Translate this page into:
Effect of Mindfulness-Based Art Therapy (MBAT) on Psychological Distress and Spiritual Wellbeing in Breast Cancer Patients Undergoing Chemotherapy
*Corresponding author: Anjali Mangesh Joshi, Department of Psycho-Oncology, HCG NCHRI Cancer Centre, Nagpur, Maharashtra, India. dranjali145@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Joshi AM, Mehta SA, Pande N, Mehta AO, Randhe KS. Effect of mindfulness-based art therapy (MBAT) on psychological distress and spiritual wellbeing in breast cancer patients undergoing chemotherapy. Indian J Palliat Care 2021;27:552-60.
Abstract
Objectives:
Psychological distress and spiritual well-being (SWB) are directly related to the quality of life in cancer patients. Mindfulness-Based Art Therapy (MBAT) integrates mindfulness practices with art therapy and has shown to decrease distress levels and improve SWB in women with breast cancer. The objective of the study was to identify the effects of a 1-week MBAT intervention on psychological distress and SWB in breast cancer patients undergoing chemotherapy.
Materials and Methods:
This was a single group, pre-test post-test study carried out in a clinical setting. The psycho-oncology assessment questionnaire, Distress Thermometer (DT) and Functional Assessment of Chronic Illness Therapy-SWB Scale 12 (FACIT-SP12) Version 4 were administered before, post1st supervised MBAT session and post 1 week of home practice to breast cancer patients undergoing chemotherapy (n = 30). The MBAT intervention included mindfulness meditation for 15 min and mindful coloring for 30 min daily for 1 week. Data analysis was done using R i386 4.0.3.
Results:
The median DT score significantly decreased from pre-session to immediate post-session and pre-session to post 1-week session. The median of meaning, peace, and faith subscales of FACIT SP12 scores along with total FACIT SP12 score significantly increased from pre-session to immediate post-session as well as from pre-session to post 1 week.
Conclusion:
One-week MBAT intervention for breast cancer patients undergoing chemotherapy significantly decreased the psychological distress and significantly improved the SWB in terms of meaning, peace, and faith.
Keywords
Mindfulness
Art therapy
Breast cancer
Spiritual wellbeing
Psychological distress
INTRODUCTION
Psychological distress, anxiety, and depression are commonly seen in cancer patients receiving chemotherapy.[1] It is necessary to identify high-risk patients through psychosocial screening to provide early intervention. Failure to detect and treat psychological distress affects the outcomes of cancer therapies and decreases patients’ quality of life (QoL).[2] Spiritual well-being (SWB) is a feeling of contentment that arises from the inner self and is directly related to the QoL in terms of meaning and peace in cancer patients.[3]
Originated from Buddhist meditation practices, mindfulness is “the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment to moment.”[4] Mindfulness-based interventions are found to be effective in reducing psychological distress and other symptoms in cancer patients.[5] They have shown significant improvements in existential well-being, the number of self-identified losses, grief scores, as well as mental adjustment styles in breast cancer patients.[6] Enhanced mindfulness is shown to partly mediate the association between increased daily spiritual experiences and improved mental health-related QoL. Changes in spirituality and mindfulness were shown to be significantly associated with improvement in mental health.[7]
There is a growing body of research supporting the potential of art therapy in reducing emotional distress, depression, anxiety, and pain in cancer patients undergoing chemotherapy.[8] The interrelatedness of art therapy and mindfulness can provide a wide range of opportunities for application with diverse populations.[9] Mindfulness-based art therapy (MBAT) is a relatively novel concept introduced by psychologist and writer Laury Rappaport.[10] MBAT combines the philosophy and practice of mindfulness with art therapy. In this, a person engages in the creative process of art as a way of self-exploration in a mindful way. This includes the core components of mindfulness with guided meditations and sensitive exploration of the art creation. The art-making practice is performed with kindness, curiosity, compassion, acceptance, non-judgmental responses, and awareness of the present moment.
Although there is little scientific evidence of MBAT as an intervention, it is slowly gaining recognition as a tool for improving psychosocial health. MBAT benefits include relief from anxiety, depression, fatigue, improvement in physical functioning,[11] psychological state, SWB, mindfulness,[12] and QoL.[11,12]
Since in mindfulness and art-making, there is awareness away from the habitual thinking mind, toward heightened feeling and sense, it is suggested that both these processes promote the activation of the parasympathetic nervous system.[13] This induces a relaxation response and reduces psychological distress. During the MBAT sessions, the patients learn to reconstruct meanings, minimizing over identification with illness, and negotiate experiences and life events on their terms. These factors can help in improving SWB.[14]
The present study was undertaken to evaluate the effects of a 1-week MBAT program on the following parameters in breast cancer patients undergoing chemotherapy.
