Translate this page into:
Development and Progress of a Collaborative Learning Model for Quality Improvement in the Field of Palliative Care in India

*Corresponding author: Dr. Nandini Vallath, National Cancer Grid, Tata Memorial Hospital, Dr. Ernest Borges Road, Parel East, Parel, Mumbai - 400 012, Maharashtra, India. aanandini@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vallath N, De Natale M, Lorenz KA, Bhatnagar S, Mickelsen J. Development and progress of a collaborative learning model for quality improvement in the field of palliative care in India. Indian J Palliat Care 2021;27(2):189-96.
Abstract
Quality is central to healthcare and even more so in the field of palliative care. Palliative care approach is centered around discovering facets of care crucial to improving the quality of life of the patient; be it symptom control, emotional concerns, impact on social roles or reviving the sense of spiritual connectedness. Although there are essential and desirable standards for quality of services, the journey taken by a service, toward quality improvement (QI), is often complex and uncharted. It is up to individual service units to strive toward improvement and reach higher levels of quality. Evidence suggests using a structured methodology for successful improvement in healthcare quality, as most problems are complex and multifaceted. This article introduces the concept and application of QI methodology in the field of palliative care in India and provides an overview of the first cohort of QI projects, facilitated through an international collaborative. The sequence of training, the tools, and the key ingredients for success are enumerated.
Keywords
Collaborative
Improvement
Methodology
Palliative care
Quality
Training
INTRODUCTION
Quality is central to healthcare. Every step in the progress of healthcare sciences may be attributed to a quest for quality, be it advent of disinfection, antibiotics, or chemotherapy, discovery of anesthesia, or emergence of new specialties. Care when it is of high quality fulfills the healthcare professional with a sense of purpose, and the care that is perceived as of high quality by the patient/ family influences therapeutic relationships positively and eventually impacts the outcomes.
Palliative care is innately quality conscious. Palliative care approach is centered around discovering facets of care crucial to improving the quality of life of the patient; be it symptom control, emotional concerns, impact on social roles or reviving the sense of spiritual connectedness. In fact, the emergence in the field of palliative care may be considered as an outcome of a quest for improvement in the quality of healthcare.
Key values evidenced as essential for improved quality of healthcare are safety, effectiveness, and efficiency of care processes; care that is equitable and timely; and care that enhances patient or staff experiences. Table 1 lists core principles of palliative care aligned with the key values included in the healthcare improvement.
| • Safety: Ethical and proportionate care, communications, coordination across care settings |
| • Efficiency: Care at physical/emotional/social/spiritual realms, continuum of care |
| • Effectiveness: Empowered autonomy, symptom relief, quality of life, and death |
| • Equitable: Nonabandonment, care inputs across trajectories/diagnosis/age |
| • Timeliness: Patient/family education on care, anticipatory care, simultaneous care with disease management |
| • Experience: Patient prioritized care, transitions in goals of care, shared decision making, ingrained with dignity and respect |
The audit tool of the Indian Association of Palliative Care lists the standards for palliative care services in India. This allows self-assessment of services as per the national norms.[1] The tool features service standards as “essential” and “desirable” components. The examples of essential standards are a trained multidisciplinary team working together through a structured process for whole patient care, through methodical assessment, documentation, and management protocols, and with access to essential medicines. The services achieve desirable standards when they include ethical framework in care decisions, collaborative activities with the community, and professional development programs.
This journey toward quality improvement (QI) is often complex and uncharted, as it is up to the service units to strive toward improvement and reach higher standards. When faced with a quality-related problem, teams conventionally tend to notice the most/superficial aspect of the problem and reach for solutions from that narrow scope. For example, when a homecare team is “dissatisfied with the quality of care” they provide, the discussions and solutions considered for improvement would often be around shortage of staff, need for recruitment, accessing funds and expansion of the team, or/and acquiring a new vehicle for better coverage. In case there is a brainstorming session, it may not necessarily involve the personnel on the ground – which in this case may be the field-based staff nurse, the driver, the community volunteer, and the home-care coordinators – who are directly involved with the problem. The discussion on the “dissatisfaction with quality of care” may have missed several significant contributors, and the teams continue to be perplexed with the lack of improvement even after investing and employing “the solutions.”
