Translate this page into:
Psychometric Assessment of SpiDiscI: Spiritual Distress Scale for Palliative Care Patients in India
*Corresponding author: Joris Gielen, Center for Global Health Ethics, Duquesne University, Pitsburgh, PA, United States. gielenj@duq.edu
-
Received: ,
Accepted: ,
How to cite this article: Gielen J, Kashyap K, Singh SP, Bhatnagar S, Chaturvedi SK. Psychometric assessment of SpiDiscI: Spiritual distress scale for palliative care patients in India. Indian J Palliat Care 2022;28:13-20.
Abstract
Objectives:
Spirituality has an impact on the quality of life of palliative care patients and it influences the way in which they experience their disease. Spiritual distress is a common issue among palliative care patients in India that is best assessed through a tool specifically designed for them. This study presents the findings of a psychometric assessment of SpiDiscI: a 16-item spiritual distress scale for Hindi speaking palliative care patients in India.
Materials and Methods:
This study used a non-experimental cross-sectional sample survey design. 400 cancer patients undergoing pain treatment at the pain and palliative care unit of a tertiary cancer hospital in New Delhi enrolled in the study and completed the study’s questionnaire. The questionnaire contained a section on demographic information, a numerical rating scale (NRS) for pain, SpiDiscI, FACIT-Sp-12, and WHOQOL-BREF. A subset of 50 patients with stable pain completed SpiDiscI a 2nd time 2 weeks after the first administration of the scale to assess test-retest reliability.
Results:
The scale’s internal consistency is very good (Cronbach’s Alpha 0.85). Spiritual distress scores ranged from 0 to 93.8 (mean 37.1, SD 23.6). Significant negative correlations between SpiDiScI and both FACIT-Sp-12 (R = –0.16, P = 0.001) and WHOQOL-BREF (R = –0.27, P < 0.001) confirmed convergent validity. There was no significant association with NRS pain scores (R = 0.06, P = 0.224). The highly significant association (R = 0.75, P < 0.001) of the scores on assessments 2 weeks apart confirmed test-retest reliability.
Conclusion:
SpiDiScI is a reliable and valid measure to assess spiritual distress in research among Hindi speaking palliative care patients in India.
Keywords
Spirituality
Spiritual distress
Scale
Palliative care
Hindi
INTRODUCTION
Studies have repeatedly shown the importance of spirituality to cancer patients at various stages of their disease. For instance, a study that included 340 seriously ill patients found that they ranked spiritual issues and concerns high in importance.[1] In another study, investigators assessed religious and spiritual themes in 68 patients’ experiences of advanced cancer. 78% (n = 53) confirmed the importance of religion and spirituality in the experience of their disease. Spirituality supported them through, among others, coping, beliefs, and community.[2] As a source of support, spirituality may have a substantial positive impact on quality of life. A qualitative study among patients with multiple myeloma found that spirituality exerted a large impact on quality of life in the view of the study participants.[3] A study that included 115 terminal cancer patients in hospice in Italy observed a positive association between spirituality and quality of life.[4] Although the importance of spirituality to advanced cancer patients has been confirmed in studies across cultures all over the world,[5] its meaning, significance, and interpretation may vary across patient populations. As a consequence, tools that have been designed to measure aspects of spirituality such as spiritual wellbeing or spiritual distress and have been shown to measure these aspects adequately among certain populations may not be equally effective in other populations. In this regard, FACIT-Sp-12 is an interesting example. FACIT-Sp stands for Functional Assessment of Chronic Illness Therapy—spiritual well-being scale. The number 12 refers to the 12 spirituality items contained in the scale. The items enquire about meaning in life, feeling at peace, the strength of belief, and faith, including faith in the future. The scale includes two subscales: one centered on meaning/ peace, and the second one on faith.[6,7] FACIT-Sp12 is used frequently in studies aiming to assess spirituality in cancer patients[8] and has been found to have good psychometric characteristics when used in such populations.[9] There is a Hindi version of this scale. Translations of FACIT-Sp12 are developed following a rigorous process including forward/ backward translation and testing.[10] Nevertheless, a close inspection of FACIT-Sp12’s Hindi version reveals that this tool may actually not accurately capture the spiritual wellbeing of Hindi-speaking palliative care patients in India. The original English version contains items that enquire after “reason for living,” “purpose in life,” “meaning and purpose,” and “faith and spiritual beliefs.” In the Hindi version, these concepts have been translated as “jīne kā kāraṇ,” “kisī udyeśya ke lie jīnā,” “artha yā udyeśya,” and “dhārmik yā ādhyātmik viśvās”. This kind of philosophical translation may be hard to grasp for patients undergoing treatment in palliative care in India because a majority of these patients have only had a very basic education or less.[11] Moreover, FACIT-Sp-12, like other spirituality scales and tools, fails to explicitly assess components of spirituality that are of central importance to many palliative care patients in India, such as belief in an all-powerful God and Karma or the conviction that every deed will have a corresponding consequence.[12-14] This does not mean that spirituality scales such as FACIT-Sp12 are necessarily useless in Hindi-speaking palliative care patients in India. However, spirituality may be better assessed by a tool that has been specifically developed for this population. This article describes the findings of a validation study of SpiDiscI, a spiritual distress scale for palliative care patients in India. Spiritual distress has been described as a “state of suffering related to the impaired ability to experience meaning in life through connectedness with self, others, world, or a Superior Being.”[15] The scale measures spiritual distress because an earlier study of 300 adult cancer patients receiving palliative care in India had shown that almost one in five of the studied patients suffered from spiritual distress.[11] Hence, spiritual distress can be considered a common problem in palliative care in India.