Psychological Distress measured by Distress Thermometer (DT)
SWB measured by The Functional Assessment of Chronic Illness Therapy-SWB Scale (FACIT SP12) Version 4
MATERIALS AND METHODS
This was a single-group, pre-test post-test study carried out in a clinical setting. The study period was from December 2020 to February 2021. The institutional ethics committee approval was obtained before starting the study. A convenience sample collection method was used for recruiting the study participants. Patients diagnosed with breast cancer and undergoing chemotherapy at a cancer hospital in Nagpur, Maharashtra, India, were recruited for the study.
Estimation of the sample size
Sample size calculation tool on https://sample-size.net/sample-size-study-paired-t-test/ was used.
N = Sample size/Group size
Z α/2 is the standard normal z-value for a significance level α = 0.05, which is 1.96.
β is the standard normal z-value for the power of 80%, which is 0.84.
Based on the reference study, the pre-test and post-test mean difference of psychological domain scores was 2.82.[15]
Effect size (E) = 2.82, SΔ is the standard deviation of the change in outcome= 5.5
B = (Z α/2+ Zβ)2=7.8489.
C = (E/SΔ)2=0.2629.
N = B/C =29.8562 = 30
The required sample size was estimated as 30. By assuming 5% lost to follow-up, the updated sample size was 32 [Figure 1].
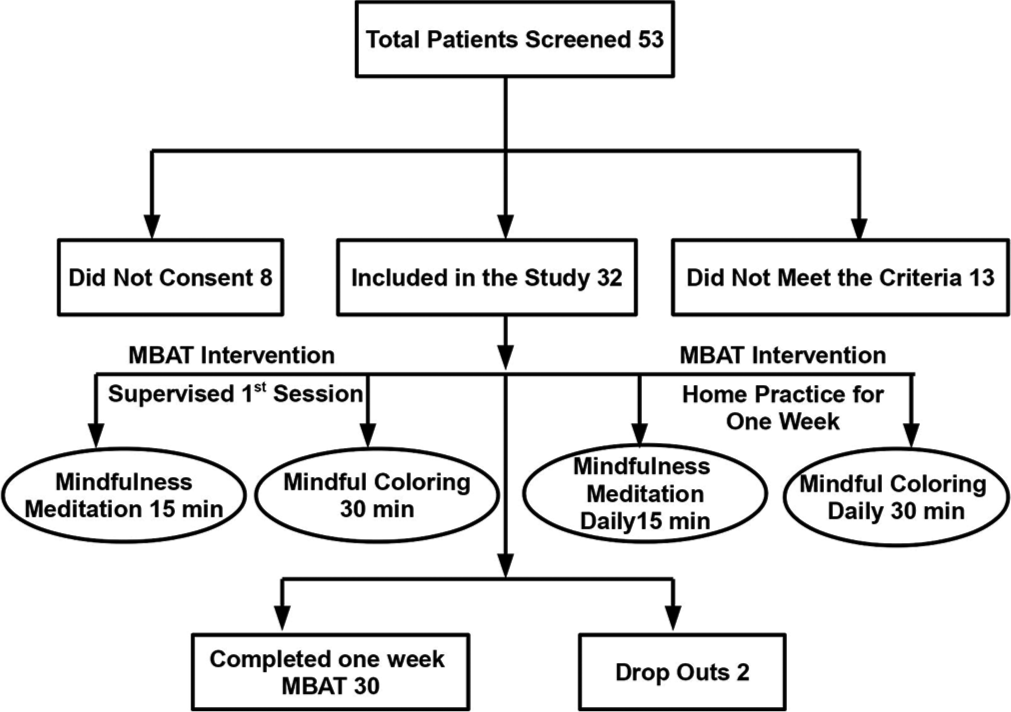
- Methodology.
The total number of patients screened was 53. Of these, 32 were included in the study, eight patients did not consent to participate in the study, while 13 patients did not meet the inclusion criteria [Figure 1]. The reasons for not consenting to participate in the study were time constraints (n = 3), presence of lymphedema with associated pain in the arm (n = 2), not interested in art (n = 2), and vision-related problems (n = 1). Out of the 32 enrolled patients, 30 completed the 1-week MBAT intervention while two patients dropped out. The reason for dropout was the deterioration of health because of chemotherapy and associated side effects (n = 2).
