Translate this page into:
Exploring Influence of Spiritual Well-being on Caregiver Burden in Head-and-Neck Malignancy: A Cross-sectional Study
*Corresponding author: Rutam Bhalendu Vaishnav, Undergraduate Section, Pramukhswami Medical College, Bhaikaka University, Karamsad, Gujarat, India. aurorutam@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vaishnav RB, Mishra G, Sharma Y, Ganjiwale JD, Kumar D, Bhatt D. Exploring Influence of Spiritual Well-being on Caregiver Burden In Head-and-Neck Malignancy: A Cross-sectional Study. Indian J Palliat Care. 2025;31:60-6. doi: 10.25259/IJPC_271_2024
Abstract
Objectives:
Taking care of a patient with head-and-neck malignancy (HNM) entails enormous physical, emotional, cognitive and moral challenges. Caregivers frequently turn to spiritual practices such as prayer, offering and meditation to enhance inner strength and coping ability. Assessment of caregiver burden (CGB) would remain incomplete without considering spiritual well-being (SWB). We set out to assess CGB and SWB in caregivers of patients suffering from HNMs.
Materials and Methods:
This cross-sectional study was carried out in a medical college-associated tertiary care centre after approval from the institutional ethics committee. CGB was determined using a translated version of Zarit Burden interview 22. SWB was determined by the spiritual wellbeing scale (SWBS), which was translated into Gujarati and validated. Relevant demographic data were also collected and analysed.
Results:
(1) Patient characteristics: (i) Number of participants: 60 (37 males and 23 females). Mean age: 55.56 years, (ii) Mean time since diagnosis: 7.33 months, (iii) Type of malignancy: Buccal mucosae 31, tongue 12, hard palate 7, lip 4, others 6, (iv) Type of family: Nuclear 14, joint 46. Locale: Rural: 36, urban: 24. (2) Caregiver characteristics: (i) Mean age: 44 years, (ii) Educational status: Graduate and above: 19, undergraduate: 22, primary education: 19, (iii) Occupation: Home-makers: 13, skilled: 18, semi-skilled: 18, others: 6. (3) CGB scores: Mean: 35.30 (Standard deviation [SD] = 11.25). Mild, moderate and high burden were reported by 66.7%, 25% and 3.3% caregivers, respectively. 5% of caregivers reported no burden. (4) SWB score: Mean: 81.70 (SD = 14.84). Low, moderate and high SWB scores were observed in 1.7%, 93.3% and 5%, respectively. (5) There was a significant correlation between higher SWB and lower CGB scores at 0.01 level.
Conclusion:
Moderate/high SWB was observed in 95% of caregivers regardless of their educational, social and family backgrounds. There was a significant correlation between higher SWB and lower CGB scores.
Keywords
Caregiver burden
Head-and-neck malignancy
Spiritual well-being
INTRODUCTION
Caregiver burden (CGB) is defined as the multifaceted strain perceived by the caregiver from caring for a family member over time.[1] Caregivers play a crucial role in supporting patients through the journey of cancer diagnosis, treatment and recovery. Extending beyond patients, health-related suffering impacts caregivers physically, mentally, economically, socially and spiritually. Determinants, impact and remedial measures for alleviating CGB have been studied extensively in diverse illnesses and diverse populations such as Parkinson’s disease, dementia, malignancies and mental health disorders.[2-4]
‘Head-and-neck malignancies’ (HNMs) are a group of cancers arising in the lip, oral cavity, pharynx, larynx and paranasal sinuses. HNM accounts for about 30% of all cancer cases. 57.5% of global head-and-neck cancers occur in Asia, especially in India.[5] Late-stage presentation, lack of access to cancer care and failure to complete treatment lead to poor survival in HNM patients.[6]
Health-related suffering extends to the immediate caregiver and family physically, mentally, economically, socially and spiritually. Caring for a person living with HNM is extremely challenging.[7] Caregivers play a crucial role in supporting patients through the journey of cancer diagnosis, treatment and recovery. Caregivers of HNM patients often must take on tasks that require nursing or technical skills such as tracheostomy care, enteral nutrition, tube feeding and pain management, which can increase the challenges of caregiving. These responsibilities contribute to high CGB, emotional distress, physical strain and social disruption.[8]
In a study comparing the CGB of HNM and other types of malignancies, CGB was found to be higher for patients with HNM than for those with breast or ovarian cancer.[9] With the rise in the number of HNM patients, the CGB of their caregivers is increasingly being recognised and needs to be studied and attended to.