Evidence suggests using a structured methodology for successful improvement in healthcare quality,[2] as most problems are complex and multifaceted. The QI methodology helps analyse the problem, surface crucial contributors and guides the team along the improvement pathway as they test interventions and observe for the impact of each. The team is enabled to act based on the emergent root causes but not on the team leader’s perspectives or “gut feeling.”
By 2017, several palliative care units in India which had matured over previous decades were ready for their improvement journey toward becoming centers of excellence. Accordingly, the palliative care community from the National Cancer Grid approached the QI Hub leaders at Stanford Medicine to initiate a collaborative experiential training in QI. By October 2017–2018, Stanford Medicine (United States) partnered with Indian palliative care leadership through an international collaborative to facilitate the first cohort for training in QI. The core QI leadership team consisted of a certified QI trainer, a director of training programs, and a palliative care professional from Stanford Hub. In addition, volunteer mentors from seven global universities engaged one on one with the seven palliative care clinical team leaders from India. The Palliative Care-Promoting Assessment and Improvement of Cancer Experience (PC-PAICE) program, that combined Stanford’s in-house curriculum, the Clinical Effectiveness Leadership Training program with mentored experience, was employed for training and implementing the QI projects of this cohort.
MATERIALS AND METHODS
The Kolb model emphasizes experiential learning, where the learning, change, and growth are accomplished as the learners apply newly learned skills, in their work, reflect on the impact, and modify their approach accordingly.[3] An iterative approach to learning, not unlike the Kolb model, served as the main approach for the clinical teams involved with the PAICE program. To facilitate this, the A3 methodology for improvement was selected and adopted.
QI methodology is an evidence-based science that assists teams to think through problems comprehensively and activate consensus while working through both the problem and the solutions. The A3 method provides a Plan-Do-Study-Act (PDSA) cycle, which is repeated cyclically to refine the solutions as the team tests process changes [Figure 1]. The PC-PAICE curriculum is Table 2 allowed each participating team to go through at least one cycle of the PDSA exercise relevant to their quality problem.

- A3 Tool used for the Palliative Care-Promoting Assessment and Improvement of Cancer Experience Training for cohort 2017–2018.
| Month and theme | Contents and activities |
|---|---|
| Problem statement and background | Encourages stating of the problem clearly without biases or foreseen solutions Explain why it is important, and how it aligns with the vision of the department or the institution and document it concisely |
| SMART goal | The team contemplates on what would be target state once the problem situation improves. This goal is stated in a SMART-bound manner |
| Process map | Engages the team to delineate the status of processes around the selected problem. This is done through a visit and mindful walk across the different components of the process within the setting |
| Run chart of the specific measure | The team selects a measure that reflects the outcome requiring change; notes its baseline status, and maintains record at regular intervals(daily, weekly, biweekly). The chart indicates in real time if the project is moving in the intended direction |
| Root-cause analysis | These are very specific tools- the cause-effect diagram and Pareto chart which helps to consensually elicit, document, and analyze all possible contributors to the problem to get to the most vital contributors |
| Key drivers | Key drivers are subgoals, which are important to the success of the project that emerges from root-cause analysis |
| Interventions | At this stage, the interventions/countermeasures to support each identified key driver are considered, iteratively developed, evaluated, refined, and implemented |
| Maturity, reliability, and sustenance plans | The most valuable interventions are selected based on their impact on the run chart of outcome measure and earmarked for wider implementation. Care is taken at this stage to help sustenance of the improvement through in-built process changes |
| QI cycle | The above components form the PDSA cycle The team can choose to go through the cycle repeatedly to further fine-tune the improvements achieved |
SMART: Specific, Measurable, Achievable, Realistic and Time-bound, QI: Quality improvement, PDSA: Plan-Do-Study-Act
The A3 methodology includes specific tools to assist with problem-solving. The principal tool is the 11’’ × 17’’ project progress tracker, commonly called the A3. The A3 was developed at Toyota Motor Corporation[4] and adapted for healthcare quality at Stanford.[5] The tool guides the flow of the project, as the teams study and reflect on their problem sequentially across the sections of the improvement tool, mandated from the left upper quadrant to the right lower quadrant of the A3. This assists methodical and deeper analysis of the problem using the specific improvement tools.