The inclusion and exclusion criteria for patient recruitment are shown in [Table 1]. A detailed evaluation of patients’ condition before enrolling them in the study was made by the medical oncologist, who was a part of the research team. The presence of any cognitive impairment or neurological disease was evaluated through detailed case history, required investigations, and mentioned in the medical records of the patient. As a regular standard protocol, all patients are assessed and evaluated by the psycho-oncologist while noting down past and present history of any psychological/ psychiatric illness.
| Inclusion criteria | Exclusion Criteria |
|---|---|
| Breast cancer patients receiving chemotherapy | Extreme mobility problems or cognitive impairments |
| Age 20 and 70 years | A major psychiatric or neurological illness |
| Functional ability as per ECOG (Eastern Cooperative Oncology Group) score 0 to 1 | Any other co-morbid condition affecting the patients’ participation |
Data collection tools
The following questionnaires were used for collecting the data before starting the chemotherapy treatment, after 1st supervised MBAT session, and after 1 week of daily home practice. The patients’ responses were recorded by the interview technique by a clinical psychologist.
Psycho-oncology assessment questionnaire
This included the demographic information including age, marital status, education, occupation, detailed medical history, obstetric and gynecological history, plan of treating doctor, social and family details, lifestyle including diet, sleep, psychological details about mood, behavior, and thought process.
Distress Thermometer (DT)
The DT is a well-validated and reliable screening tool used in psycho-oncology research across the globe. It is recommended as a clinical tool to be used routinely in cancer settings.[16] It is a simple, pencil, and paper measure consisting of a 0-10 scale where zero point means “No distress” and point ten means “Extreme distress”. A score of four or above indicates that the distress needs intervention.
FACIT-SP12 version 4
The FACIT-Sp-12 has been translated and linguistically validated in 15 languages. It is being used in studies to evaluate the relationships between SWB, health, and adjustment to illness.[17] It is a 12-item questionnaire with subscales that measure faith, meaning, and peace, which are broadly consistent with conceptual models of SWB. It has a five-point Likert scale coded with the response categories “Not at all,” “A little bit,” “somewhat,” “Quite a bit,” and “Very much.” Permission to use the questionnaire was obtained through email. Validated questionnaires in Hindi and Marathi languages were used for the patients.
The MBAT intervention
MBAT intervention consisted of the first in-person supervised session conducted by the facilitators, followed by 1 week of daily guided home practice. The sessions were conducted by experts having training and experience in art therapy and mindfulness. The mindfulness sessions were conducted by the first author of this paper, a medical doctor, qualified yoga therapist with certification in Mindfulness-Based Stress Reduction program. She has 21 years of meditation practice experience and has been teaching yoga and meditation for 15 years. The psycho-oncologist and the co-author of this paper received training in “Expressive Arts Therapy Interventions for relieving emotional and physical suffering in cancer patients” in Banff, Canada, in 2019. It was a Pre-Congress workshop during the 21st World Congress of Psycho-Oncology, organized by the International Psycho-Oncology Society and Psycho-social academy. However, regarding art therapy intervention, the focus of our study was to add an element of mindfulness to the art activity.
The session was designed to suit the specific health conditions of the patients. Patients’ medical oncologist was consulted regarding the safety concerns and health conditions to participate in the study. Care was taken to protect vulnerable patients from potential risk factors. The following potential risk factors were considered while giving MBAT intervention.
Potential risk factors related to patient’s health
The medical oncologist was an integral part of the research team. Toxicity, chemotherapy-induced neutropenia, and side effects of chemotherapy such as nausea and vomiting were monitored and supervised. The participants enrolled in our study did not report any severe adverse effects of chemotherapy during the entire duration of MBAT intervention.
Since this study was carried out from December 2020 to February 2021 while COVID-19 pandemic was still going on, patients’ safety was given a priority. The COVID protocol was strictly adhered to. Group sessions were avoided and individual patient’s MBAT sessions were conducted.
Potential risk factors related to MBAT intervention
Although a growing body of research has documented the benefits of mindfulness-based practices, its potential adverse effects cannot be ruled out. A few studies have suggested that mindfulness may increase the awareness of difficult feelings, exacerbate psychological problems and can even lead to psychotic episodes.[18] It is believed that the occurrence of adverse effects can reflect pre-existing problems and/or unbalanced approaches to practice.[19]
Therefore, care was taken to exclude the vulnerable patients during the patient recruitment process. Clear instructions on how to practice the intervention were given to the patients. The intervention was simple, easy to understand and follow at home with the help of guided meditation audio in the local language.