The entirety of caregiving experience and CGB is heavily influenced by social factors, culturally-justified ideologies and religio-spiritual traditions. Spirituality, as understood by modern psychology, is a multilevel and multidimensional construct, which provides meaning and purpose to life. Spiritual well-being (SWB) is a feeling of one’s contentment. It has been defined by the National Interfaith Coalition on Aging as ‘the affirmation of life in a relationship with God, self, community and environment that nurtures and celebrates wholeness’. Spirituality encompasses multidimensional connectedness and provides meaning and purpose to life.
Many researches have shown that people who are more spiritual have better mental health and adapt more quickly to health problems compared to those who are less spiritual.[10] They demonstrate positivity about their roles and communicate better when caring for their patients. Several studies have shown that social support, economic security and faith improve quality of life (QoL), and religious and spiritual functions improve QoL, physical health, hope and general satisfaction with life.[11,12] However, such associations are much less studied in caregivers of head-and-neck cancer patients. There are studies assessing the CGB and SWB in conditions such as thalassemia, neurodegenerative disorders, breast cancers and palliative conditions.[13-16] However, assessment of CGB in caregivers of HMN is seldom reported. The present study was undertaken to identify the association between SWB and CGB in caregivers of patients with HNM, which is an important, yet relatively unexplored area of research.
MATERIALS AND METHODS
Study design and setting
This cross-sectional study was conducted in the inpatient and outpatient Department of Otorhinolaryngology and Head and Neck Surgery, at a rural medical college in Gujarat, Western India. Caregivers who fulfilled the inclusion criteria and voluntarily agreed to participate in the study constituted the study sample.
Sample size
60 caregivers.
Sampling method
The selection was based on a convenient sampling method. The participants were enrolled in the study based on their availability and willingness to participate, ensuring that they met the inclusion criteria specified by the researchers. This approach was selected because it allowed us to access the target population efficiently within the time constraints and resources.
Inclusion criteria
(i) Caregivers looking after patients with HNM admitted/coming for follow-up at the department (ii) Caregivers who can communicate in Gujarati.
Exclusion criteria
(i) Paid caregivers, (ii) Minor caregivers (<18 years), (iii) Caregivers not living with the patient, (iv) Caregivers of patients with ocular and dermatological malignancies of the head-and-neck region (as it is not dealt with by the department of otorhinolaryngology and head and neck). The rationale behind exclusion criteria i, ii and iii emphasises that a caregiver who is not a first- or second-degree relative may lack the same level of attachment as a close relative residing with the patient, even if the latter has their own social and professional obligations.
Ethics committee approval
The research proposal was approved by the Institutional Ethics Committee; IEC Approval no: IEC/BU/2023/Ex. 21/117/2023.
Data collection and study tools
Data were collected using the participant information form consisting of demographic and disease-related section, CGB scale and SWB scale. CGB was assessed using the Zarit Burden Interview (ZBI) and SWB was assessed using the SWB Assessment Scale.
Revised ZBI (Official Distribution – Mapi Research Trust – PROQOLID. 2021):[17] The revised version contains 22 items. Each item on the interview is a statement, which the caregivers are asked to endorse using a five-point scale. Response options range from 0 (Never) to 4 (Nearly Always). Interpretation of ZBI scores was as follows: 0–21 indicating little or no burden, 21–40 indicating mild-to-moderate burden, 41–60 indicating moderate-to-severe burden and 61–88 indicating severe burden. Gujarati translation with linguistic validation was acquired and used following permission.
