Translate this page into:
Concerns of Health Care Professionals Managing non-COVID Patients during The COVID-19 Pandemic: A Descriptive Cross- Sectional Study
Address for correspondence: Dr. Sushma Bhatnagar, Room No-242, 2nd Floor, Department of Onco-Anaesthesia and Palliative Medicine, Dr BRAIRCH, AIIMS, New Delhi, India. E-mail: sushmabhatnagar1@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
The coronavirus pandemic has put an unprecedented burden on the health-care workers who are the cornerstone of the work system, preparing to mitigate its effects. Due to the lack of protective equipments, guidelines for managing patients, or proper training and education regarding the same, health care professionals (HCPs) working in non-COVID areas may face even greater problems than those working in COVID areas of a hospital. Our aim was to find out the concerns of HCPs working in non-COVID areas.
Subjects and Methods:
After obtaining institutional ethics approval, a descriptive cross-sectional study was planned. An online Google-based questionnaire was rolled out to all doctors through various social media platforms who were dealing with COVID-negative patients.
Results:
We received a total of 110 responses. 84.5% of participants were concerned about the risk of infection to self and family, 67.3% were concerned by the disruption of their daily activities. 56.4% of HCPs were disturbed by the lack of any concrete protocol for patient management. Less staff availability, delay in discharging duties toward their patients, and increased workload were other concerns. More than half of the doctors received N-95 masks whenever required and were trained in donning and doffing of Personal protective equipment. Sixty-eight percemt of our respondents labeled their current quality of life as stressful.
Conclusion:
It is the need of the hour to develop a comprehensive strategy focussing on the above challenges that HCPs working in non-COVID areas are facing. This will go a long way in not only providing holistic care to the patients but also in controlling this pandemic.
Keywords
Challenges
health care professionals
non COVID
pandemic
INTRODUCTION
The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has resulted in more than four million infected cases and three hundred thousand deaths, has placed a sudden inadvertent strain on health-care services worldwide.[1] This disease can be transmitted even in the asymptomatic phase and hence carries a high risk for health-care professionals (HCPs).[2] Health care workers are the backbone of any working system during a pandemic. All other system elements such as tools and technologies, organizational conditions, work tasks, and environmental factors serve to empower the health-care workers to perform his or her role to their maximum capability, safely and effectively. Therefore, any effort to strengthen the work culture must be HCP-centric to facilitate their acceptance and implementation. Center for Disease Control (CDC) has recommended the use of personal protective equipment (PPE) that includes full-body covering gown, double pair of gloves, and either an N95 respirator with face shield/goggles or a respirator to ensure minimum risk of acquiring the infection.[3] However, these precautions are not routinely taken in the daily care of a patient suffering from generalized respiratory illness. Thus, all those HCPs working in designated non-COVID areas are faced with the task of dealing with patients without any PPE. They are required to work long hours with inadequate resources under significant pressure and less than adequate staff while accepting the dangers associated with close interaction of sick patients. HCPs, like everyone else, are vulnerable both to the disease itself and to rumors and incorrect information that may increase their anxiety levels.
The state of lock-down in various parts of the world has led to the halting of essential services. Transport has been affected globally. The HCPs are also affected by this without any exception. This has resulted in further stress and poorer quality of life in HCPs. Those HCPs who are working in the frontline dealing with positive COVID-19 patients are being hailed as heroes. Although the challenges faced by them are nonetheless lesser and even at times greater than those HCPs working in non-COVID areas, a lot of public and government support are rallying toward their protection. With this background, our study attempts to find out the concerns and challenges of those HCPs who are managing patients in non-COVID areas and the coping strategies they are adopting for the same.
SUBJECTS AND METHODS
After institutional review board approval and ethical clearance (IEC-403 / 08.05.2020), this descriptive cross-sectional study was conducted among HCPs who were working in designated non-COVID areas of a hospital and who were not dealing with any known infected COVID-19 patient. Health-care workers who had completed their MBBS, willing to participate in the study who understood English, were included in the study. Those HCPs who were posted in COVID wards of a hospital and dealing with a known infected patient were not included in the study. To maintain homogeneity in response we decided to include only doctors in our study.