Since no participants in the study had previous experience of mindfulness practice, the first session was supervised to monitor the patients’ responses to the mindfulness practice and to clear any doubts. Before the session, the details of the study were explained to the patients and their informed consent was obtained in writing. The responses of the patients were recorded on the questionnaires.
MBAT session
The intervention included didactic and experiential components of mindfulness meditation and mindful art.
Mindfulness meditation
The patients were briefed about the mindfulness practice and its core principles. The meditation included body scan, anchoring attention with the breath, and nonjudgmental awareness of physical sensations, thoughts, and emotions. The duration of meditation was 15 min.
Mindful art
This component of the intervention was focused on mindful coloring. Mindfulness-based coloring prints/sketches with 12 color pencils/crayons for coloring were used for art therapy. The coloring pages included abstract-style images, birds, animals, nature motifs, and mandalas (circular designs composed of symmetrical shapes). The mindful art session involved the mindful exploration of art materials with an awareness of sensory stimulus and response during coloring. The patients were encouraged to explore present moment experiences with kindness, curiosity, and non-judgment. An individual session for each patient was approximately 30 min duration.
After the session, the patients’ responses were recorded on the DT and FACIT-SP12 questionnaire. They were provided art materials and guided meditation audio in the facilitator’s voice for home practice. The participants continued the home practice for 1 week devoting at least 30 min to mindful coloring and 15 min to guided mindfulness meditation. The participants maintained a diary of daily MBAT practice. Daily telephonic follow-up of the participants was done by the cancer counselor and psychologist who was a member of the research team. Reminders to practice were given by telephone calls and text messages daily. After completion of 1 week, the responses were recorded on the DT and FACITSP12 questionnaire telephonically or in person.
Statistical analysis
Data analysis was done using R i386 4.0.3. Non-normal continuous data represented using median (1st Quartile, 3rd Quartile). Paired continuous data were compared using Quade test followed by Paired Wilcoxon test with “Bonferroni” adjustment as post-hoc. P < 0.05 was considered significant. A total of 30 patients were considered for the analysis. [Table 2] shows the demographic characteristics of the study population with reference to age, gender, diagnosis, co-morbidities and previous mindfulness practice. [Table 3] provides the summary of the data analysis.
| Demographic characteristics | Details | Number of patients out of 30 |
|---|---|---|
| Age in years | 25 to 30 | 1 |
| 30 to 40 | 7 | |
| 41 to 50 | 10 | |
| 51 to 60 | 10 | |
| 61 to 70 | 2 | |
| Gender | Female | 30 |
| Diagnosis | Ca breast | 28 |
| Ca breast with recurrence | 1 | |
| Ca breast with metastasis | 1 | |
| Co-morbidities | Not Significant | 19 |
| Hypertension | 8 | |
| Hypothyroidism | 3 | |
| Diabetes Mellitus | 6 | |
| Chronic Kidney Disease | 1 | |
| Previous mindfulness practice | No | 30 |
| Factor | Time point | Median (IQR) | Post hoc analysis | ||
|---|---|---|---|---|---|
| P-value | Pre versus post session | Pre versus post 1 week | |||
| Distress Thermometer score | Pre | 5 (5,6) | <0.0001 | <0.0001 | <0.0001 |
| Post | 4 (4,5) | ||||
| Post 1 week | 3 (3,4) | ||||
| Meaning Subscale of FACIT-SP12 | Pre | 11 (9,12) | <0.0001 | 0.001 | 0.006 |
| Post | 12 (9.75,13) | ||||
| Post 1 week | 13 (12,14) | ||||
| Peace Subscale of FACIT-SP12 | Pre | 10 (9,11) | <0.0001 | <0.0001 | <0.0001 |
| Post | 12 (11,14.25) | ||||
| Post 1 week | 15 (14,16) | ||||
| Faith Subscale of FACIT-SP12 | Pre | 12 (8,13) | <0.0001 | <0.0001 | <0.0001 |
| Post | 13 (12,15.25) | ||||
| Post 1 week | 15.5 (12.25,16) | ||||
| Total FACIT SP 12 | Pre | 31 (26.75,36) | <0.0001 | <0.0001 | <0.0001 |
| Post | 37 (31.5,41.25) | ||||
| Post 1 week | 43 (41,44) | ||||
FACIT-SP12: The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale, IQR: Interquartile range
RESULTS
The median DT score significantly decreased from pre-session to immediate post-session and pre-session to post 1-week session [Figure 2]. The median of total meaning, peace, and faith subscales of SWB score significantly increased from pre-session to immediate post-session as well as from pre-session to post 1 week [Figure 3]. The median of total SWB (FACIT SP12) score significantly increased from pre- to post-session and from pre to post 1 week [Figure 4].
