]
Praying emerged as an important coping strategy, with 70% responses. Praying is an established religious coping mechanism as per evidence, which has helped the patient to get through the distress caused by institutional quarantine.[14] It helps through strengthening their sense of connectedness, deriving meaning for the experienced distress. Although a significant number of patients felt their life's routine was disrupted with the quarantine, and valued counselling, they did not perceive their life as being out-of-control. They were probably able to accept the disruption by making meaning of the situation as a necessary consequence of the unusual circumstances. This again suggests opportunities for therapeutic interactions by providing opportunities for venting, questioning, clarifications, and psychological counselling as needed to support emotional well-being and also respond to those who feel overwhelmed.[4] Though quarantine can be extremely distressing, it did not influence any changes in the personality of majority patients, thus, indicating the capability of individuals to tide over this short-term period of severe distress.
This study has several limitations. First, being a survey the findings reported will have certain inadequacies to them as an inherent drawback.[16] Second, the sample of participants may be different from the general population in variety of socio-demographic characteristics determining their background, perceptions, and level of knowledge. Thus, the findings of this study should be interpreted carefully considering the above mentioned limitations.
CONCLUSION
This is the first of its kind survey among Indian patients in institutional quarantine suffering from SARS-CoV-2 infection, exploring the psychological sequelae of infectious illness during the pandemic. It has highlighted that the psychological impact of this illness on affected individuals should not be overlooked as it may have a potential to cause a major psychiatric morbidity. This indicates the need for designing possible interventions to mitigate this sudden acute distress. It also provides a crucial assessment of their coping mechanisms, thus, paving the way for future research possibilities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Available from: https://covid19whoint/
- Focus on mental health during the coronavirus (COVID-19) pandemic: Applying learnings from the past outbreaks. Cureus. 2020;12:e7405.
- [Google Scholar]
- Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123-7.
- [Google Scholar]
- Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in China: A model of West China Hospital. Precis Clin Med. 2020;3:3-8.
- [Google Scholar]
- An evaluation of psychological distress and social support of survivors and contacts of Ebola virus disease infection and their relatives in Lagos, Nigeria: A cross sectional study − 2014. BMC Public Health. 2015;15:824.
- [Google Scholar]
- Psychological trauma of Middle East respiratory syndrome victims and bereaved families. Epidemiol Health. 2016;38:e2016054.
- [Google Scholar]
- Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31:318-26.
- [Google Scholar]
- Quality of life reported by survivors after hospitalization for Middle East respiratory syndrome (MERS) Health Qual Life Outcomes. 2019;17:101.
- [Google Scholar]
- Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708-20.
- [Google Scholar]
- Developing a measurement instrument for coping with occupational stress in academia. SA J Ind Psychol. 2019;45:a1653.
- [Google Scholar]
- Man's Search for Meaning: An Introduction to Logotheraphy. London: Hodder and Stoughton; 1962.
- Using survey methods in telehealth research: A practical guide. J Telemed Telecare. 2017;23:770-9.
- [Google Scholar]
Appendices
Appendix 1:
Pro forma
Title: Concerns and coping strategies of persons under institutional quarantine during SARS-CoV-2 pandemic
Date: UHID: Phone number/email id: Gender: Male Female Others Age: <30 years 30-50 years 50-65 years >65 years This represents my work background (select one)*
Student Professional Employee- NGO Employee-Government Self Employed Artist/Musician Other During the past few weeks under institutional quarantine, the physical issues that concerned me are (select your concerns)
No concerns cough fever breathing difficulty loose motion difficulty sleeping disruption of daily routines constipation Pain nausea, vomiting sore throat, nasal congestion feeling very weak, fatigue, decreased smell, decreased taste decreased appetite Other (specify). During the past few weeks under institutional quarantine, the emotional issues that concerned me are (select your concerns)*
No concerns worried, anxious sad angry, irritated overwhelmed, incapacitated difficulty sleeping disruption of daily routines Fear of acquiring infection Fear of worsening health Mostly comfortable mostly uncomfortable Nervous, panicky feeling guilty Restless Other: During the last few weeks with institutional quarantine, the strategies that helped with my mental well-being have been (select your concerns)*
Maintaining my daily routines at personal level Support from my friends/family Remaining connected with family and friends Staying updated on latest updates in the news, media Limiting mobile/media exposure Noticing my emotional status and trying to calm myself Prayers Listening to music Yoga Reading computer games searching for meaning I am unable to cope Others I feel this stress that I'm going through*
is an opportunity to help others has made life very difficult for all concerned is unjustified and unnecessary is necessary, given the circumstances I am not stressed at all Other I feel calm and my life is well under control (select a score)* Totally agree 1 2 3 4 5 Totally disagree I feel very worried and my life is totally disrupted (select a score) * Totally agree 1 2 3 4 5 Totally disagree This quarantine has influenced and changed me as a person (select your score * Totally agree 1 2 3 4 5 Totally disagree As of now, I would value some counselling *
Yes No May be Other: I belong to *
South India North India East India West India North East India central India Outside India
Appendix 2:
Study definitions
WHO defines confirmed case as
A person with laboratory confirmation of COVID-19 infection, irrespective of clinical signs and symptoms For confirmed asymptomatic cases, the period of contact is measured as the 2 days before through the 14 days after the date on which the sample was taken which led to confirmation. WHO defines a probable case as – i) for whom testing for the COVID-19 virus is inconclusive as reported by the laboratory. OR, ii) for whom testing could not be performed for any reason. WHO defines a suspect case as
A patient with acute respiratory illness AND a history of travel to or residence in a location reporting community transmission of COVID-19 disease during the 14 days prior to symptom onset. A patient with any acute respiratory illness AND having been in contact with a confirmed or probable COVID-19 case (see definition of contact) in the last 14 days prior to symptom onset; A patient with severe acute respiratory illness (fever and at least one sign/symptom of respiratory disease, e.g., cough, shortness of breath) AND requiring hospitalization AND in the absence of an alternative diagnosis that fully explains the clinical presentation.






