Translate this page into:
Experience in Strategic Networking to Promote Palliative Care in a Clinical Academic Setting in India
Address for correspondence: Dr. Shoba Nair; E-mail: nair.shoba@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Palliative care in low and middle-income countries is a new discipline, responding to a greater patient need, than in high-income countries. By its very nature, palliative as a specialty has to network with other specialties to provide quality care to patients. For any medical discipline to grow as a specialty, it should be well established in the teaching medical institutions of that country. Data show that palliative care is more likely to establish and grow in an academic health care institution. It is a necessity that multiple networking strategies are adopted to reach this goal.
Objectives:
(1) To describe a strategic approach to palliative care service development and integration into clinical academic setting. (2) To present the change in metrics to evaluate progress.
Design and Setting:
This is a descriptive study wherein, the different strategies that are adopted by the Department of Palliative Medicine for networking in an academic health care institution and outside the institution are scrutinized.
Measurement:
The impact of this networking was assessed, one, at the level of academics and the other, at the level of service. The number of people who attended various training programs conducted by the department and the number of patients who availed palliative care service over the years were assessed.
Results:
Ten different strategies were identified that helped with networking of palliative care in the institution. During this time, the referrals to the department increased both for malignant diseases (52–395) and nonmalignant diseases (5–353) from 2000 to 2013. The academic sessions conducted by the department for undergraduates also saw an increase in the number of hours from 6 to 12, apart from the increase in a number of courses conducted by the department for doctors and nurses.
Conclusion:
Networking is an essential strategy for the establishment of a relatively new medical discipline like palliative care in a developing and populous country like India, where the service is disproportionate to the demands.
Keywords
Academic institution
Networking
Palliative care
INTRODUCTION
Palliative care is a nascent discipline in India even after two decades of its introduction. Because of its holistic approach in patient care, palliative care should be looked at as a public health strategy in any country.[1] Although World Health Organization (WHO) identifies the three tenets of how to introduce a public health strategy (education, policy, drugs), there has been very little guidance or data on how to do this. Palliative care requires the expertise of doctors, nurses, social workers, administrators, and other health care professionals who understand chronic and life-limiting illness. Data show that palliative care is more likely to establish and grow in an academic hospital.[2] Networking between different specialties in the hospital is very essential for its growth.
Networking can be defined as the exchange of information or services among individuals, groups or institutions. Palliative medicine is, by its very nature, multi-disciplinary, and complements other specialties.[3] In the United States, the field of hospital palliative care has grown rapidly in recent years in response to patient need and clinician interest in effective approaches to managing chronic life-limiting illness.[4] Creating and fostering an effective team is one of the greatest challenges for providers of palliative care and for this, networking both inside and outside an institution is important.[56] For providing quality care, each hospital in the country should have a palliative care team that can provide both hospice and nonhospice care.[7] This will happen only if a postgraduate program is established in palliative medicine. Therefore, needless to say, networking and growth of palliative medicine in a teaching institution is imperative. Here, we present a strategic approach to establish palliative care as an important specialty in a teaching tertiary care hospital in Bengaluru, India. In order to evaluate the success of this, we present process metrics: Change in both teaching contact hours for undergraduate medical curriculum, other palliative care courses conducted and in numbers of patients referred to the palliative care service.
METHODS
Setting and study procedures
The study was carried out at St. John's Medical College Hospital, Bengaluru, India. Different strategies of networking that were used over the years (2000–2013) were recalled and discussed between the team members. Our team comprises of three doctors, one nurse and a social worker at any given point of time.
More than 5000 patient records were reviewed. The records were divided into malignant and nonmalignant groups. The number of patients in each group was taken into account to analyze the outcome of networking.
RESULTS
Strategies for networking
A number of strategies to spread the awareness of palliative care were identified at St. John's Medical College Hospital, Bengaluru. They are described below [Table 1].