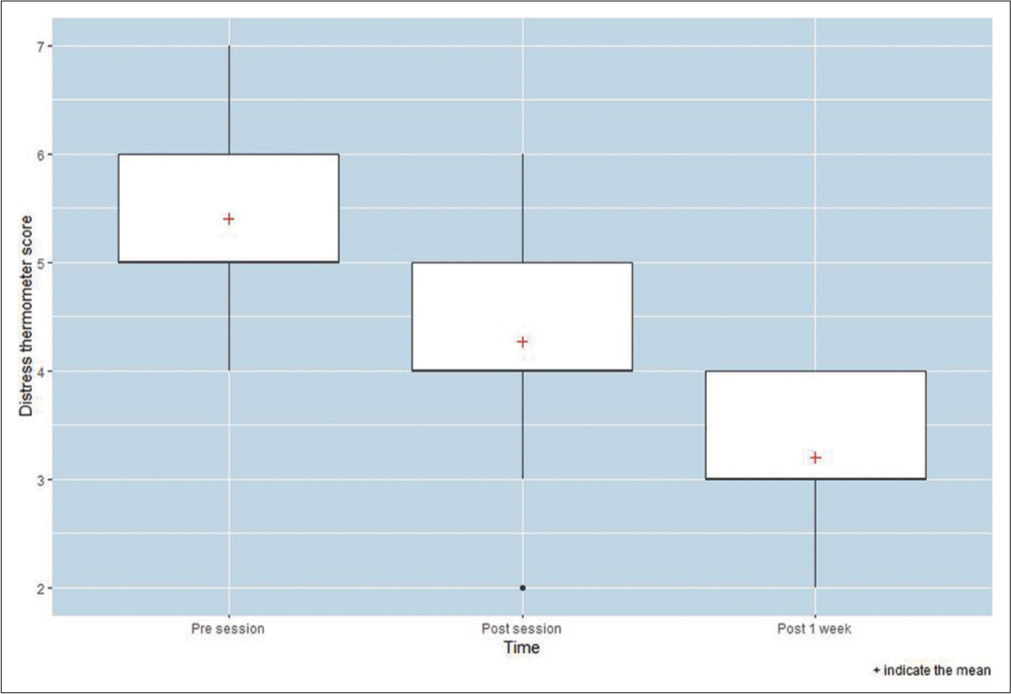
- Comparison of distress thermometer scores over time points.

- Comparison of subscale scores of Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-SP12) over time points.

- Comparison of Total Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-SP12) scores over time points.
DISCUSSION
In this study, we evaluated the effects of 1-week MBAT intervention on two parameters, psychological distress, and SWB in breast cancer patients undergoing chemotherapy.
Psychological distress
We observed a significant reduction in distress scores immediately after the first supervised session and after 1 week of daily home practice of MBAT intervention. The results of this study are in agreement with a study that has shown decreased distress levels and improved QoL in women with breast cancer after the MBAT intervention.[15] Another randomized, controlled investigation of MBAT reported a reduction in symptoms of distress and improvements in key aspects of QoL in women with cancer.[20]
Our results are consistent with a study that evaluated the impact of a coloring intervention on female adults’ psychological experiences. The participants experienced lower levels of depressive symptoms and anxiety following the intervention.[21,22]
In our study, we used mindful coloring as a form of art therapy. The therapeutic value of coloring was demonstrated in a study[22] that reported significantly lower levels of depressive symptoms and anxiety. It was suggested that daily coloring can improve some negative psychological outcomes and may provide an effective, inexpensive, and highly accessible self-help tool.[22] Mandala coloring paired with focused breathing was suggested as an effective technique for reducing self-reported negative affect and state anxiety.[23] A study[24] supported the hypothesis that coloring a mandala for 20 min was more effective at reducing anxiety than free-form coloring for 20 min. Another study[25] also concluded that coloring structured mandalas were associated with greater anxiety reduction than unstructured coloring.