-
SWB assessment scale:
The SWB SWBS is composed of twenty items and measures two dimensions of SWB.[18,19] The Religious Well-Being (RWB) Subscale provides a self-assessment of one’s relationship with God, while the existential well-being (EWB) Subscale gives a self-assessment measure of one’s sense of life purpose and life satisfaction. Each item is answered on a 6-point Likert scale ranging from ‘strongly agree’ (1) to ‘strongly disagree’ (6). Eight items were worded in a reverse direction and were reversely scored. The overall score from the SWBS is computed by summing the responses to all twenty items after reversing the negatively worded items. It ranges from 20 to 120, with a higher score representing greater SWB. Gujarati translation of SWBS was carried out by the experts using the translation-back translation method and was validated (0.803 Scale Content Validity Index [S-CVI]). Two components of SWB were EWB which measured one’s level of life satisfaction and life purpose and RWB which measured how one views their relationship with God. It reflects one’s sense of satisfaction and positive connection with God.
Tool administration
The patient and their caregivers were informed about the study, and those who voluntarily agreed to participate were enrolled. Written informed consent was obtained from each caregiver before participation. Subsequently, participants were provided with a hard copy of a combined form, which included sections for demographic details of both the patient and caregiver, disease-related information and two standardised questionnaires: (i) The Revised ZBI and (ii) the SWB Assessment Scale. The form was designed to be self-administered by the participant, with the researcher present throughout to address any questions or provide clarifications as necessary. Additional information, such as cancer staging and specific treatment details, was retrieved and recorded by the researcher directly from the patient’s medical records.
RESULTS
Of the 60 caregivers interviewed, the majority were males (61%), married (85%), from rural areas (60%) and resided in joint families (76%). The mean age of the respondents was 44.3 years (standard deviation [SD] = 14.9) and ranged from 21 to 72 years. The detailed demographic profile of the study participants is given in Table 1:
Malignancy wise distribution of patients has been given in Figure 1. The mean duration of the disease was 7.25 months (SD = 7.87) ranging from 1 to 40 months.
| Demographic profile | Variable | Number, (%) |
|---|---|---|
| Gender | Male | 37 (61.66) |
| Female | 23 (38.33) | |
| Marital Status | Married | 51 (85) |
| Unmarried | 9 (16) | |
| Residence | Rural | 36 (60) |
| Urban | 24 (40) | |
| Type of family | Joint | 46 (76.66) |
| Nuclear | 14 (23.23) | |
| Educational status | Graduate and above | 19 (31.66) |
| Undergraduate | 22 (36.66) | |
| Primary and above | 19 (31.66) | |
| Occupation | Homemaker | 13 (21.66) |
| Skilled | 22 (36.66) | |
| Semiskilled | 18 (30) | |
| Others | 07 (11.66) |
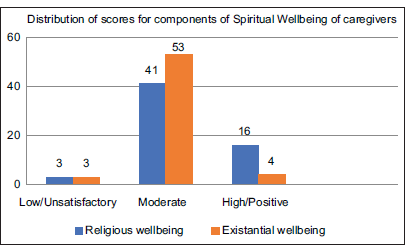
- Distribution of score for components of spiritual wellbeing of caregivers.
SWB
The mean SWB score amongst caregivers was 81.70 (SD = 14.84). Most caregivers (56, 93.3%) exhibited moderate levels of SWBS. The distribution of SWBS among study participants is shown in Table 2.
| Spiritual wellbeing score | No of participants (%) |
|---|---|
| Low (0–40) | 01 (1.7) |
| Moderate (41–99) | 56 (93.3) |
| High (100–120) | 03 (5) |
The SWBS consists of two components:
EWB: This measures life satisfaction and purpose. EWB scores were classified as low ( less than 20), moderate (21-40) and high (more than 40).
RWB: This assesses one’s sense of satisfaction and connection with God. RWB scores were classified as unsatisfactory (less than 20). moderate ( 21-40) and positive (more than 40). The distribution of EWB and RWB is given in Figure 2.
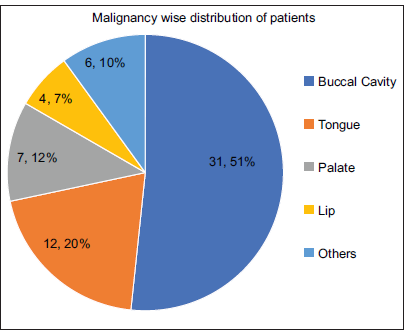
- Malignancy wise distribution of patients.