The sequential learning schedule for the 2017 cohort is listed in Table 2.
The A3 tool begins by stating the specific problem as relevant to the background of the institution and selecting the goals (e.g. Specific, Measurable, Achievable, Realistic and Time-bound (SMART) goals) that would reflect the improvement envisaged. The run chart using the chosen project measures tracks the project progress. Moreover, the process map tool helps identify the main sequential steps in the current scenario. The detailed mapping opens up the scope for reflections and improvements. The cause-and-effect tool activated at this stage helps identify all the contributors to the problem under six or more main domains. Next, the Pareto chart is used to categorize the list of contributors into the vital few root causes. The project is now ready to derive the key drivers that help reorient the processes and evolve specific tests of change to execute. The continuous charting of the identified outcome measure depicts the ongoing change as the different interventions are employed. The team thus gets continuous visual feedback on the impact of interventions on the improvement process.
The learning schedule and the assignments were crucial to conceptual clarification. During the project period, participants met virtually once every month, when each section of the A3 would be elaborated through a didactic, followed by presentations of QI projects by the site teams. The teams were also encouraged to engage and provide feedback to other projects during the virtual course sessions. Each team met together and collaborated with their assigned mentor through e-mails and through virtual meetings across the duration of the project to complete the mandated interim assignments and uploaded it on the interactive platform provided by the Stanford Hub. The electronic copy of the A3 made it convenient for the participants to update, share, comment, and review their efforts as mutually decided with the mentors.
RESULTS
The improvements achieved by projects from cohort 1 are depicted in Table 3. Figure 2 shows the run charts of four of the team projects from the 2017–2018 QI cohort. The primary objective, of improving or resolving the identified quality problem, was achieved during the project period, by all the teams in the first cohort. For example, one project tripled their home visit capacity over the timeframe of the training from an average of two home visits per week to seven home visits per week. Another project decreased the delay in referral of advanced oral cancer patients to specialist palliative care, from an average of 50 to 14 days. The team that was dissatisfied with the quality of care provided to their home-care patients, improved their satisfaction score significantly, and achieved their target level. Finally, a team that improved the documentation of prognostication conversations with patients/families increased it from 0% of adequate documentation to over 75% during the course.