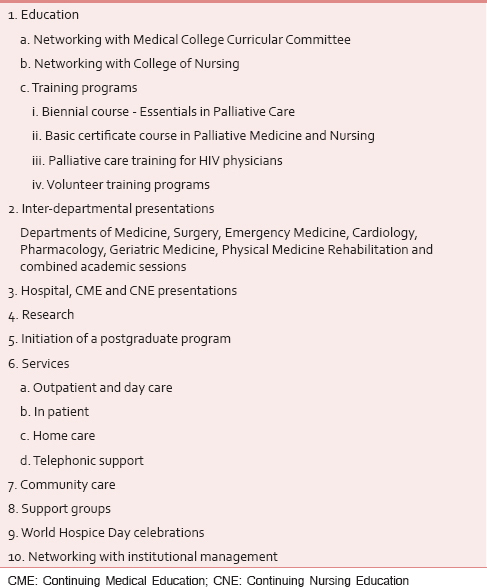
Education
St. John's Medical College Bengaluru is the first institution in the country to begin undergraduate medical and nursing training in palliative care. This was initiated in the year 2001.[8]
The medical undergraduates started with 6 h of palliative care training as part of anesthesia lectures in the year 2001. To understand the impact of these training hours a pre- and post-test analysis was done for one batch of medical and nursing students and the results were published in the Indian Journal of Palliative Care in the year 2004.[8] After liaising with the dean and different clinical departments such as Medicine, Surgery, Gynecology, and Clinical Ethics, the number of lecture hours was increased to a total of 12.
Networking with college of nursing
The nursing students have 4 h of palliative care training in their third term. Apart from lectures on pain and palliative care, nursing students are also posted for practical experience in the department since 2008.
Training programs
In the years 2002 and 2003, training programs were conducted for doctors and nurses in collaboration with other institutions such as Kidwai Memorial Institute of Oncology and Rammiah Medical College, Bengaluru. Around 50 doctors and 100 nurses attended the program. Since 2008, the department has been conducting regular training programs for doctors and nurses under the auspices of the Indian Association of Palliative Care (IAPC).
Biennial course - Essentials in palliative care
The biennial course, running under the auspices of the IAPC is a 2-month distance-learning program with 15 h of contact session for doctors and nurses. The number of participants for the contact session is usually between 15 and 25. Topics such as pain, symptom management, communication skills, ethics, and end of life care are covered during the contact sessions. The candidates need to submit a case reflection and give a written exam at the end of 2 months. The exam consists of multiple choice, true or false, short answer questions and Spotters. This program started in June 2008. Eleven courses have been conducted till December 2013.[9]
Basic certificate course in palliative medicine and nursing
This 1-month residential course was initiated in the year 2013. Two courses have been conducted to date. These courses provide hands-on training to doctors and nurses and equip them to run a palliative care unit in their place of work. One nurse from Nagaland, a Northeastern State in India and a doctor from Bengaluru attended the first course. Two nurses attended the next course from a rural hospital at Chatharpur, a remote village in Uttarakhand, a Northern State in India.
Palliative care training for human immunodeficiency virus physicians
This training program was designed for doctors who treated human immunodeficiency virus (HIV) patients at community care centers, set up by the National Acquired Immune Deficiency Syndrome Control Organization in rural settings in Karnataka. It was a 3 day course with a pre- and post-test to assess the knowledge and attitude toward palliative care issues in HIV patients. This was an activity initiated by our department in the institution. Seventeen doctors from rural parts of Karnataka underwent training. Due to the lack of funds, this course could not be continued.
Palliative care introductory lectures were also part of HIV training program initiated by Karnataka Health Promotion Trust under the “Samastha” project. Faculty members from our department used to deliver the lecture on palliative care in these training programs. This program was closed in 2011 at the end of 5 years. Around 200 doctors were trained under this program.
Volunteer training program
Introductory lectures were conducted for volunteers in the year 2009 and 2010. Volunteers in batches of 5–10 have been trained in the department. They were given 5 h of training that included an overall understanding of palliative care, physical care of the patients, emotional and spiritual care. Altogether around 12 volunteers were trained in 2 years.
Inter-departmental presentations
Palliative care introductory lectures and pain management lectures were conducted in the Departments of Medicine, Surgery, Emergency Medicine, Cardiology, and Pharmacology in a span of 2 years from 2009 to 2011. The lectures were prepared and taken by faculty in the department. In the year 2013, a once a month integrated academic session, between the Departments of Palliative Medicine, Physical Medicine Rehabilitation. and Geriatric Medicine was initiated.