CGB
The mean CGB score (CGBS) was 35.30 (SD = 11.25). Most caregivers (40, 66.6%) reported mild-to-moderate levels of CGBS. The distribution of CGB scores among participants is detailed in Table 3.
| CGB score | No of participants (%) |
|---|---|
| Little or no burden (0–20) | 3 (5) |
| Mild to moderate (21–40) | 40 (66.7) |
| Moderate to severe (41–60) | 15 (25) |
| Severe (61–88) | 2 (3.3) |
CGB: Caregiver burden
Correlations between SWB and CGB
A significant negative correlation was observed between SWB and CGB [Figure 3]. The Pearson correlation test yielded an R-value of −0.769 (R2 = 0.591, P < 0.01), indicating that higher SWB scores were associated with lower CGB scores. Further analysis showed significant negative correlations between the CGB, RWB, and EWB components of SWBS. The R-value was −0.599 and −0.702, respectively [Table 4].
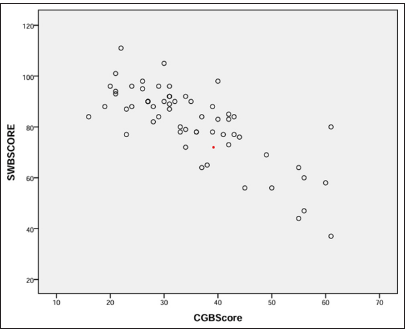
- Pearson correlation between Spiritual well being (SWB) score and caregiver burden (CGB) score among the caregivers of head and neck malignancy patients. A negative correlation was found between the two domains. With R value -0.769.
| CGB1 | SWB2 | EWB3 | RWB4 | |
|---|---|---|---|---|
| CGB | − | −0.769 | −0.702 | −0.599 |
| SWB | −0.769 | − | 0.872 | 0.852 |
| EWB | −0.702 | 0.872 | − | 0.496 |
| RWB | −0.599 | 0.852 | 0.496 | − |
CGB: Caregiver burden1, SWB: Spiritual wellbeing: EWB: Existential wellbeing3and RWB: Religious wellbeing4
Observations on demographical points
CGB demonstrated a direct relationship with nuclear families and an inverse relationship with individuals from urban areas and those who are unmarried, although these findings were not statistically significant. Similarly, SWB showed a direct relationship with individuals from urban regions and married persons, while an inverse relationship was observed with individuals from nuclear families. However, these relationships were also not statistically significant.
DISCUSSION
It is imperative to study the factors which affect caregiving and modulate it to improve the health of patients and caregivers. This study is one of the few investigations to use standardised assessment tools to examine the relationship between CGB and SWB in HNM patients. Based on our results, SWB emerged as a critical factor in mitigating CGB evidenced by the significant inverse relationship between CGB and SWB (R: −0.769). This suggests that higher levels of SWB are associated with lower levels of CGB. Despite limited studies comparing SWB and CGB in HNM caregivers, our findings are supported by previous research conducted in other clinical conditions, indicating that SWB can enhance coping mechanisms, provide a sense of purpose and reduce psychological distress amongst caregivers.[16,19-21]
Relationship between CGB and SWB
Türkben Polat et al., have reported a negatively significant relationship between CGB and SWB in caregivers of patients with breast cancer. They further observed that CGB in female caregivers was significantly higher than that in male caregivers.[15] In a study of 178 family members of patients admitted to palliative care word in Brazil, there is an inverse correlation between the Zarit score and all the World Health Organisation Quality Of Life- Spirituality, Religiousness And Personal Beliefs (WHOQOL-SRPB) facets, indicating that the lower the spirituality, the greater the emotional burden.[16] In a study of patients with neoplastic brain tumours, it was found that caregivers with low levels of spirituality were at higher risk of high CGB, anxiety and stress.[22]
The above studies suggest a potential connection between an individual’s spiritual health and a reduced CGB in the respective cohorts. They further underline the importance of assessing spiritual beliefs and practices for providing resources that promote SWB for comprehensive care.[23,24]
Studies further show that caregivers who experience low SWB have a poorer QoL and more problematic intrapsychic aspects of personality, such as low acceptance of their own emotions and failure to be in contact with their own feelings.[21,25] Individuals with higher SWB are found to have lower depressive symptoms, lesser personality disorders and lesser CGB.[26,27] Spirituality helps family caregivers to avoid emotional problems, be satisfied, feel strong and peaceful; find the meaning of their caregiver roles, as well as cope with their sadness and losses.[28,29]
Factors influencing caregiving process
The caregiving process is influenced by diverse factors. Cultural context shapes the entirety of the caregiving experience. Culturally-justified ideologies about roles, responsibilities and religio-spiritual traditions shape the caregiving process. Specific factors influencing CBG include age, gender, type of family, occupation, education, income and personal health conditions of caregivers themselves.