| Palliative care centers in India | The overall project results |
|---|---|
| Department of Palliative Medicine- All India Institute of Medical Sciences, NewDelhi | Reduced the delay for referring advanced cancer patients to palliative care, from 50 days to 14 days |
| Trivandrum Institute Palliative Sciences, Thiruvananthapuram | Improved provider satisfaction on quality of care from baseline of 5.82/10 to 7.3/10(here 0 indicated no satisfaction at all, and 10 indicated maximum satisfaction with the quality of care provided to home-care patients) |
| Department of Palliative Medicine- Homi Bhabha Cancer Hospital and Research Centre, Visakhapatnam | Improved home visit volume from 2 to 8 per week |
| Department of Palliative Medicine- MNJ Institute of Oncology, Hyderabad | Improved provider confidence level for care coordination 1.5-6.0 (1-10 scale) |
| Department of Palliative Medicine- Tata Memorial Hospital, Mumbai | Improved appropriate referral rate to palliative care from 50% to 75% |
| Thrissur Institute of Palliative Care, Thrissur | Improved documentation of communication on prognosis from 0% to 75% |
| Cipla Palliative care Centre, Pune | Improved consistency of early referrals from 0% to 80% |
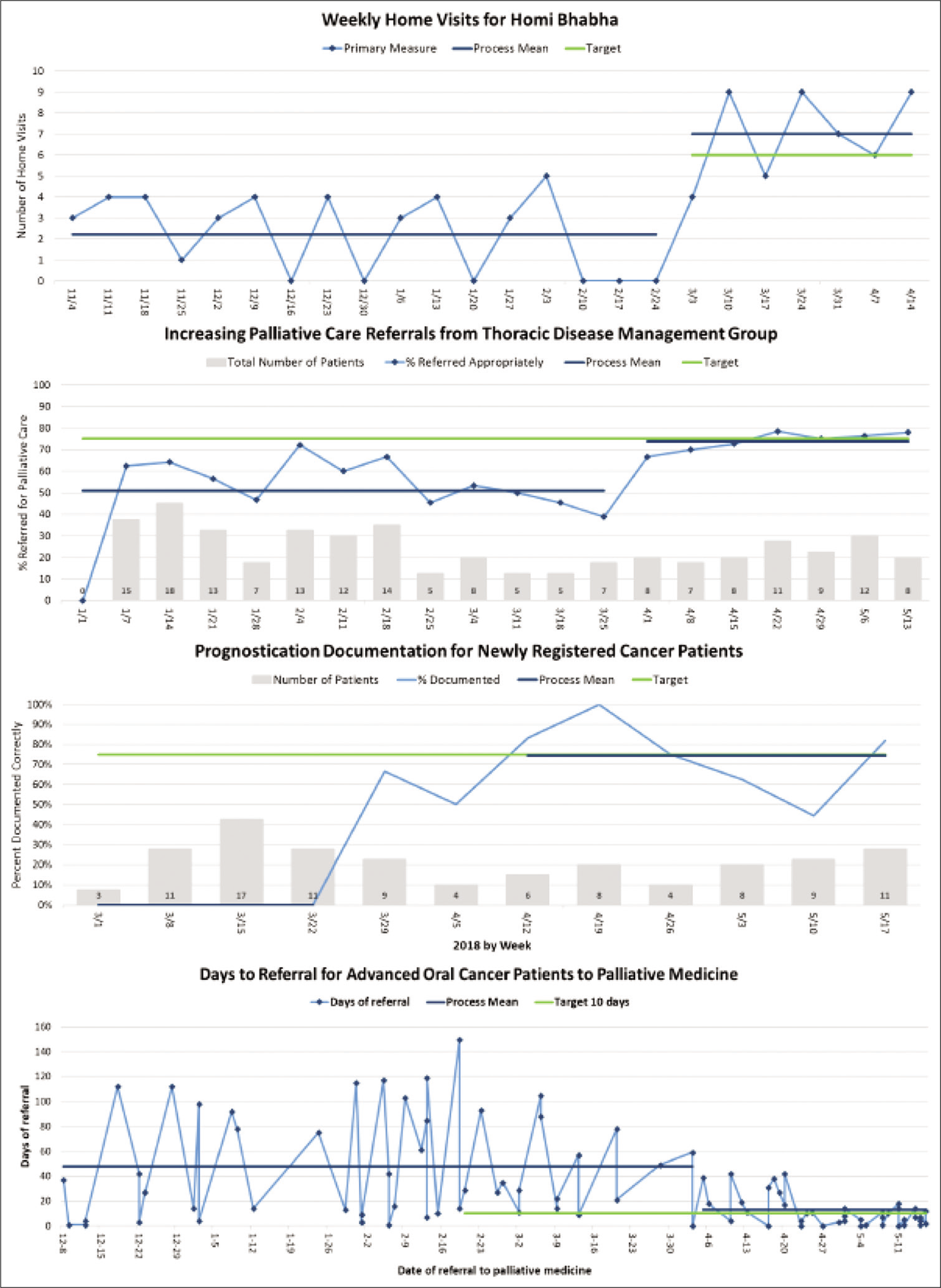
- Run charts showing four of the seven 2017–2018 project results. Each showing significant measurable improvement in their chosen project measure.