We used the technique of snowball sampling. With the help of Google form, an online questionnaire was developed containing a consent form that appeared before the participants were directed to the main section consisting of the concerned questions. The link of the questionnaire was sent through various social media platforms, including WhatsApp and E-mails to the contacts of the investigators. The participants were encouraged to pass on the survey to as many people as possible. Thus, from the first point of contact, the link was forwarded to many people. On receiving and clicking the link, participants were auto directed to a section containing information about the study and consent. After they accepted to take the survey, participants had to choose their options of choice against a set of several multiple-choice questions that appeared sequentially. This questionnaire was revised and validated by a panel of five medical professionals from different health fields.
Sample size
Since this type of study has not been conducted before, we decided to take a sample size of convenience.
Statistical analysis
The data were entered in the Microsoft excel chart, and results were interpreted accordingly. Percentages were used in the conclusion of data.
RESULTS
A total of 150 questionnaires were sent out. One hundred and ten participants replied, and all of them were found to be eligible according to our inclusion criteria. The maximum number of participants, i.e., 22.72% belonged to the department of onco-anesthesia, 10.90% of the participants were working as Medical Officer in various health centers. There was one participant each belonging to the orthodontics, pathology, and physical medicine and rehabilitation department that together made up 2.72% of our cases. About 62.72% of the participants were in the age group of 30–40 years, 60% of the responders were male. The majority of our HCPs were senior residents (44.54%) [Table 1].
| Non-COVID areas where HCPs were working | |
|---|---|
| Number of cases (n=110), n (%) | |
| Onco-anaesthesia | 25 (22.72) |
| Palliative Medicine | 12 (10.90) |
| Anaesthesia and Critical Care | 12 (10.90) |
| Medical Oncology | 16 (14.54) |
| Medicine | 10 (9.09) |
| Obstetrics and Gynecology | 9 (8.18) |
| Pediatrics | 4 (3.63) |
| Surgery | 5 (4.54) |
| Psychiatry | 2 (1.81) |
| Post-MBBS Medical Officer | 12 (10.90) |
| Others | 3 (2.72) |
| Age group (years) | |
| <30 | 30 (27.27) |
| 30-40 | 69 (62.72) |
| 40-50 | 5 (4.54) |
| >50 | 6 (5.45) |
| Gender | |
| Male | 66 (60) |
| Female | 44 (40) |
| Designation | |
| Medical Officer | 12 (10.90) |
| Junior Resident | 18 (16.36) |
| Senior Resident | 49 (44.54) |
| Consultants | 31 (28.18) |
HCPs: Health care professionals
Out of 110 participants, 93 felt that there was a risk of infection to self and family, whereas three participants did not feel challenged at all in their personal life. Other challenges faced by HCPs were not having any insurance back up and salary cut [Figure 1]. Sixty-two participants felt that they were troubled by the lack of any concrete protocol for patient management in their respective work areas. Not wearing PPE throughout their duty period, too many guidelines regarding patient management and hesitancy of patients to reveal their contact as well as travel history were other significant challenges faced by the health workers in their workplace [Figure 2].