However, no meaningful associations of CGB and/or SWB with other variables such as age, gender, occupation, education, type of family or duration of the disease were observed in the present study. Our study finds no significant association between the duration of illness and SWB or CGB. However, the results showed some improvement in SWB and reduction in CGB as the time progressed which was supported by Pearson correlation −0.208 and 0.164, respectively.
Ross et al. have found no significant correlation between results of disease duration and gender with unmet psychological health needs.[30] Caregivers have also shown a trend towards increased burden and worsened QoL at higher disease stages, with higher perceived social support associated with lower burden and higher QoL.[31] In a study of selected social and social psychological factors that are associated with perceived CGB of the elderly in northern India, Gupta et al. found that male caregivers’ perceived burden depends only on the size of the role overload and female caregivers’ perceived burden depends on the interrelationship between the size of the role overload and adherence to Asian cultural norms.[32] In a study of CGB in patients receiving haemodialysis, Rafati et al., reported that CGB was moderate/severe. In addition to showing a significant reveres relationship between CGB and SWB scores, they demonstrated that the patient’s income, frequency of patient dialysis per week and patient’s need to receive care and SWB were predictors of CGB, which explained 41% of the burden in caregivers.[33] These findings underscore the complex and multifaceted nature of CGB, influenced by various factors in different contexts and the ability of an individual to resist against the odds.
Exploring the subparameters of the SWB scale, i.e. RWB and EWB both showed inverse relations with CGB with Pearson correlation of −0.599 and −0.702, respectively. The role of both parameters was nearly equal in determining the overall SWB of the caregiver with Pearson correlation of 0.852 and 0.872, respectively.
It is said that in moments of grief, an individual turns to existential truths to seek solace in suffering. Despite the evidence-based importance of SWB and the recognition of spirituality as a dimension of health by the World Health Organization, it seems that spiritual care remains insufficiently addressed by the medical system.[34] A study conducted by Camargos et al., suggests that not only the patients but also healthcare professionals consider spirituality an important component of a holistic approach and having been practising certain spiritual/religious practices has helped them face problems.[35] It is well known that individuals diagnosed with cancer often turn to their religious faith or deeply rooted spiritual beliefs/practices for palliation and seeking meaning and purpose in life and its vicissitudes. The satisfaction received from their connection with a divine power, and EWB, enriches the sense of understanding about the purpose and meaning of life and enhances coping strength.
Strengths and limitations
This study is one of its kind in assessing the two complex parameters among the caregivers of HNM patients. The results of this study have consolidated the role of spirituality in healthcare and highlighted the utmost need to assess and provide spiritual care needs. There are a few limitations of the present study. Ours was a cross-sectional study with a limited sample size. Since socioeconomic status, cultural differences and within-group variability may confound any research findings on CGB, it would be difficult to determine how each of these factors impacts the caregiving experience and hence limit its generalisability. Moreover, we could not assess an individual’s CGB and SWB with the progression of the disease owing to the cross-sectional nature of the study, which has the potential to indicate a direction in providing effective spiritual care.