MATERIALS AND METHODS
Research design and procedures
This study used a non-experimental cross-sectional sample survey design. Between May 2017 and July 2019, the study questionnaire was administered to 400 cancer patients who presented for pain assessment at the pain and palliative care unit of the Dr. B.R. Ambedkar Institute Rotary Cancer Hospital (IRCH) at the All India Institute of Medical Sciences (AIIMS) in New Delhi. Physicians assessing patients at the pain clinic evaluated them for eligibility to participate in the study. In a few, straightforward sentences, they explained the study’s aims and informed the patient that it involves the completion of an interviewer-administered questionnaire. The physicians assured the patients that their decision whether or not to participate in the study would in no way affect their care at the clinic or in the hospital. Patients who showed interest to participate in the study were referred to one of the researchers (SPS, KK, JG). They provided the patients with more extensive information. Literate patients were given the Patient Information Sheet (PIS), so that they could quietly read it on their own. When they had read the document, the researcher reviewed the document with them to ensure that they had understood its content. The PIS was read to illiterate patients and the interviewer verified that they had understood its content. When the researcher had ascertained that the patient was still willing to participate in the study, the patient was offered to sign the informed consent form, whose content was also explained to the patient.
Patients who were 18 years or older and able to communicate in Hindi were eligible to participate. Patients could participate in the study only once. Patients were excluded from participation if they were showing signs of extreme pain, were visibly too distressed or anxious, had a history of neurological or psychiatric impairment, cognitive dysfunction, or alcohol or substance abuse, or had received treatment with investigational drugs within the last 30 days preceding the interview. Most of the items on the questionnaire were closed-ended resulting in quantitative data. Test-retest reliability of the spiritual distress scale was assessed among a subsample of 50 patients who were requested to complete the scale again after 2 weeks. 50 has been suggested to be an adequate size for assessing test-retest reliability.[16,17] Patients were requested to participate in the test-retest study if, in addition to the above inclusion criteria they had stable pain. Pain was considered stable if the patient’s NRS score has remained unchanged ±1 over the past 4 weeks and the patients were expected to present themselves again at the clinic after 2 weeks. Before this study, the questionnaire was piloted among 40 patients meeting the same inclusion and exclusion criteria as those of the full study. The study protocol was approved by the Institute Ethics Committee (IRB) of All India Institute of Medical Sciences (New Delhi, India, ref. no. IEC-239/04.05.2018) and the Institutional Review Board of Duquesne University (Pittsburgh, PA USA, Protocol ID 2018/04/3).
Instruments
The questionnaire consisted of five sections: Demographic information, a numerical rating scale (NRS) for pain, SpiDiscI, FACIT-Sp-12, and WHOQOL-BREF. In the demographic section, the interviewers recorded age, gender, marital status, diagnosis, prognosis, educational level, and religious affiliation. In addition to that, patients were asked to rate their prognosis and to briefly describe what they know about their illness. The section on physical pain contained just one item: a numeric rating scale with 11 categories, which is a commonly accepted unidimensional measure for pain.[18] Patients were asked to tell the interviewer how much pain they felt at the time of the interview by naming a number from zero to ten, with zero signifying no pain and ten the worst possible pain.
SpiDiScI is a Hindi-language scale to assess spiritual distress among Hindi-speaking palliative care patients in India. Within the context of this scale, palliative care patients are patients who have palliative care needs. The English-language version of the scale in [Table 1] is provided to give an idea of the content of the scale to people with limited skills in Hindi. Only the Hindi-version of the scale has been validated. The English-language version of the scale has not been validated and should not be used to administer the scale to research subjects. SpiDiscI was developed by selecting items from a 36-item Hindi spirituality questionnaire that the investigators had developed for a study of spirituality among palliative care patients in India. The extensive process that resulted in that questionnaire has been elaborately described elsewhere.[19] For the development of the more condensed scale, the investigators relied on the psychometric assessment of that questionnaire.[19] This resulted in the current scale with 16 unique binary items.