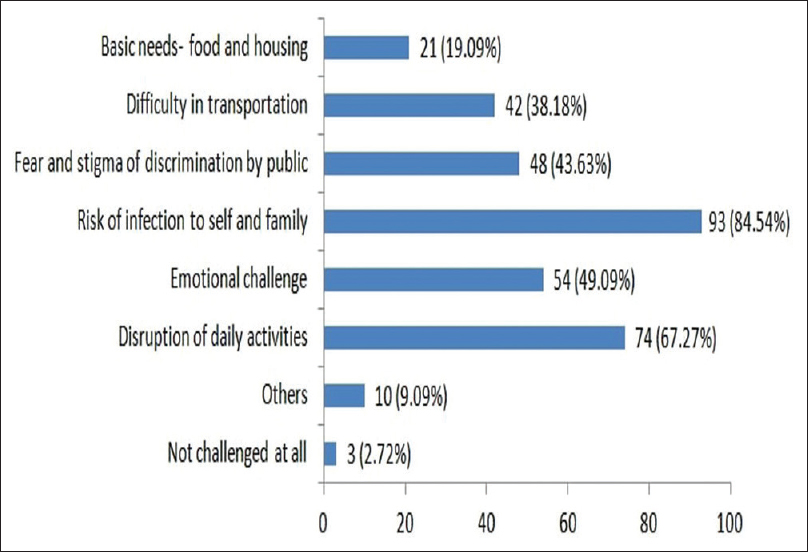
- Bar diagram showing challenges faced by health care professionals at personal level
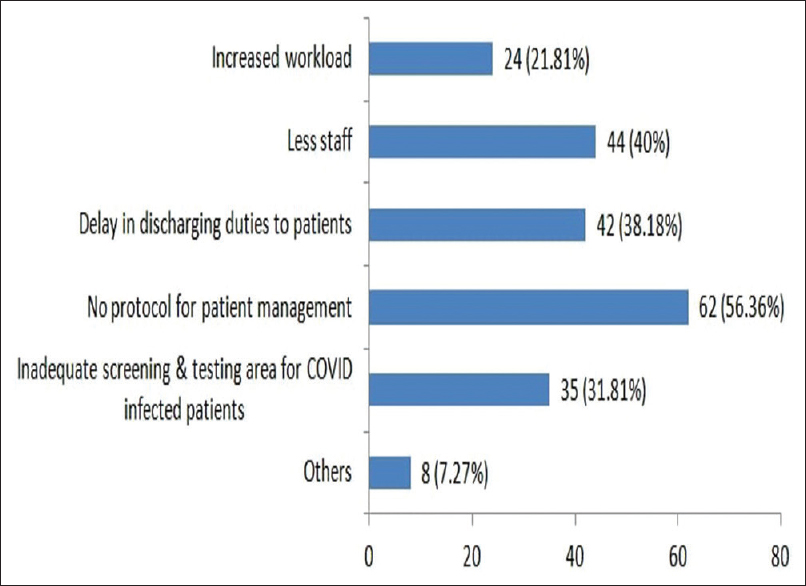
- Bar diagram showing challenges faced by health care professionals in their respective work area
About 58.18% of participants were given N-95 masks whenever they wanted, whereas 38.18% received PPE during their duty period. About 2.72% of participants were equipped with neither PPE nor N-95 masks in their respective work areas [Table 2]. 56.36% of participants had undergone a formal training class on donning and doffing, whereas only 40% of the participants were confident of wearing and dispensing PPE properly [Table 3]. About 56.36% of participants felt difficulty in practicing social distancing at their workplace, whereas 52.72% of them were hesitant to attend to patients. About 71.81% of our responders wanted that all admitted patients undergo COVID testing to rule out their infection. About 11.8% rated their present quality of life as very stressful, while 8.2% did not feel any stress at all [Table 4].
| Difficulty in getting N-95 mask in ward, n (%) | Difficulty in getting PPE in ward, n (%) | |
|---|---|---|
| Available whenever required | 64 (58.18) | 42 (38.18) |
| Available for suspected positive patients | 33 (30) | 48 (43.63) |
| Available for invasive procedure only | 7 (6.36) | 9 (8.18) |
| Available sometimes for invasive procedure only | 6 (5.45) | 8 (7.27) |
| Not available at all | 3 (2.72) | 3 (2.72) |
PPE: Personal protective equipment
| Number of participants (n=110), n (%) | |
|---|---|
| Any training or class in donning and doffing of PPE | |
| Yes | 62 (56.36) |
| No | 48 (43.63) |
| Confident in donning and doffing | |
| Yes | 44 (40) |
| No | 35 (31.81) |
| Maybe | 31 (28.18) |
PPE: Personal protective equipment
| Number of participants (n=110), n (%) | |
|---|---|
| Difficulty in practicing social distancing at work place | |
| Difficult | 62 (56.36) |
| Not difficult | 48 (43.63) |
| Hesitant to attend to patients | |
| Yes | 58 (52.72) |
| No | 52 (47.27) |
| Wants all admitted patients to undergo COVID testing | |
| Yes | 79 (71.81) |
| No | 16 (14.54) |
| Maybe | 15 (13.63) |
| Present level of stress | |
| No stress at all | 9 (8.2) |
| Feels stress sometimes | 25 (22.7) |
| Feels stress most of the time | 34 (30.9) |
| Feels stress all the time | 29 (26.4) |
| Feels stress even when at home | 13 (11.8) |
About 73.63% of HCPs felt that promotion of social distancing in their work helped them to deal with patients in the ward in an efficient manner. 64.54% of participants used telemedicine, whereas 34.54% of participants felt the compassion and empathy from leadership helped them in dealing with patients [Figure 3]. About 72.72% of health workers maintained their mental well-being by communicating with their friends and family. In comparison, 4.54% HCPs felt that they were unable to cope at all with the recent change in their professional lives due to this pandemic [Figure 4].