CONCLUSION AND RECOMMENDATIONS
This study is one of its kind in assessing the two complex parameters (CGB and SWB) among the caregivers of HNM patients. Our study shows that 95% of caregivers demonstrate moderate-to-high SWB irrespective of diverse educational, social and family backgrounds. Most caregivers (66.6%) reported mild-to-moderate levels of CGBS. Higher SWB seems to be leading to lower CGB. Our study did not show any significant effect of sociodemographic variables such as age, sex, education, occupation, income and type of family on CGB.
Based on the results of the study, the following recommendations can be made:
Incorporation of spiritual care into the routine assessment and support of caregivers of patients with HNM can help widen the paradigm of care. Identification of and enhancement of SWB of caregivers should be considered and can be included as standard operating protocols for these patients.
Further longitudinal studies should be conducted to explore the impact of SWB on CGB in different populations and settings. Institutionalising policies for the training of healthcare providers can help to pursue these recommendations.
Acknowledgement
The authors wish to acknowledge the Dean of the institute for all the support. This study was presented at the 9th European Conference on Religion, Spirituality and Health in May 2024 at Salzburg, Austria.
Ethical approval
The research/study was approved by the Institutional Ethics Committee at HM Patel Centre for Medical Care and Education, Bhaikaka University, Karamsad, Gujarat, number IEC/BU/2023/Ex.21/117/2023, dated April 19th, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Caregiver Burden: A Concept Analysis. Int J Nurs Sci. 2020;7:438-45.
- [CrossRef] [PubMed] [Google Scholar]
- Caring for a Loved One with Advanced Cancer: Determinants of Psychological Distress in Family Caregivers. J Palliat Med. 2006;9:912-21.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of an Interaction-skills Training for Reducing the Burden of Family Caregivers of Patients with Severe Mental Illness: A Pre-posttest Design. BMC Psychiatry. 2018;18:84.
- [CrossRef] [PubMed] [Google Scholar]
- The Burden of Care and the Understanding of Disease in Parkinson's Disease. PLoS One. 2019;14:e0217581.
- [CrossRef] [PubMed] [Google Scholar]
- Head and Neck Cancer Burden in India. Int J Head Neck Surg. 2013;4:29-35.
- [CrossRef] [Google Scholar]
- Cancer Statistics, 2020: Report from National Cancer Registry Programme, India. JCO Glob Oncol. 2020;6:1063-75.
- [CrossRef] [PubMed] [Google Scholar]
- Distress in Spouses and Patients after Treatment for Head and Neck Cancer. Laryngoscope. 2007;117:238-41.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers and Strategies in Implementation of Oral Care Standards for Cancer Patients. Support Care Cancer. 2003;11:435-41.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer Patients' Diagnosis and Symptoms and Their Family Caregivers' Self-efficacy and Social Support Are Associated with Different Caregiver Reactions. Eur J Cancer Care. 2020;29:e13311.
- [CrossRef] [PubMed] [Google Scholar]
- Religion, Spirituality, and Health: The Research and Clinical Implications. ISRN Psychiatry. 2012;2012:278730.
- [CrossRef] [PubMed] [Google Scholar]
- A Systematic Review of Associations between SWB and Quality of Life at the Scale and Factor Levels in Studies among Patients with Cancer. J Palliat Med. 2015;18:286-98.
- [CrossRef] [PubMed] [Google Scholar]
- The Relationship between Spiritual Well-being, Mental Health, and Quality of Life in Cancer Patients Receiving Chemotherapy. J Family Med Prim Care. 2019;8:1701-5.
- [CrossRef] [PubMed] [Google Scholar]
- Caregiver Burden, Spirituality, and Psychological Well-Being of Parents Having Children with Thalassemia. J Relig Health. 2016;55:941-55.
- [CrossRef] [PubMed] [Google Scholar]
- SWB and CGB in Alzheimer's Caregivers. Geriatr Nurs. 2005;26:154-61.
- [CrossRef] [PubMed] [Google Scholar]
- SWB and Care Burden in Caregivers of Patients with Breast Cancer in Turkey. J Relig Health. 2023;62:1950-63.