SWB
In our study, significant improvements in peace, faith, and meaning sub-scales scores, as well as total SWB score, were observed. These results are consistent with a study[14] where 8 weeks of MBAT intervention was found to have significant improvement in peace, faith, and meaning sub-scales of SWB and improvement in emotional well-being in cancer patients. SWB is being considered an important component of a comprehensive care program that influences other aspects of health. A strong association between spirituality and QoL among patients undergoing cancer chemotherapy has been identified.[26] It has been suggested that the treatment of breast cancer patients should address SWB along with physical health.[27] Breast cancer patients with higher scores of SWB were reported to have lower levels of stress, anxiety, and depression.[27]
It has been observed that higher SWB is associated with reduced death anxiety in cancer patients.[28]
Duration of intervention
Different duration of art therapies, MBAT intervention and mindfulness meditations have been investigated in studies and found to be effective in improving various aspects of psychological wellbeing. Reduction in distress levels and anxiety has been reported after a single session of art therapy[24,25,29] and 7 days of art therapy.[22]
While in a few studies on MBAT intervention, the duration was 12 sessions,[21] 8 weeks[20] and 12 weeks,[15] short duration of MBAT interventions have also been reported to be effective. A Japanese study[30] on advanced cancer patients suggested that a single session of Mindfulness Art Therapy Short version might activate physiologically, alleviate tension, and increase energy.
Regarding the duration of mindfulness meditation, significant results have been reported with varying duration of practice. In a study,[31] a single 20-min session of mindfulness meditation resulted in a greater sense of religious SWB and more positive religious-spiritual coping resources. It also increased positive feelings such as optimism, hope, security, contentment, peace, and compassion. It was also observed that physiological measures of novice meditators were similar to those of the experienced group following a single session of meditation training.[32] A brief mindfulness meditation training program (25 min each day for 3 days) has been shown to alter psychological and neuroendocrine responses to stress and buffers self-reported psychological stress reactivity.[33]
In our study, 7 days duration of intervention was selected to improve patients’ compliance, retain their participation, and reduce the number of drop-outs.
Mechanism of MBAT intervention
The probable mechanism for the effects of MBAT intervention can be attributed to different components of mindfulness as well as expression through mindful art [Table 4]. In mindfulness meditation, we used body scan (moving attention systematically from toes to head), non-judgmental awareness of the physical sensations, breathing, thoughts, and emotions. How these elements of mindfulness meditation can help alleviate the pain and emotional suffering in oncology patients has been explained by a few researchers. The body scan helps to develop an awareness of subtle changes happening moment to moment which makes unpleasant sensations more tolerable. It reduces pain-related distress and helps in relaxation.[34]
| Mindfulness meditation | Probable mechanism |
|---|---|
| Body scan (moving attention systematically from toes to head) | •Reduces pain related distress[34] • Helps in relaxation[34] |
| Non-judgmental awareness of the physical sensations | • Makes the sensation less frightening and less overwhelming[35] |
| Awareness of breathing | • Enhances the parasympathetic nervous system that is associated with calm, rest, and repair[36] |
| Non-judgmental awareness of thoughts and emotions | • Seeing things in a different perspective helps to observe habitual reactions and gives more control and choice to act in a more adaptive way[38] |
| Non-striving and acceptance of reality | • Prevents worry about the future and ruminating thoughts of past events[37] • Allows to live more fully in the present moment, regardless of what lies ahead[37] • Helps to alleviate the suffering that is often accompanied by pain or emotional discomfort[35] |
| Mindful Art | Probable Mechanism |
| Mindful exploration while art making with an awareness of sensory stimulus and response | • Relaxing and calming effect • Takes awareness away from the habitual thinking mind, towards heightened feeling and sensing • Promotes the activation of the parasympathetic nervous system[13] |
| Exploring present moment experiences | • Facilitates an experience of immersion, flow, focus and calm, accessing an inner witness and being absorbed in present-moment experience[39] |
| Art making with kindness, curiosity and non-judgment | • Helps to reconstruct meanings • Helps to minimize over identification with illness • Helps to negotiate experiences and life events on own terms[14] |
| Coloring | • Coloring induces a mindful or meditative state[23,24] • Reduces activity in the amygdala[40] • Changes brain waves activity[41] |
| Coloring complex geometric forms | • Facilitates a meditative-like state that helps reduce anxiety[24] • Helps to suspend the “inner dialogue” • Helps to deeply engage in the activity • Distracts from the negative thought patterns and emotions[24] |