In addition, the coordinating Hub team, maintained a monthly record of the project progress of each team. The score legend and the progress, by the end of the project time, are depicted in Figure 4. Figure 4 shows the progress scores of the seven projects. The articles that follow this section contain a detailed step-by-step description of the individual improvement projects of the cohort 2017–2018.
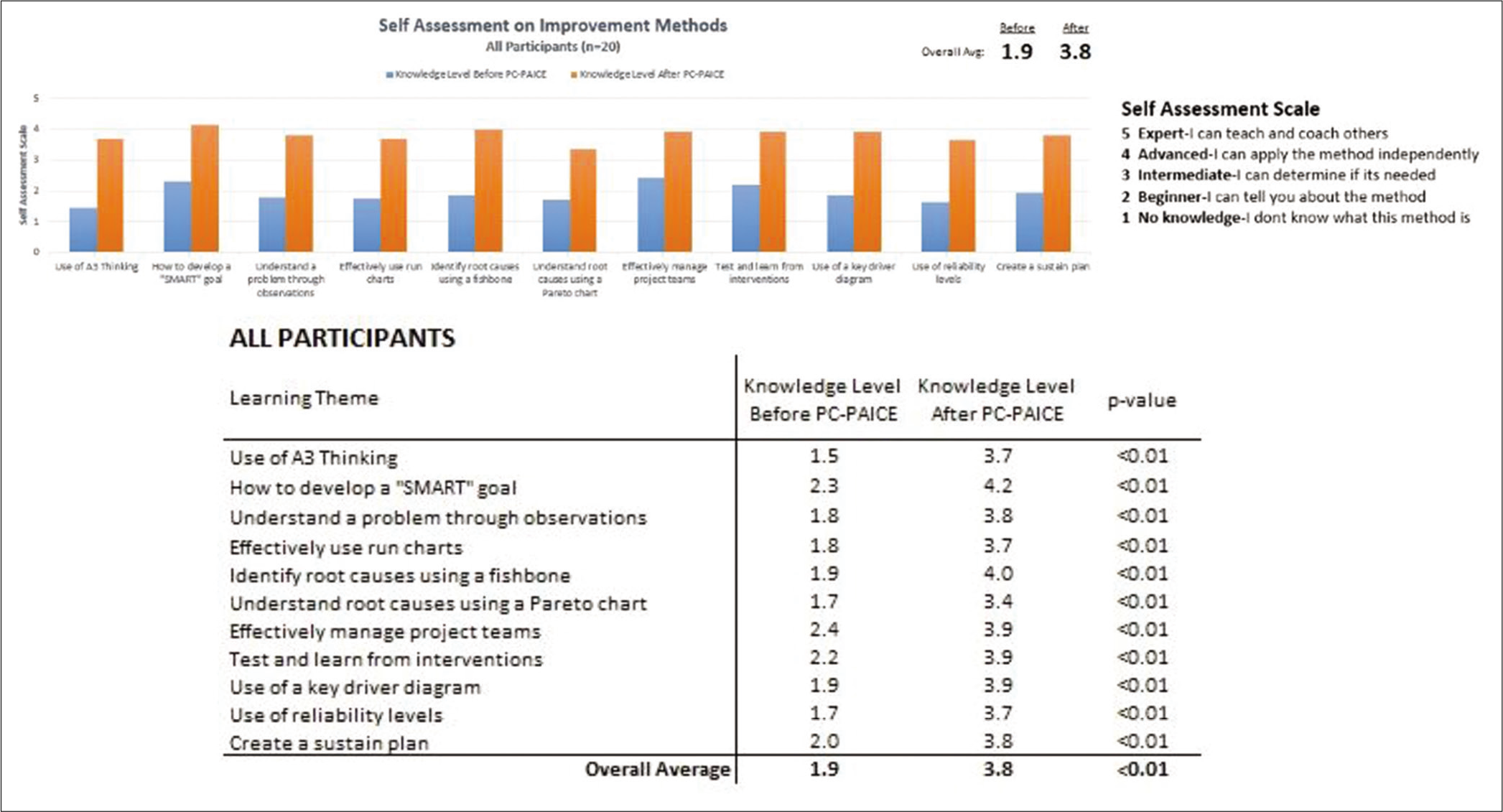
- Improvement in self-reported learner capacity to use improvement methodology during 2017–2018 training.