- [CrossRef] [PubMed] [Google Scholar]
- Spirituality Alleviates the Burden on Family Members Caring for Patients Receiving Palliative Care Exclusively. BMC Palliat Care. 2020;19:77.
- [CrossRef] [PubMed] [Google Scholar]
- 2021. Available from: https://www.eprovide.mapi/trust.org/instruments/zarit-burden-interview [Last accessed 2024 Sep 21]
- Loneliness, SWB and the Quality of Life In: Peplau LA, Perlman D, eds. Loneliness. A Sourcebook of Current Theory Research and Therapy.. New York: Wiley; 1982. p. :224-37.
- [Google Scholar]
- Examining the Relationship between Fear of COVID-19 and Spiritual Well-being. Spirit Psychol Counsel. 2020;5:341-54.
- [CrossRef] [Google Scholar]
- Exploring the Associations between Spiritual Well-being, Burden, and Quality of Life in Family Caregivers of Cancer Patients. Palliat Support Care. 2019;17:294-9.
- [CrossRef] [PubMed] [Google Scholar]
- SWB Associated with Personality Traits and Quality of Life in Family Caregivers of Cancer Patients. Support Care Cancer. 2018;26:2633-40.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring Spirituality in Family Caregivers of Patients with Primary Malignant Brain Tumors Across the Disease Trajectory. Oncol Nurs Forum. 2013;40:E119-25.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative Care Experience in the Last 3 Months of Life: A Quantitative Comparison of Care Provided in Residential Hospices, Hospitals, and the Home from the Perspectives of Bereaved Caregivers. Am J Hosp Palliat Care. 2018;35:456-63.
- [CrossRef] [PubMed] [Google Scholar]
- Spirituality, Religiosity, and Spiritual Pain among Caregivers of Patients with Advanced Cancer. Am J Hosp Palliat Care. 2013;30:455-61.
- [CrossRef] [PubMed] [Google Scholar]
- Associations between Faith, Distress and Mental Adjustment: A Danish Survivorship Study. Acta Oncol. 2013;52:364-71.
- [CrossRef] [PubMed] [Google Scholar]
- Spirituality, Sense of Coherence, and Coping Responses in Women Receiving Treatment for Alcohol and Drug Addiction. Eval Prog Plann. 2008;31:113-23.
- [CrossRef] [PubMed] [Google Scholar]
- The Effects of Religiosity on Psychopathology in Emerging Adults: Intrinsic Versus Extrinsic Religiosity. J Relig Health. 2014;53:1529-38.
- [CrossRef] [PubMed] [Google Scholar]
- Spiritual Care from the Perspective of Family Caregivers And Nurses in Palliative Care: A Qualitative Study. BMC Palliat Care. 2023;22:161.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological Impairments Burden and Spirituality in Caregivers of Terminally Ill Cancer Patients. Eur J Cancer Care. 2018;27
- [CrossRef] [PubMed] [Google Scholar]
- Psychosocial Adjustment of Family Caregivers of Head and Neck Cancer Survivors. Support Care Cancer. 2010;18:171-8.
- [CrossRef] [PubMed] [Google Scholar]
- Burden, Quality of Life, and Social Support in Caregivers of Patients Undergoing Radiotherapy for Head and Neck Cancer: A Pilot Study. Chronic Illn. 2016;12:236-45.
- [CrossRef] [PubMed] [Google Scholar]
- Perceived Caregiver Burden in India: Implications for Social Services. Affilia J Women Soc Work. 2009;24:69-79.
- [CrossRef] [Google Scholar]
- Caregiver Burden and Spiritual Well-being in Caregivers of Hemodialysis Patients. J Relig Health. 2020;59:3084-96.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative Care and Spiritual Care: The Crucial Role of Spiritual Care in the Care of Patients with Advanced Illness. Curr Opin Support Palliat Care. 2012;6:269-74.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding the Differences between Oncology Patients and Oncology Health Professionals Concerning Spirituality/Religiosity: A Cross-Sectional Study. Medicine (Baltimore). 2015;94:e2145.
- [CrossRef] [PubMed] [Google Scholar]