| Agree (%) | Disagree (%) | No answer (%) | ||
|---|---|---|---|---|
| 1 | Since the onset of my illness, I have become less interested in thinking about God or religion. | 103 (25.8) | 294 (73.5) | 3 (0.8) |
| 2 | I wonder why this illness has happened to me. | 266 (66.5) | 117 (29.3) | 17 (4.3) |
| 3 | I find it difficult to forgive others for wrong they did to me. | 94 (23.5) | 299 (74.8) | 7 (1.8) |
| 4 | This illness is unfair. | 296 (74) | 80 (20) | 24 (6) |
| 5 | I wonder what will happen after death. | 174 (43.5) | 208 (52) | 18 (4.5) |
| 6 | I am afraid of the future. | 199 (49.8) | 194 (48.5) | 7 (1.8) |
| 7 | I feel lonely. | 186 (46.5) | 212 (53) | 2 (0.5) |
| 8 | Since the onset of my illness, I have become less interested in hearing about God or religion. | 41 (10.3) | 355 (88.8) | 4 (1) |
| 9 | When I think of God, I feel agitated. | 35 (8.8) | 361 (90.3) | 4 (1) |
| 10 | Because of my illness, I find it difficult to do puja or other religious rituals. | 205 (51.2) | 189 (47.3) | 6 (1.5) |
| 11 | My illness or pain is a punishment for wrong done by me. | 194 (48.5) | 189 (47.3) | 17 (4.3) |
| 12 | Thinking about what will happen after death frightens me. | 158 (39.5) | 232 (58) | 10 (2.5) |
| 13 | God has abandoned me. | 90 (22.5) | 292 (73) | 18 (4.5) |
| 14 | Due to my illness, I have lost faith in a higher benevolent power. | 55 (13.8) | 342 (85.5) | 3 (0.8) |
| 15 | Since the onset of my illness I am wondering more often whether my decisions are good and right. | 110 (27.5) | 277 (69.3) | 13 (3.3) |
| 16 | I find it difficult to forgive myself for wrong I did. | 110 (27.5) | 283 (70.8) | 7 (1.8) |
The spiritual distress score is calculated by coding the answers as 1 for sahmat/agree and 0 for asahmat/disagree. Neutral responses are not coded and are not considered while calculating the distress score. There are two ways to calculate the distress score. Investigators may either calculate the mean score of all answers multiplied by 100, excluding neutral responses or they may calculate the percentage of positive (1) responses, excluding neutral responses. Both ways lead to the same score between 0 and 100. A higher score indicates more substantial spiritual distress. Researchers start administering the scale by requesting the research subject to answer in accordance with how he or she felt over the past 2 weeks. The neutral response is not to be presented as a standard answer category to the patients. It should only be used when patients, for whatever reason, find it impossible to either agree or disagree with a statement. Most often this will be because the item somehow does not apply to them. The scale has so far only been tested as an interviewer administered tool. Spiritual distress scores were to be compared with FACITSp-12 and WHOQOL-BREF. WHOQOL-BREF is a general measure of the quality of life developed by the WHO. It is a briefer version of the extensive WHOQOL-100 and is recommended in situations where it is essential to reduce the burden to respondents. WHOQOL-BREF is a widely used measure for quality of life, including that of cancer patients.[20-22] An international field trial, which included data from New Delhi, observed that the measure has good psychometric characteristics.[23]
Analysis
The investigators conducted a descriptive analysis of the demographic questions as well as the items of the spiritual distress scale and computed spiritual distress scores for each participant. They checked for associations between SpiDiscI, on the one hand, and demographic variables, the NRS for pain, FACIT-Sp-12, and the four domains of WHOQOL-BREF. The investigators did an explorative factor analysis of SpiDiscI. Test-retest reliability was assessed with the Pearson Correlation Coefficient. For the statistical analysis, IBM SPSS Statistics 26 was used. The factor analysis was performed with M. Basto’s and J.P. Pereira’s SPSS R-Menu for Ordinal Factor Analysis.[24] R was called from SPSS with IBM SPSS R Essentials.