- Project Progress Scores 2017–2018 cohort.
A self-assessment survey was distributed to all participants following the training program to measure the increase in knowledge and capability. Participants demonstrated a higher level of knowledge and confidence in applying improvement science to their local settings. The assessment showed an increase of capability to utilize the improvement methods from an average of 1.9 (beginner: I can tell you about the method) to 3.8 (advanced: I can apply the method independently).
Comments from participants on completing the improvement training reflected the qualitative impact of the program. For example, “I learnt the importance of quality in daily practice. Realized that when routine work is checked/analysed, there is scope for improvement at multiple domains. Once root causes are correctly identified, and interventions designed to improve quality, it actually saves time and efforts for both patients and clinicians,” commented one team leader. The insight on structured approach was reflected in the following comment, “I have always thought here is a problem, this is the solution and jumped right into it. PAICE helped approach solution in a more open-minded approach through specific steps and logic.”
The participants also commented on the helpfulness of the resources toward the training in QI. Online improvement videos were rated as the least helpful, while the A3 problem-solving tools and monthly virtual learning sessions and discussions with mentors were rated as most essential to the success of the program. Figure 3 depicts the rise in the capacity to use improvement methodology as self-assessed by the team members.
DISCUSSION
The team-based, project-based, methodology-based immersion training in QI achieved significant success in three major areas; (i) in addressing the quality problem identified by the team and achieving significant, measurable, improvement with a level of reliability and with plans for sustainability; (ii) in increasing the knowledge and skills of QI team leaders in applying evidence-based QI methods in the clinical and operational setting; and (iii) in building capacity of a team within the host institution, which is oriented to approaching quality concerns and its improvement in a methodical manner, and who can catalyze QI culture changes for the institutions in the future.
The team experienced major attitudinal leaps regarding problem-solving at two specific stages along the methodology; (i) root–cause analysis of the problem to derive key drivers – the hierarchy that governs hospital environment was impacted and physicians learned some incredible contributors to the problem/ solutions from the ground staff, whose voice would otherwise have remained unheard; (ii) analysis and implications of the Pareto principle, i.e. 20% of the contributors cause 80% of the problem. These qualitative results are indeed difficult to express as significant using conventional publication models available.
Overall, the teams enjoyed the experience of attaining a major improvement through teamwork focused to modify just a few of the listed contributors. Access to a steady reliable mechanism for effective organizational change, and initiating an organizational culture of constructive problem-solving, inclusive of all stakeholders, has been valued.