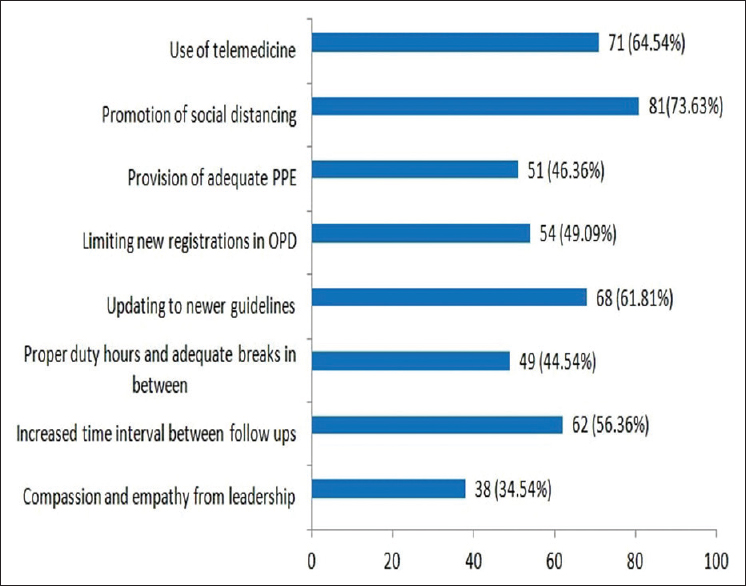
- Bar diagram showing strategies taken at workplace which helped health care professionals to deal with patients in an efficient manner
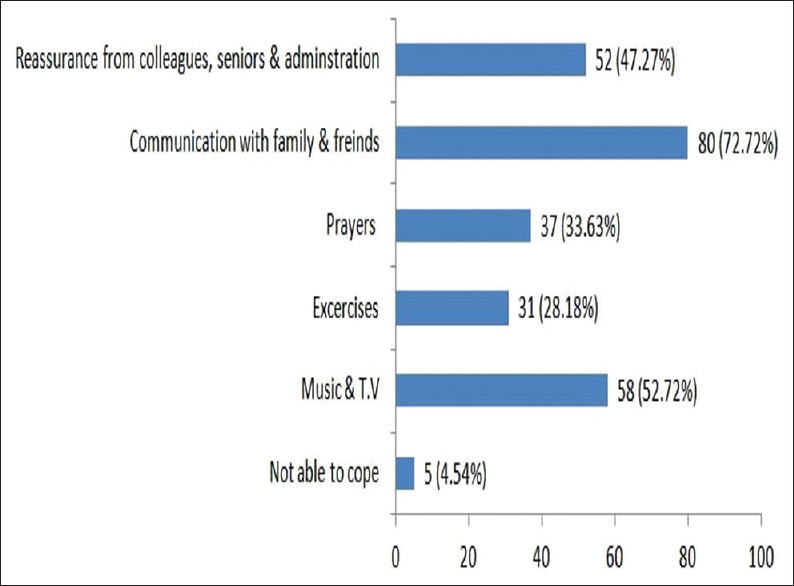
- Bar diagram showing strategies taken for mental well being
DISCUSSION
With the rise in the number of infected cases of COVID-19, HCPs are facing heavy workload and high risks of infection throughout the world. Health-care workers are the cornerstone for building an efficient system during the times of a pandemic outbreak. Hence, their health and safety remain of utmost importance to provide continuous and safe patient care. It was found that HCPs caring for patients during Middle east respiratory syndrome and SARS outbreak were found to work under very high level of stress due to potential risk of high infection, stigma of discrimination, uncertainty about future along with lack of any radical support.[45] Similar results are reflected in our study where the greatest concern of health workers are the risk of infection to self and family. As part of their chosen profession, doctors accept the risks associated while caring for their patients, but exhibit concern about transmitting this hospital-acquired infection to their family members, especially those who are immunocompromised, elderly, and suffering from chronic diseases.[6] SARS-CoV-2 can be transmitted even when the disease progresses asymptomatically in some patients.[2] In a case series of hundred and thirty-eight patients treated in a Wuhan hospital, forty patients (29%) were HCPs. Out of them, 2 (5%) worked in the intensive care unit, 7 (17.5%) in the emergency department, and 31 (77.5%) in general wards. The source of infection was a patient admitted to the surgical department for abdominal symptoms who were asymptomatic.[7]
Disruption of daily activities and difficulty in transportation are common during the state of lockdown, and halting of essential services have added a further cause of concern for health workers.[8] Fear and stigma of discrimination by the general public was another major concern of health workers participating in our study and are being prejudiced against by labeling them as “modern-day plague spreaders.”[9]
Many HCPs are overwhelmed by a lack of concrete management protocol for patient care. There is also delay in discharging duties towards the patients admitted in wards as there are various logistic issues, including curtailing of outpatient services in various health centers.[10] A major chunk of support staff has been pulled to work in COVID areas that have resulted in further work pressure among the staff who are caring for patients in non-COVID area.
Many health care workers were not aware of the proper sequence of use, disposal, and replacement of PPE. Reports have come from various centers worldwide where HCPs had to resort to reusing single wear PPEs.[11] HCPs should take additional measures for contact during aerosol-generating procedures alongside standard measures for droplets, close contact, and airborne transmission. Control measures specific to the invasive procedures must be considered. In the event of a cardiac arrest, cardiopulmonary resuscitation measures cause aerosolization of the pathogens that could result in the wide dissemination of virus particles to clinicians, health care staff, and other patients.[12] Apart from this, lack of training resulting in improper donning of PPE as well as wearing an ill-fitting mask can increase the risk of infection.[13] Similar to our findings, various reports have emphasized the need of adequate provision along with training in the proper use of PPEs.[14] It is difficult to provide safe healthcare without providing adequate PPE to health workers which might result in the sense of inadequacy regarding the delivery of their duties.