Continuing medical education and nursing education presentations
The institution has regular clinical meetings every Friday and several topics in palliative medicine, including pain and its management, end of life care, symptom control, palliative care in Geriatrics, etc., have been presented. At least 12 presentations were performed over the years in Friday clinical meetings. Nursing education is also active in the institution and lectures on assessment of pain, long-term care of the patient, care of the dying, etc., have been conducted by faculty in the department.
Research
Research work on pain in HIV, burns, geriatrics, prevalence and patterns of anxiety and depression in palliative care patients, assessment of knowledge after palliative care training for medical and nursing students etc., have been carried out by the department.[810] These projects enabled networking with other departments.
Starting a postgraduate program
A specialty board for curriculum development for postgraduate course in palliative medicine and also for laying the guidelines for faculty criteria and infrastructure that is needed for the initiation of the postgraduate program, was set up by the Medical Council of India, in the year 2011. Initial work has begun in the institution towards commencing a postgraduate program in palliative medicine. University inspection was successfully completed and at this point, in time, we are awaiting inspection by the Medical Council of India after which we would be able to initiate the postgraduate program.
Services
Outpatient and day care
The Outpatient services began in the year 2000. It includes clinical assessment and management, psychosocial assessment and management, counseling, procedures such as ascitic tap, pleural tap, lymphoedema massage, lympha press machine application, and bereavement support.
In-patient
The in-patient admission was initiated in the year 2010. Patients are admitted from pain and palliative outpatient services or referred from other specialties, or directly admitted from emergency medicine for symptom management, or end of life care.
Home care
Home care is carried out on a need basis within 8 km around the hospital, for symptom management, counseling, and end of life care. Doctor, nurse team visits are conducted.
Telephonic support
Patients on morphine are given a call twice a month from the department to assess their pain relief and other symptoms. Advice regarding adjustment of the dose, management of side effects such as constipation, nausea, etc., is given over the phone mostly by the nursing staff. Patients and relatives also call the department for advice on pain relief and other symptoms such as fatigue, nausea, vomiting, constipation, etc.
Community care
The department is collaborating with a Community Care Centre for HIV patients. There is an in-house doctor and in-patient and outpatient service. Once a week, a physician from our team visits the Community Centre to provide palliative care. This was initiated in the year 2008.
Support groups
Group therapy is organized for patient support regularly. Previously treated patients’ families and patients with their family members participate in this group therapy. Common problems and how to tackle them are discussed at the support group meetings.
World Hospice Day celebrations
World Hospice Day was celebrated to raise awareness, along with other hospitals in the city by participating in walkathons in the early days of the establishment of the unit. From 2009 onward the world hospice and palliative care day is being celebrated in the institution with lectures for health care professionals, plays and exhibitions for the public and staff.
Networking with the institutional management
There has been strong institutional support in the growth of palliative care in the institution. Even when the Medical Council of India does not have a prescribed curriculum in palliative care for undergraduates, the management has been very supportive in including palliative care in the undergraduate curriculum. Academic posts for medical staff were created, and one staff nurse has been allotted specifically for palliative care. Infrastructure is also being taken care of. Apart from a palliative care outpatient area and office area, there is provision for an exclusive palliative care ward.
RESULTS
Outcome of networking
The outcome of networking can be assessed by the change in metrics. Metrics in this context indicates the number of patients who have availed palliative care service and the number of health care professionals who got trained in palliative care.
Patient census
Analyses of patient data for both malignant and nonmalignant diseases clearly indicate that the utilization of services as indicated by the number of patients that availed the service has increased. Over the past few years, the number of patients has increased at a faster rate when compared to previous years [Figures 1 and 2].