Detailed reflection of the PC-PAICE 2017–2018 identified seven key ingredients that contributed to its import. They are listed in Table 4.
| Key element | Remarks |
|---|---|
| Selection of team leaders to represent both the administrative and clinical perspectives | This bridged the gaps in communications and sanctions required by the frontline staff from the institutional management |
| Empowering frontline staff members in each setting during the entire change process | Provides a sense of ownership of the processes, during the project and after its completion. Ensures the challenges are accurately represented, and improvements are sustained |
| Designation of the training program coordinator director who orchestrated the training and schedules monitored the project progress | Communications that clarified the agenda before and summary of meetings after. Clear instructions on assignments the projects should be working on during the interim periods between learning sessions |
| QI teams required to enroll the support of managers/ heads of department and other staff by demonstrating the relevance and criticality in solving the identified problem | The problem and the interventions emerged with consensus. The coordination and communications became simpler as the ownership was shared, and the changes are not felt as imposed |
| Mentors assigned to each team to assist with approaching the problem and applying suitable tools | The mentors did not directly solve the problem. Their expertise was in guiding teams to approach each step with an open mindset and developing the solutions consensually |
| Assignments on each problem-solving tool and sharing of progress through a common platform | The key concepts on methodology got reinforced through the assignments that followed |
| Simultaneous work with multiple project teams | Participants were able to learn from each other by listening to the shared challenges and progress of each other. The teams were encouraged through the healthy peer to peer accountability that helped drive them forward |
QI: Quality improvement
The smooth flow of the QI training program and the impact that was achieved must be attributed to the encouragement and generosity of the spirit of the Stanford Hub members, who gladly shared their years of QI coaching experiences with different cohorts from various backgrounds.
An India-based QI Hub was launched in October 2018 as a direct outcome of the enthusiasm shared by the first cohort participants to organize themselves and access funds to initiate this. The QI Hub has gone on to develop in-house training capacity contextual to India. The QI-Hub-India continues to collaborate with the Stanford team while developing it’s in-house training capacity. A total of 30 teams comprising of 60 professionals from across India, have become certified quality improvement leaders, capable of enhancing the safety and quality of patient care. This period was used to build the mentorship capacity of India, by pairing interested alumni of the first cohort, with international QI mentors engaged with this project. Subsequently, the QI-Hub India successfully conducted the “Enable Quality, Improve Patient Care -“EQuIP-India” program for the 2019–2020 cohort with content and contextual modifications to the PC-PAICE, making it suitable for Indian healthcare settings. The most recent cohort included oncology teams as well. The processes at the QI-Hub India across the two cohorts since 2018 are being monitored, and the analysis will provide the required evidence to improve the effectiveness of its structure, processes, and organizational capacity and its relevance in the future of cancer-related care in India.
CONCLUSION
Highly contextual capacity building in crucial realms such as quality improvement can be achieved through international collaboration models that are aligned with the regional healthcare culture and needs.
Acknowledgments
We are grateful to all our international mentors - Michael Rabow - University of California, San Francisco; Stephanie Harman, and Sridhar Seshadri - Stanford Medicine; Jane Philips and Meera Agar, MBBS - University of Technology, Sydney; David Casarett - Duke University; Sydney Dy - Johns Hopkins Medicine; Odette Spruijt - Peter Mac Callum Cancer Centre and Karen Anderson - Edith Cowan University, Australia, for their commitment and support in developing the QI training program in India.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Creation of minimum standard tool for palliative care in India and self-evaluation of palliative care programs using it. Indian J Palliat Care. 2014;20:201.
- [CrossRef] [Google Scholar]
- A framework for healthcare quality improvement in India: The time is here and now! Postgrad Med. 2011;57:237-41.
- [Google Scholar]
- Toward an applied theory of experiential learning In: Cooper C, ed. Studies of Group Process. London, England: Wiley; 1975. p. :31-57.
- [Google Scholar]
- Principle 7: Use Visual Control So No Problems Are Hidden, in New York, McGraw-Hill Education. 2004. Available from: https://www.accessengineeringlibrary.com/content/book/9780071392310/chapter/chapter13 [Last accessed on the 2021 Aug 03]
- [Google Scholar]
- Realizing improvement through team empowerment (RITE): A team-based, project-based multidisciplinary improvement program. Radiographics. 2016;36:2170-83.
- [CrossRef] [Google Scholar]