RESULTS
In the sample, there were slightly more men (n = 224, 56%) than women (n = 176, 44%). Patients tended to be middle-aged adults, with the mean age 49.33 years (std. deviation 13.6). The youngest included patient was 18 years old, the oldest 81. A large majority of the patients were married at the time of the interview (n = 361). 29 patients (n = 7.2) were unmarried and 10 (n = 2.5) had been widowed. More than one fourth of the patients (28%, n = 112) were uneducated. 20.3% (n = 81) had studied until seventh grade (11 years) and 24.3% (n = 97) until tenth grade (16 years). 11.5% (n = 46) had completed intermediate education (18 years). 16% (n = 64) had at least an undergraduate degree. A large majority (82%, n = 328) was Hindu and 14.8% (n = 59) was Muslim. The remaining patients belonged to various religious or ideological minorities: Sikh (n = 6, 1.5%), Christian (n = 5, 1.3%), Buddhist (n = 1, 0.3%), and atheist (n = 1, 0.3%). Among these patients, the four most common types of cancer were head and neck carcinoma (21%, n = 84), lung cancer (16.8%, n = 67), genitourinary carcinoma (15.5%, n = 62), and breast cancer (14%, n = 56). The mean pain score for all patients was 4.62 (std. deviation 2.44). [Table 1] lists the numbers and percentages of participants who agreed and disagreed with the 16 items of SpiDiScI. Three indications of spiritual distress were observed in a majority (>50%) of patients: Wondering why the illness happened (item 2, 66.5%), the feeling that the illness is unfair (item 4, 74%), and difficulties to do religious rituals because of the illness (item 10, 51.2%). Five indications of spiritual distress were observed in at least one third of the patients but less than half of the patients(>33% and <50%): Wondering what will happen after death (item 5, 43.5%), fear of the future (item 6, 49.8%), feeling lonely (item 7, 46.5%), considering illness or pain a punishment for wrong done by the patient (item 11, 48.5%), and frightening thoughts about what will happen after death (item 12, 39.5%). Five out of the remaining eight items still occurred in at least one fifth (>20%) of patients: feeling less interested in thinking about God or religion (item 1, 25.8%), finding it difficult to forgive others (item 3, 23.5%) or oneself (item 16, 27%), thinking that God has abandoned oneself (item 13, 22.5%), and wondering whether decisions are good (item 15, 27.5%).
The very low percentages in the neutral or no-answer column indicate that, overall, the patients were able to apply nearly all sixteen spiritual distress items to their lives. The frequency of no-answers ranged from 0.5% for item seven on feeling lonely to 6% for item four on the unfairness of the illness. Five items were left unanswered by at least 4% of the research subjects (items 2, 4, 5, 11, and 13). All these items assessed philosophical or existential aspects of spiritual distress, such as wondering why the illness happened (item 2), finding the illness unfair (item 4), wondering what will happen after death (item 5), or the perception of illness as a punishment for sin (item 11).
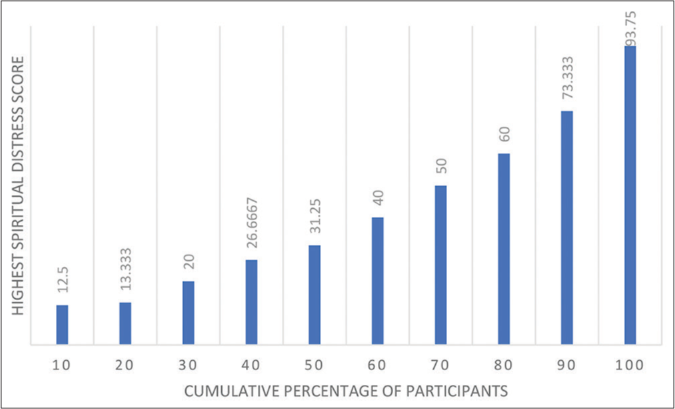
Spiritual distress scores were calculated for all participants. The lowest recorded spiritual distress score was 0. The highest was 93.8. The mean spiritual distress score was 37.1 (SD 23.6) and the median (quartile range) was 31.3 (18.8–53.3).
The skewness (0.508) and kurtosis (–0.580) for scale scores were within a tolerable range for assuming a normal distribution. However, the Kolmogorov–Smirnov test showed that the scale scores were not normally distributed (P < 0.001). 17 (4.25%) patients had a spiritual distress score of 0. 19 (4.75%) had a score of 6.25 and 41 (10.25%) scored 12.5, indicating that they gave an affirmative response to just one or two items respectively. [Graph 1] shows the number of participants within each tenth percentile of the spiritual distress score. Most commonly, participants scored between 10 and 20 (n = 80, 20%), followed by scores between 30 and 40 (n = 71, 17.75%) and scores between 20 and 30 (n = 49, 12.25%). [Graph 2] shows the ranked ascending spiritual distress scores highlighting the highest spiritual distress score within each tenth percentile of participants. The graph shows that 10% of participants had a spiritual distress score of 12.5 or less 80% scored 60 or less. Alternatively, this means that 20% of participants scored over 60.

- Histogram of spiritual distress scores.
- Histogram of spiritual distress scores per tenth participant percentile.
Convergent validity was confirmed by significant negative correlations between SpiDiScI and both FACITSp-12 (R = –0.16, P = 0.001) and WHOQOL-BREF (R = –0.27, P < 0.001). However, the correlation with NRS pain scores was not significant (R = 0.06, P = 0.224).