Social distancing has become a vital component of reducing the spread of the virus. According to CDC guidelines, individuals should remain 6 ft or 2 m apart from each other.[15] However, it is often difficult to practice social distancing in the ward and the outpatient units where lack of space along with overcrowding of patients is a major issue in a tertiary level hospital. In our study, participants felt the same. Although HCPs were aware of the risk of infection associated while treating patients in the hospital, more than half of our study participants were not at all hesitant to attend to their patients. This reflects the willingness to provide quality care to patients with the utmost dedication that can be augmented by taking care of the physical and emotional needs of our health workers. Various strategies at the workplace which have helped the health workers in coping with the current situation include the use of telemedicine facility to enquire about the problems of patients and measures to enforce social distancing in the wards and outpatient departments. Keeping the health workers updated about the recent developments helps to negate the uncertainty and emotional challenges associated with the disease.[16] Peer support, regular communication with friends, and family helps to alleviate the anxiety associated with the current crisis situation.[17] Meditation, music, exercises, and prayers are other coping methods that one may use to tide over during this period. More than two-thirds of our study participants felt that their current quality of life as stressful as compared to pre-COVID times. Various studies have reported a high prevalence of depression and anxiety among HCPs during this time and are found to be prone to burnout mental exhaustion and suffer from insomnia.[181920] Chen et al. worked on a three-step approach to describe the psychological needs of their staff, which included the development of an interventional team for designing online materials, the use of teleconsultation for counseling, and the development of group activities to reduce stress. However, this initiative was met with diffidence from the participants themselves. Hence, after discussion with them, it was restructured to include basic requirements such as food, provision of the rest area, education on the care of COVID-19 patients, leisure activities, etc. This resulted in considerable satisfaction among the HCPs and highlights the need for repeated feedback and modification of such programs.[21] Liu et al. found that psychologists should work closely with those engaged in critical care activities, to minimize their stress levels and decrease the likelihood of developing depression, while Kang et al. noted the impact of teleconsultation services and counseling to address the emotional aspect of health workers.[2223]
To preserve the mental and physical well being of our health care workers, it is time to execute an accessible counseling service along with the need of a platform where they can vocalize their concerns without any fear of hostile consequences. Health-care workers may ask whether their family members can receive priority for testing and treatment for this disease. Ensuring the care of health-care workers' family members would enhance workforce confidence and availability.