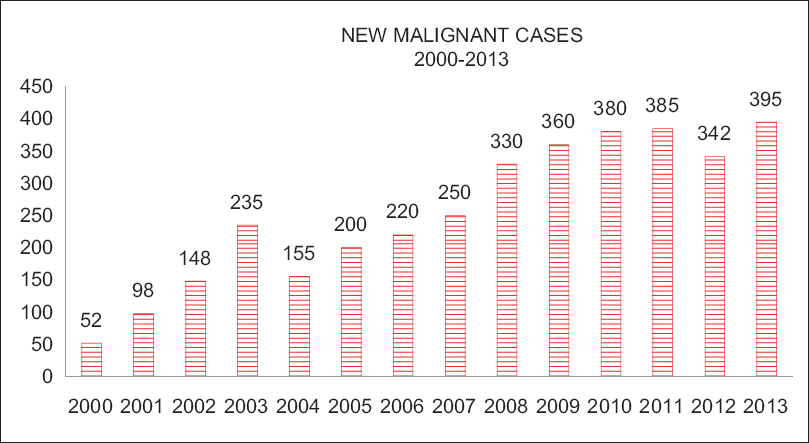
- New malignant cases
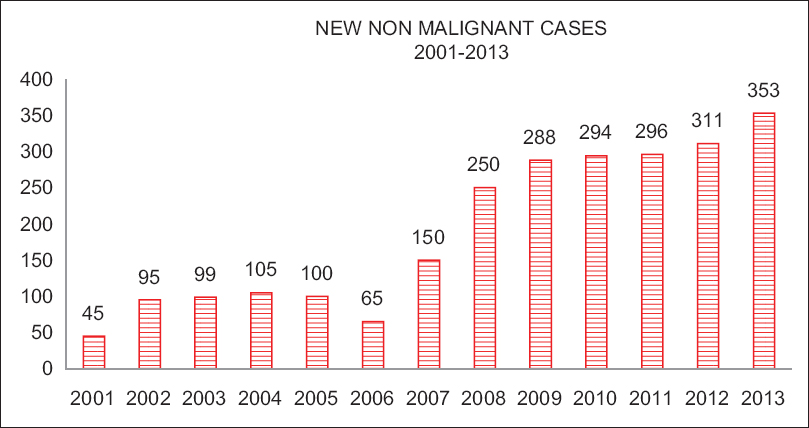
- New nonmalignant cases
Nonmalignant diseases include, congestive cardiac failure, renal failure, chronic obstructive pulmonary disease, burns, diabetic neuropathy, HIV infection, postherpetic neuralgias, chronic back pain, phantom limb pain, and peripheral vascular disease.
Academic census
St. John's Medical College Hospital is the first medical institution in the country to include palliative medicine as part of the undergraduate medical and nursing curricula.[8] Since last decade, regular undergraduate training in palliative care has been undertaken in the Medical and Nursing College. Over 600 medical students and 1000 nursing students have attended palliative care classes during their training.
Hundred and twenty seven doctors and 138 nurses have got trained in the biennial course -Essentials in Palliative Care run under the auspices of IAPC since 2008–2013. Seventeen doctors got training in HIV palliative care. One doctor and three nurses attended the 1-month basic certificate course.
Other outcomes
Over the years, the awareness amongst health care professionals in the institution, about palliative medicine has improved. This can be noted by observing that specialty doctors other than oncologists are referring patients to the service, and more health care professionals are attending the courses that are conducted by the department. Specialties such as Plastic surgery, Vascular surgery, Geriatrics, Pediatric Surgery, General Medicine, Orthopedics, Surgery, Dermatology, etc., regularly refer patients for palliative care. These referrals are for either pain and symptom management or end of life care. Many staff members are more interactive with the department and over the years, their confidence level with the services given by the department is on the rise.
DISCUSSION
Networking pays a rich dividend in the growth of any new initiative. If we look at the growth of palliative care worldwide, it is through networking that it has achieved its current status.[1112131415]
In the United Kingdom where it all began, a draft strategic plan for palliative care written for England for 2000–2005, suggests that managed networks of palliative care services will coordinate access to care and links with other relevant local networks. It strongly advocates training and research development to include in the educational program.[11]
According to Weissman et al., hospital palliative care programs in the United States are growing in number, scope, and sophistication. This was possible because of good networking between the public and the private sector.[12]
In their position statement drafted by Bruera et al., The American Academy of Hospice and Palliative Medicine states that, academic medical centers can no longer afford to look at palliative care as an optional, “nice to have” program with a mission and responsibility to be leaders in health care. A robust academic palliative care program is increasingly a key component for achieving success in the clinical, educational, and research missions of an Academic Medical Centre.[13]
Kaasa et al., states that starting the organizational development of palliative care at the tertiary level has been crucial for educational and audit purposes and has provided an excellent basis for networking in Norway. They state that palliative care in Norway has evolved in close cooperation between the health authorities and health care professionals.[14]
In Asia, the concept of palliative care was introduced in the early 80s and has grown in leaps and bounds. In their book, Hospice and Palliative Care in the South East Asia, Wright et al. describe the growth of palliative care in Malaysia, Thailand and Philippines. They state that this was achieved through international networking and collaboration.[15]
In India, the growth of palliative care has been mainly in the Southernmost State, Kerala. The palliative care movement in India began in Calicut, Kerala in 1993 with the establishment of Pain and Palliative Care Society, a Non-Governmental Organization in the premises of Calicut Medical College. Community link centers were established following this. Volunteers were trained and were given the support and the freedom to set up new link centers. Today there are around 265 centers in the Northern districts of Kerala. This has been possible with excellent local networking called the Neighborhood Network in Palliative Care (NNPC). NNPC is now a WHO Demonstration Centre for Palliative Care networking in the developing world.[16]
Thus, if we look at the growth of palliative care across the world, it is because of wide networking between countries, within countries, regions and institutions, and collaboration between resource rich and resource poor countries.