With a Cronbach’s Alpha of 0.85, the scale’s internal consistency is very good. Test-retest reliability was assessed using the Pearson correlation coefficient, which assessed the correlation between total scores the 1st time the scale was administered and a 2nd time 2 weeks later. The correlation was both high (R = 0.75) and highly significant (P < 0.001). To evaluate the dimensions of the scale, factor analysis was performed. For the factor analysis, we used the abovementioned SPSS menu for ordinal factor analysis with the orthogonal varimax rotation. Initial eigenvalues showed a first large factor with Eigenvalue 7.52 explaining 46.99% of the variance. The next factor had a much lower eigenvalue (2.06) explaining 12.84% of the variance and was followed by factors with Eigenvalues just above 1 or below. [Table 2] lists the sorted component loadings for the first two factors. There is substantial overlap between the factors, but, in factor 1, spiritual issues and concerns tend to be more focused on the patients themselves, while, in factor 2, there is an emphasis on God. In [Table 2], loadings <0.1 have been suppressed.
| Factor 1 | Factor 2 | ||
|---|---|---|---|
| 6 | I am afraid of the future | 0.855 | |
| 5 | I wonder what will happen after death | 0.851 | |
| 12 | Thinking about what will happen after death frightens me | 0.803 | 0.179 |
| 15 | Since the onset of my illness I am wondering more often whether my decisions are good and right | 0.742 | 0.351 |
| 7 | I feel lonely | 0.732 | 0.193 |
| 11 | My illness or pain is a punishment for wrong done by me. | 0.717 | 0.142 |
| 16 | I find it difficult to forgive myself for wrong I did | 0.708 | 0.323 |
| 4 | This illness is unfair | 0.525 | 0.403 |
| 10 | Because of my illness, I find it difficult to do puja or other religious rituals | 0.457 | 0.284 |
| 14 | Due to my illness, I have lost faith in a higher benevolent power | 0.851 | |
| 1 | Since the onset of my illness, I have become less interested in thinking about God or religion | 0.234 | 0.782 |
| 8 | Since the onset of my illness, I have become less interested in hearing about God or religion | 0.127 | 0.775 |
| 9 | When I think of God, I feel agitated | 0.142 | 0.738 |
| 13 | God has abandoned me | 0.575 | 0.626 |
| 3 | I find it difficult to forgive others for wrong they did to me | 0.525 | 0.533 |
| 2 | I wonder why this illness has happened to me | 0.422 | 0.530 |
Age was not correlated with spiritual distress scores. A Mann–Whitney test did not show an association between spiritual distress scores and gender, nor did Kruskal–Wallis tests reveal associations with marital status, diagnostic category, or religious affiliation. However, a Kruskal–Wallis test did show a significant association between spiritual distress scores and how participants expected their illness to evolve (Kruskal–Wallis χ2 = 17.97, df = 5, P = 0.003, with a mean rank factor score of 122.74 for I do not know anything about that, 135.43 for Very bad, 140.26 for Bad, 186.06 for Neither good, nor bad, 202.28 for Good, and 213.97 for Very good). [Table 3] shows that patients who expected the further evolution to be bad or very bad had higher average spiritual distress scores than patients who expected that evolution to be good or very good.
| How is your illness going to evolve in your opinion? | Mean | n | SD | |
|---|---|---|---|---|
| 1 | I do not know anything about that | 42.1132 | 128 | 23.50077 |
| 2 | Very bad | 54.3750 | 10 | 33.68177 |
| 3 | Bad | 39.7657 | 30 | 22.75841 |
| 4 | Neither good, nor bad | 37.3467 | 35 | 25.69617 |
| 5 | Good | 33.0960 | 168 | 21.82167 |
| 6 | Very good | 28.8488 | 28 | 21.89483 |
| Total | 37.0983 | 399 | 23.58047 | |
Further, a Kruskal–Wallis test revealed a significant association between spiritual distress scores and educational level (χ2 = 23.323, df = 5, P < 0.001, with a mean rank factor score of 222.17 for uneducated, 224.12 for less than class 7, 202.06 for until 10th, 169.86 for inter, 149.41 for undergraduate, and 149.04 for postgraduate). [Table 4] makes clear that there is a linear association between spiritual distress scores and educational level with patients who were less educated (uneducated, less than class 7, or until 10th), on average, scoring higher levels of spiritual distress than patients who had studied longer (until inter, undergraduate or postgraduate).