Awareness of breathing helps to breathe more easily and often elicitates a relaxation response.[35] It can enhance the parasympathetic nervous system that is associated with calm, rest, and repair.[36] Mindfulness aims for non-striving and acceptance of reality as it is. This prevents worry about the future and ruminating thoughts of past events, allows to live more fully in the present moment, regardless of what lies ahead.[37] It helps to alleviate the suffering that is often accompanied by pain or emotional discomfort.[35] Seeing things from a different perspective helps to observe habitual reactions and gives more control and choice to act in a more adaptive way.[38] MBAT is also referred to as “focusing-oriented art therapy”, as it involves an emphasis on shifting focus as part of the experience. Mindful art is believed to facilitate a sense of immersion, flow, focus, calm, and being in the present-moment experience.[39]
It is often suggested that coloring induces a mindful or meditative state,[23,24] reduced activity in the amygdala,[40] or changes in brain waves activity.[41] Coloring is also referred to as mindfulness or meditative-like activity.[23] Coloring complex geometric forms help the participants to suspend the “inner dialogue” and deeply engage in the activity that removes them from the negative thought patterns and emotions that can sometimes dominate their lives.[24] The complexity and structure of these designs draw the participants into a meditative-like state that helps reduce anxiety.[24]
Limitations and recommendations for future research
The sample size was small hence study findings may have limited generalizability to those patients seeking care at study settings like ours. To substantiate the findings, there is a need for studies with larger samples that are more elaborate. The possibility of bias cannot be ruled out as we relied on self-report measures of psychological distress and SWB. Non-compliance by some patients in regards to inconsistency in daily home practice may have affected the outcome. We have studied the effectiveness of MBAT in breast cancer patients. It would be interesting to explore its potential role in other oncology populations. SWB may have different implications specific to gender, age, and cross-cultural issues. These variables can be explored in future research.
CONCLUSION
One week of MBAT intervention for breast cancer patients undergoing chemotherapy significantly decreased the psychological distress, significantly improved the SWB in terms of meaning, peace, faith, and total SWB from pre-session to immediate post-session and pre-session to post 1-week session. MBAT is a feasible, safe, cost-effective, and novel approach for improving psycho-social health and SWB in breast cancer patients undergoing chemotherapy. The results of this study determine the potential role of MBAT as an effective psycho-social intervention in an oncology setting. However, further validation is required by conducting randomized controlled trials with larger sample size.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Epidemiological assessment of distress during chemotherapy: Who is affected? J Taibah Univ Med Sci. 2019;14:448-53.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19-28.
- [CrossRef] [Google Scholar]
- A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J Palliat Med. 2015;18:286-98.
- [CrossRef] [PubMed] [Google Scholar]
- Mindfulness-based interventions in context: Past, present, and future. Clinical psychology: Sci Pract. 2003;10:144-56.
- [CrossRef] [Google Scholar]
- Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: A systematic review and meta-analysis of randomized controlled trials. Psychooncology. 2019;28:2257-69.
- [CrossRef] [PubMed] [Google Scholar]
- Mindfulness: Existential, loss, and grief factors in women with breast cancer. J Psychosoc Oncol. 2011;29:643-56.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in spirituality partly explain health-related quality of life outcomes after Mindfulness-Based Stress Reduction. J Behav Med. 2011;34:508-18.
- [CrossRef] [PubMed] [Google Scholar]
- A pilot study of improved psychological distress with art therapy in patients with cancer undergoing chemotherapy. BMC Cancer. 2020;20:899.
- [CrossRef] [Google Scholar]
- An Investigation of the Impact of Adding Art Therapy to Mindfulness Enhancement Training.
- [Google Scholar]
- Focusing-oriented art Therapy: Accessing the Body's Wisdom and Creative Intelligence London: Jessica Kingsley Publishers; 2008.
- [Google Scholar]
- Effectiveness of mindfulness-based art therapy for symptoms of anxiety, depression, and fatigue: A systematic review and meta-analysis. Complement Ther Clin Pract. 2020;2020:101246.
- [CrossRef] [PubMed] [Google Scholar]
- Mindfulness-based arts interventions for cancer care: A systematic review of the effects on wellbeing and fatigue. Psychooncology. 2021;30:240-51.
- [CrossRef] [PubMed] [Google Scholar]
- Mindfulness and Art Therapy Article. 2014. British Association of Art Therapist, Newsbriefing. Available from http://www.arttherapyandmindfulness.com/mindfulness-and-art-therapy-article [Last accessed on 2021 Aug 24]
- [Google Scholar]
- A pilot study of a mindfulness-based art therapy intervention in outpatients with cancer. Am J Hosp Palliat Med. 2018;35:1195-200.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of mindfulness-based art therapy on healthy quality of life in women with breast cancer. Asia Pac J Oncol Nurs. 2019;6:193.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of the distress thermometer worldwide: state of the science. Psychooncology. 2014;23:241-50.