CONCLUSION
These are extraordinary times. Collaboration between all health workers, meticulously designed work environment, clarity in guidelines to treat patients based on evidence, effective leadership is essential to containing this outbreak. Adequate provision of PPEs and training of HCPs should be mandatory in safeguarding and preserving our workforce. Implementation of productive strategies will go a long way in protecting our frontline army in this battle against such a fatal disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Coronavirus Disease (COVID-19) Situation Reports. Available from: https://wwwwhoint/emergencies/diseases/novel-cor onavirus-2019
- Novel Coronavirus Disease 2019 (COVID-19) Pandemic: Increased Transmission in the EU/EEA and the UK–Sixth Update. Stockholm, Sweden: European Centre for Disease Prevention and Control; 2020.
- Interim Infection Prevention and Control Recommendations for Patients with Confirmed Coronavirus Disease 2019 (COVID-19) or Persons under Investigation for COVID-19 in Healthcare Settings. Available from: https://wwwcdc gov/coronavirus/2019-ncov/hcp/infection-control-recommendations html
- Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123-7.
- [Google Scholar]
- The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168:1245-51.
- [Google Scholar]
- Supporting the Health Care Workforce During the COVID-19 Global Epidemic. JAMA. 2020;323:1439-40.
- [Google Scholar]
- Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-9.
- [Google Scholar]
- Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083.
- [Google Scholar]
- Straining at work and its relationship with personality profiles and individual consequences in healthcare workers (HCWs) Int J Environ Res Public Health. 2020;17:610.
- [Google Scholar]
- Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049-55.
- [Google Scholar]
- China's Doctors, Fighting the Coronavirus, Beg for Masks. 2020. New York Times. Available from: https://wwwnytimescom/2020/02/14/world/asia/china-coronavirus-doctorshtm
- [Google Scholar]
- Infection Prevention and Control during Health Care when COVID-19 is Suspected: Interim Guidance 19 March 2020. Geneva, Switzerland: World Health Organization; 2020.
- Do theatre staff use face masks in accordance with the manufacturers' guidelines of use? J Infect Prev. 2019;20:99-106.
- [Google Scholar]
- Personal protective equipment and Covid 19- a risk to healthcare staff? Br J Oral Maxillofac Surg. 2020;58:500-2.
- [Google Scholar]
- 2020. Coronavirus Disease 2019 (COVID-19): Interim US guidance for risk assessment and public health management of persons with potential Coronavirus Disease 2019 (COVID-19) exposures: geographic risk and contacts of laboratory-confirmed cases Centers for Disease Control and Prevention. https://wwwcdcgov/coronavirus/2019-ncov/php/risk-assessmenthtml
- The impact of COVID-19 epidemic declaration on psychological consequences: A study on active Weibo users. Int J Environ Res Public Health. 2020;17:2032.
- [Google Scholar]
- COVID-19: Peer Support and Crisis Communication Strategies to Promote Institutional Resilience. Ann Intern Med 2020:M20-1236. doi:107326/M20-1236 Epub ahead of print
- [Google Scholar]
- COVID-19 pandemic: Stress experience of healthcare workers – A short current review. Psychiatr Prax. 2020;47:190-7.
- [Google Scholar]
- Psychological status of surgical staff during the COVID-19 outbreak. Psychiatry Res. 2020;288:112955.
- [Google Scholar]
- Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun 2020 May 8:S0889. doi: 10.1016/j.bbi.2020.05.026. Epub ahead of print
- [Google Scholar]
- Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15-6.
- [Google Scholar]
- Critical care response to a hospital outbreak of the 2019-nCoV infection in Shenzhen, China. Crit Care. 2020;24:56.
- [Google Scholar]
- The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7:e14.
- [Google Scholar]