| Educational level | Mean | n | SD | |
|---|---|---|---|---|
| 1 | Uneducated | 41.8932 | 112 | 24.79901 |
| 2 | less than class 7 | 42.6438 | 81 | 25.39205 |
| 3 | Until 10th | 37.3275 | 96 | 23.15203 |
| 4 | Inter | 30.5228 | 46 | 19.55967 |
| 5 | Undergraduate | 26.1943 | 38 | 16.66600 |
| 6 | Postgraduate | 25.8913 | 26 | 18.11148 |
| Total | 37.0983 | 399 | 23.58047 | |
DISCUSSION
The findings of this study call for an evaluative assessment of the severity of spiritual distress among the studied patients. To be able to interpret the results, it is necessary to determine which scores of spiritual distress indicate light, moderate, or severe spiritual distress. Obviously, the 17 patients (4.25%), who had a spiritual distress score of 0, are not spiritually distressed. However, not all patients who have a score above 0 need necessarily be characterized as spiritually distressed. In a way, most people ask themselves existential or spiritual questions and may express insecurity about their answers.[25] Cancer patients who are confronted with the finitude of life may ponder more often about these questions.[26] This pondering in itself is not necessarily a sign of spiritual distress unless it starts impacting the quality of life. Therefore, it is no surprise that this study found a significant negative association between spiritual distress scores and quality of life (WHOQOL-BREF). This leads to the question of which spiritual distress score indicates a substantial level of spiritual distress that may need clinical attention.
It is hard to give a final answer to this question at this point due to the limitations of the collected data. The data were collected in one cancer setting. More data from more diverse palliative care settings will be required to determine levels of spiritual distress for SpiDiScI. However, a meaningful hypothesis can be derived from a comparison of the current findings with those of a study that analyzed the prevalence and nature of spiritual distress among palliative care patients in India. Studying a population very similar to the one of the current study and using an explorative quantitative research design, the authors concluded that 17.4% of included patients were spiritually distressed to an extent that would require intervention.[11] The current study observed that 20% of patients had a score over 60. This means that a score of 60 or more could be interpreted as a sign of severe spiritual distress.
Meaningful correlations of SpiDiScI with FACIT-Sp-12 and WHOQOL-BREF illustrated the validity of this measurement. These correlations were negative because SpiDiScI measures a negative experience (spiritual distress), while FACIT-Sp-12 and WHOQOL-BREF measure positive experiences (spiritual well-being and quality of life, respectively). Although the correlations with both FACIT-Sp-12 and WHOQOL-BREF were highly significant (P ≤ 0.001), they were not strong (R = –0.16 for FACIT-Sp-12 and R = –0.27 for WHOQOLBREF). This is not surprising. Quality of life, which is measured by WHOQOL-BREF, overlaps to some extent with spiritual well-being and, therefore, poor quality of life, can be expected to be associated with spiritual distress. A majority of studies that have assessed the relationship between spirituality and quality of life in healthcare have indeed found a significant association.[27,28] However, quality of life is a broader concept that, also, includes social relationships, as well as physical and environmental factors.[23] A very strong negative correlation between WHOQOL-BREF and SpiDiScI would, thus, have been unexpected.
More remarkable is the highly significant but weak negative correlation between SpiDiScI and FACIT-Sp-12. Since the former measures spiritual distress and the latter spiritual wellbeing, a nearly perfect negative correlation might have been expected. Yet, FACIT-Sp-12 is an international instrument that may not be as accurate among Hindi-speaking palliative care patients in India in India as SpiDiScI, which has been specifically developed to assess spiritual distress among this patient population. Within the context of the validation of SpiDiScI; however, the most important finding is not the strength of the correlation, but the fact that a significant correlation was observed, thus illustrating convergent validity.
Other indications of SpiDiScI’s psychometric quality can be derived from the scale’s Cronbach’s Alpha and the results of the test-retest assessment. The scale’s high Cronbach’s alpha (0.85) is indicative of very good internal consistency. Test-retest reliability was confirmed by a high statistically significant correlation between initial distress scores and distress scores that were measured 2 weeks later among patients with stable pain. This indicates that patients interpret the items consistently over time and that the results may be reliably replicated under similar circumstances.
This study, also, assessed associations of SpiDiScI with NRS pain scores and demographic factors. Although physical pain may make patients ask themselves spiritual questions, such as why they may be experiencing this pain, in the end, physical pain and spiritual distress are two distinct phenomena. It is, therefore, no surprise that no significant correlation was observed between SpiDiScI and NRS scores. The literature is ambivalent on the association between spirituality and pain, with some studies showing an association[11] and others not finding such an association.[29]
While assessing associations of SpiDiScI with demographic variables, no correction for multiple comparisons was undertaken due to the explorative nature of this part of the study. The observations can be compared with the findings of an earlier study that had assessed spiritual distress among Hindi speaking palliative care patients using an explorative research design that enabled the researchers to divide the studied patients into four groups: Trustful patients, spiritually distressed patients, and patients clinging to divine support. After the regression, the study found that spiritually distressed patients were more likely to be female, and less educated than patients in the other groups. No association was observed between the groups and age, marital status, religious affiliation, and how patients thought about their prognosis.[11] Interestingly, the current study largely found the same associations although it did not note an association for gender, while it did observe an association for spiritual distress and how patients expected their illness to evolve. The overall similarity in findings is another indication that SpiDiScI is an adequate measure of spiritual distress among the studied patient population.