Our program got established in the institution due to strategic planning and long-term vision. Other specialties recognized the need for pain management and palliative care due to constant awareness programs, clinical discussions, palliative care team's direct communication with consultants and most importantly patient care. The next step is the establishment of a postgraduate program in the specialty.
Due to lack of outcome measures we don’t yet have evidence of patient outcomes. Since the referrals were not huge in numbers, we were able to provide optimum care to patients. Had the number of referrals increased exponentially, we would not have been in a position to accept patients for providing palliative care. More resources and personnel are the need of the hour.
CONCLUSIONS
Networking with different departments in the institution and outside has helped palliative care grow as a specialty in the institution. More doctors and nurses look at palliative care as a specialized area and are keen to have palliative care team's input in the management of patients. We have gained the trust of other specialties as a reliable team whose inputs are needed, through the service and academic programs. Networking at the national level has helped to initiate the process of establishing palliative medicine as a specialty in the country.
Clinical, educational, demographic, and financial imperatives driving this growth should not be ignored, and networking should not be looked at as a one-off procedure. It should be continuous and sustained. Each academic medical institution in the country can adopt a strategy for the establishment of palliative care as a specialty. Now that many states in India are adopting palliative care policy in their health service and Medical Council of India has approved the new postgraduate course in palliative medicine, let us hope that more institutions will take up palliative care and establish it as a specialty. Undoubtedly this would lead to the creation of health care professionals who can provide holistic care for our well deserving patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Dr. Richard Harding, Reader in Palliative care, Director of Global Programmes and Partnerships, King's College London. Dr. Maria Ekstrand, Professor of Medicine, Division of Prevention Science University of California, San Francisco and Adjunct Professor, St. John's Research Institute, Bengaluru. Dr. Vatsala P, Assistant Professor, Palliative Medicine, St. John's Hospital, Bengaluru for their valuable contributions.
REFERENCES
- Available from: http://www.who.int/gb/ebwha/pdf_files/A61/A61_R21-en.pdf
- The growth of palliative care programs in the United States hospitals. J Palliat Med. 2005;8:1127-34.
- [Google Scholar]
- Networking of palliative care at the corporate level. Indian J Palliat Care. 2011;17:20-2.
- [Google Scholar]
- Introduction of palliative care into undergraduate medical and nursing education in India. A critical evaluation. Indian J Palliat Care. 2004;10:55-60.
- [Google Scholar]
- Available from: http://www.Palliative care.in
- Prevalence of pain in patients with HIV/AIDS. A cross-sectional survey in a South Indian State. Indian J Palliat Care. 2009;15:67-70.
- [Google Scholar]
- Operational features for hospital palliative care programs: Consensus recommendations. J Palliat Med. 2008;11:1189-94.
- [Google Scholar]
- Academic Palliative Medicine Task Force of the American Academy of Hospice and Palliative Medicine. AAHPM position paper: Requirements for the successful development of academic palliative care programs. J Pain Symptom Manage. 2010;39:743-55.
- [Google Scholar]
- Palliative care in Norway: A national public health model. J Pain Symptom Manage. 2007;33:599-604.
- [Google Scholar]
- Hospice and Palliative Care in South east Asia. A Review of developments and challenges in Malaysia, Thailand and the Philippines. New York: Oxford University Press; 2010.
- [Google Scholar]
- The evolution of palliative care programmes in North Kerala. Indian J Palliat Care. 2005;11:15-8.
- [Google Scholar]