- [CrossRef] [PubMed] [Google Scholar]
- Spiritual well-being as a component of health-related quality of life: The functional assessment of chronic illness therapy spiritual well-being scale (FACIT-Sp) Religions. 2011;2:77-94.
- [CrossRef] [Google Scholar]
- A qualitative analysis of experiential challenges associated with meditation practice. Mindfulness. 2015;6:848-60.
- [CrossRef] [Google Scholar]
- The insight knowledge of fear and adverse effects of mindfulness practices. Mindfulness. 2019;10:2172-85.
- [CrossRef] [Google Scholar]
- A randomized, controlled trial of mindfulness-based art therapy (MBAT) for women with cancer. Psychooncology. 2006;15:363-73.
- [CrossRef] [PubMed] [Google Scholar]
- Beneficial effect of mindfulness-based art therapy in patients with breast cancer a randomized controlled trial. Explore. 2016;12:333-40.
- [CrossRef] [PubMed] [Google Scholar]
- Sharpen your pencils: Preliminary evidence that adult coloring reduces depressive symptoms and anxiety. Creat Res J. 2017;29:409-16.
- [CrossRef] [Google Scholar]
- Stress management in young adults: Implications of mandala coloring on self-reported negative affect and psychophysiological response. Psi Chi J Psychol Res. 2016;21:16-28.
- [CrossRef] [Google Scholar]
- Can coloring mandalas reduce anxiety? A replication study. Art Ther. 2012;29:87-92.
- [CrossRef] [Google Scholar]
- Spirituality and associated factors among cancer patients undergoing chemotherapy. Jpn J Nurs Sci. 2020;17:e12276.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between spiritual wellbeing and stress, anxiety, and depression in patients with breast cancer. J Isfahan Med Sch. 2012;30:195.
- [Google Scholar]
- The relationship between spiritual wellbeing and depression or death anxiety in cancer patients in Bushehr 2015. Nurs Vulnerables. 2015;2:15-28.
- [Google Scholar]
- An art therapy group intervention for cancer patients to counter distress before chemotherapy. Arts Health. 2021;13:35-48.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in the autonomic nervous system and moods of advanced cancer patients by mindfulness art therapy short version. J Cancer Ther. 2016;7:13-6.
- [CrossRef] [Google Scholar]
- Spirituality in pain medicine: A randomized experiment of pain perception, heart rate and religious spiritual well-being by using a single session meditation methodology. PLoS One. 2018;13:e0203336.
- [CrossRef] [PubMed] [Google Scholar]
- A single session of meditation reduces of physiological indices of anger in both experienced and novice meditators. Conscious Cogn. 2016;40:54-66.
- [CrossRef] [PubMed] [Google Scholar]
- Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology. 2014;44:1-2.
- [CrossRef] [PubMed] [Google Scholar]
- Immediate effects of a brief mindfulness-based body scan on patients with chronic pain. J Behav Med. 2014;37:127-34.
- [CrossRef] [PubMed] [Google Scholar]
- Mindfulness meditation for oncology patients: A discussion and critical review. Integr Cancer Ther. 2006;5:98-108.
- [CrossRef] [PubMed] [Google Scholar]
- Fully Present: The Science, Art, and Practice of Mindfulness Boston, Massachusetts: Da Capo Lifelong Books; 2010.
- [Google Scholar]
- Mindfulness-based Cancer Recovery: A Step-by-step MBSR Approach to Help you Cope with Treatment and Reclaim your Life Oakland, California: New Harbinger Publications; 2011.
- [Google Scholar]
- Mindfulness-based stress reduction in breast cancer: A qualitative analysis. Complement Ther Clin Pract. 2012;18:221-6.
- [CrossRef] [PubMed] [Google Scholar]
- Mindfulness and the Arts Therapies: Theory and Practice London, N1 United Kingdom: Jessica Kingsley Pub; 2014. p. :24-36.
- [Google Scholar]
- Health Benefits of Coloring Books Attracting Adults to Childhood Pastime. 2015. Fox News. Available from http://www.foxnews.com/health/2015/12/28/health-benefits-coloringbooks-attracting-adults-to-childhood-pastime.html [Last accessed on 2021 Aug 24]
- [Google Scholar]
- The Science Behind Adult Colouring Books. 2015. Australia: Books and Arts; Available from https://www.abc.net.au/radionational/programs/archived/booksandarts/why-are-australian-adults-drawn-to-colouring-in-books/6750808 [Last accessed on 2021 Aug 24]
- [Google Scholar]