It is not immediately clear why the previous study on spiritual distress among Hindi speaking palliative care patients found an association between spiritual distress and gender while the current study did not. It is possible that SpiDiScI is a more accurate measure of spiritual distress for this patient population and that the association that was observed in the previous study was due to chance. The association between spiritual distress and gender will require more attention in future research. On the other hand, the finding that patients who expected their illness to get worse, had, also, significantly higher spiritual distress scores is not surprising. Expectations, hope, and fear for the future are aspects of spirituality and, thus, of spiritual distress as well.[12] Fear by itself may be a sign of spiritual distress.[25] Moreover, SpiDiScI contains several items [items 5, 6, and 11 in Table 1] that assess fear of what will happen in the future or after death. Considering this, an association of higher spiritual distress scores with negative views of disease progression was expected.
Actually, the previous study on spiritual distress among Hindi-speaking palliative care patients[11] may not have found an association between spiritual distress and how patients rated their own prognosis because of the way in which the question was phrased. A majority of the patients had only had limited education and they may have struggled to understand the concept “prognosis” (Hindi: pūrvānumān) that was used in the questionnaire. Consequently, the finding of the study for that item may not be absolutely reliable.
This study has shown that SpiDiScI is a reliable and valid measure to assess spiritual distress in research among Hindi-speaking palliative care patients in India. However, this study and the scale have some limitations. First, this validation study was not multicentric. Although, the clinic in which this study was undertaken is part of a large tertiary hospital that treats patients from all over Northern India and from very diverse socio-economic, religious, and cultural backgrounds validation studies in other palliative care centers are recommended. Second, only the Hindi version of the scale has been validated. There is an English version of the scale, but that version has not been validated and should not be administered to patients even if their primary language is English. It is essential to develop and validate versions of SpiDiScI in other Indian languages so that the scale can be used outside the Hindi belt. Third, so far, SpiDiScI has only been validated for research purposes and, at this stage, should not be used as a diagnostic tool to determine treatment. Future research on the clinical value of the scale is required because there clearly is a need for tools to help healthcare providers in busy pain and palliative care clinics decide which patients need special attention to manage spiritual distress. Fourth, SpiDiScI has so far only been tested as an interviewer administered scale. Given the simple and straightforward nature of the items, SpiDiScI may work well as a self-administered scale among patients who are sufficiently literate, but this needs to be assessed. When the scale is interviewer administered, it would be meaningful to evaluate inter-rater reliability. Fifth, to gain insight into the score levels that correspond to light, moderate, or severe spiritual distress it might be helpful to compare scores of palliative care cancer patients with those of patients suffering from non-malignant chronic conditions such as diabetes or hypertension. Sixth, SpiDiScI is a straightforward spiritual distress scale that is both easy to use by researchers and not hard to complete by patients. In that capacity, the scale includes many items that enquire after negative emotions, such as fear and feelings of loneliness, abandonment, and injustice. Not all of SpiDiScI’s items are of such negative nature: some items are existential or philosophical (items 2, 4, 5, 11, and 13). Comparatively more patients left items regarding existential or philosophical issues unanswered. This seems to indicate that the patients could less readily relate to these items and found it harder to apply them to their lives. However, this does not mean that the issues that these existential items assessed are not a substantial source of distress for many patients. For example, although 6% did not answer item 4 “This illness is unfair,” 74% agreed with the statement. Likewise, 4.5% did not provide an answer to item 5 “I wonder what will happen after death,” but 43.5% agreed with the statement. It has to be added that in the experience of the investigators who administered the scale, the large number of items enquiring after negative emotions, was not a burden to the patients. On the contrary, after the interview was over, many patients expressed relief that finally, someone seemed to be interested in the spiritual thoughts and feelings that they had been unable to express for a long time.
CONCLUSION
This study has shown that SpiDiScI is a reliable and valid measure to assess spiritual distress in research among Hindi speaking palliative care patients in India. The scale’s direct and short items that are easy to understand by patients and the fact the collected data are easy to enter and analyze make the scale a valuable tool for research in the target population. Interesting avenues for future research among the target population include studies on the association of spiritual distress scores with stage and site of disease and further evaluation of associations with demographic factors. Future validation studies of SpiDiScI should focus on different palliative care populations, the validation of translations of the scale in other languages, and the assessment of its clinical validity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This study was funded by an extramural research grant of the Indian Council of Medical Research.
Conflicts of interest
There are no conflicts of interest.
References
- Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476-82.
- [CrossRef] [PubMed] [Google Scholar]
- If god wanted me yesterday, I wouldn't be here today": Religious and spiritual themes in patients' experiences of advanced cancer. J Palliat Med. 2010;13:581-8.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding what matters most to people with multiple myeloma: A qualitative study of views on quality of life. BMC Cancer. 2014;14:496.
- [CrossRef] [PubMed] [Google Scholar]
- Spirituality, quality of life, psychological adjustment in terminal cancer patients in hospice. Eur J Cancer Care (Engl). 2016;25:961-9.
- [CrossRef] [PubMed] [Google Scholar]
- Spiritual care im globalisierten gesundheitswesen In: Historische Hintergründe und Aktuelle Entwicklungen. Darmstadt: Wissenschaftlichen Buchgesellschaft; 2019.
- [Google Scholar]
- A case for including spirituality in quality of life measurement in oncology. Psychooncology. 1999;8:417-28.
- [CrossRef] [Google Scholar]
- Spiritual well-being as a component of health-related quality of life: The functional assessment of chronic illness therapy-spiritual well-being scale (FACIT-Sp) Religions. 2011;2:77.
- [CrossRef] [Google Scholar]
- Spirituality and well-being in cancer patients: A review. Psychooncology. 2010;19:565-72.
- [CrossRef] [PubMed] [Google Scholar]
- Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy-spiritual Well-being scale (FACIT-Sp) Ann Behav Med. 2002;24:49-58.
- [CrossRef] [PubMed] [Google Scholar]
- A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Eval Health Prof. 2005;28:212-32.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and nature of spiritual distress among palliative care patients in India. J Relig Health. 2017;56:530-44.
- [CrossRef] [PubMed] [Google Scholar]
- Spirituality as an ethical challenge in Indian palliative care: A systematic review. Palliat Support Care. 2015;14:561-82.
- [CrossRef] [PubMed] [Google Scholar]
- Belief in karma and mokṣa at the end of life in India In: Selin H, Rakoff RM, eds. Death Across Cultures: Death and Dying in Non-Western Cultures. Cham: Springer International Publishing; 2019. p. :19-39.
- [CrossRef] [Google Scholar]
- Spiritual concerns in hindu cancer patients undergoing palliative care: A qualitative study. Indian J Palliat Care. 2013;19:99-105.
- [CrossRef] [PubMed] [Google Scholar]
- Spiritual distress-proposing a new definition and defining characteristics. Int J Nurs Knowl. 2013;24:77-84.
- [CrossRef] [PubMed] [Google Scholar]
- Measures of reliability in sports medicine and science. Sports Med. 2000;30:1-15.
- [CrossRef] [PubMed] [Google Scholar]
- A critical analysis of test-retest reliability in instrument validation studies of cancer patients under palliative care: A systematic review. BMC Med Res Methodol. 2014;14:8.
- [CrossRef] [PubMed] [Google Scholar]
- Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: A systematic literature review. J Pain Symptom Manage. 2011;41:1073-93.
- [CrossRef] [PubMed] [Google Scholar]
- Development and psychometric assessment of a spirituality questionnaire for indian palliative care patients. Indian J Palliat Care. 2016;22:9-18.
- [CrossRef] [PubMed] [Google Scholar]
- Does awareness of diagnosis influence health related quality of life in North Indian patients with lung cancer? Indian J Med Res. 2016;143:S38-44.
- [CrossRef] [PubMed] [Google Scholar]
- A cross-sectional comparison of quality of life between physically active and underactive older men with prostate cancer. J Aging Phys Act. 2016;24:642-8.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life after first-line anti-cancer treatments for advanced non-small cell lung cancer in clinical practice. Qual Life Res. 2016;25:1441-9.
- [CrossRef] [PubMed] [Google Scholar]
- The World Health Organization's WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299-310.
- [CrossRef] [PubMed] [Google Scholar]
- Making Sense of Spirituality in Nursing and Health Care Practice: An Interactive Approach (2nd ed). London, United Kingdom: Jessica Kingsley Publishers; 2006.
- [Google Scholar]
- Spirituality and religion in oncology. CA Cancer J Clin. 2013;63:280-9.
- [CrossRef] [PubMed] [Google Scholar]
- Relational spirituality and quality of life 2007 to 2017: An integrative research review. Health Qual Life Outcomes. 2018;16:75.
- [CrossRef] [PubMed] [Google Scholar]
- Quality-of-life and spirituality. Int Rev Psychiatry. 2017;29:263-82.
- [CrossRef] [PubMed] [Google Scholar]
- Spiritual pain among patients with advanced cancer in palliative care. J Palliat Med. 2006;9:1106-13.
- [CrossRef] [PubMed] [Google Scholar]






