Translate this page into:
Impact of a Longitudinal Intervention to Improve Care Coordination between a Hospital and a Hospice: A Quality Improvement Project

*Corresponding author: Spandana Rayala, Pain Relief and Palliative Care Society, MNJ Institute of Oncology Regional Cancer Center, Hyderabad, Telangana, India. spandanarayala@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rayala S, Palat G, Mathews JJ. Impact of a longitudinal intervention to improve care coordination between a hospital and a hospice: A quality improvement project. Indian J Palliat Care 2021;27(2):216-21.
Abstract
Objectives:
When patients with advanced cancer transition from systemic cancer treatments at MNJ Institute of Oncology to palliative and end-of-life care at a separate stand-alone non-governmental organisation-run hospice facility, there is insufficient transfer of health information, including details of cancer diagnosis and staging, past treatments, imaging reports and goals for future care. Without this information, the hospice care team is not adequately prepared to receive and deliver high-quality palliative care for these patients. This project aims to improve the care coordination between the hospital and hospice.
Materials and Methods:
The measures used are the self-reported confidence score on a scale of 0 to 10 related to knowledge about plan of care among staff who receives patients at hospice at baseline and during and after interventions. Interventions included recognizing the workplace culture and promoting ownership of the tasks, enhancing communication by creating user-friendly transfer forms and on-going assessment of the process.
Results:
Improvement in the care coordination in terms of communication of patient goals of care, from hospital to hospice.
Conclusion:
QI project and the steps involved helped the team to work towards solutions objectively. Seemingly excellent ideas may not be the most impactful and data collection demonstrates this and helps identify the most successful interventions.
Keywords
Care coordination
Confidence score
Ownership
INTRODUCTION
MNJIO and RCC is a public tertiary Cancer Centre located in Hyderabad and caters to the cancer patients in the catchment area with a population of approximately 100 million. The palliative care needs are huge as most of the patients present in the advanced stages of the disease. A Non-Governmental Organisation Hospice which is located 15 km away from the hospital caters to all the hospice needs of the patients from the centre. The outpatient team in the hospital refers the patients to the team in the hospice for control of difficult symptoms and end of life care. Referral system is through paper which also includes photocopies of treatments given and copies of imaging reports which the family takes and presents to the treating team in hospice. The hospice transfer forms are filled up by the doctor, the nurse and the counsellor at the hospital and this form are sent with patient to hospice. In addition, phone calls are made between doctors, nurses and counsellors regarding each hospice transfer. Several challenges resulting in compromised patient care are found in this system of care transition. It is found that the hospice transfer form is often inadequately filled and the phone calls do not always happen. This system of referral makes information transfer erratic, unreliable and incomplete and also makes it difficult for the hospice team to provide timely and holistic support to the patients. Since many transitions are urgent and unplanned, patients and their families are largely unprepared for what transpires and are often uncertain about the roles of different stakeholders.[1] Another factor contributing to the challenges of care transition is the lack of a single clinician or clinical entity taking responsibility for coordination across the continuum of the patient’s overall healthcare, regardless of setting.[1] Separate care team and paper medical records are maintained in each facility, leading to gaps in continuity of care related to goals of care, when patients transition from one facility to another.
Continuity, coordination and transitions of care are key domains for improving quality of care for patients with advanced and serious illness. These three concepts are key standards for quality palliative care[2] and key determinants of satisfaction with care for patients at the end of life.[3,4] Proper transfer of accurate, relevant data about diagnostic findings, treatment, complications, consultations, tests pending at discharge and arrangements for post-discharge follow-up may improve the continuity, coordination and transition of care.[5,6] Despite the availability of these performance standards, the extent to which physicians successfully transfer timely and accurate patient information at hospital discharge is often inadequate and uncertain.
The aim of our QI process is to make sure the treating team in hospice has all the required information when the patient reaches hospice to take appropriate medical decisions.
MATERIALS AND METHODS
There is evidence to suggest that dissatisfaction among health-care providers occurs due to infrequent direct communication between hospital physicians and primary care physicians during the discharge process.[7-9] Therefore, to measure the impact of our QI intervention, we defined a provider-reported confidence score on a scale of zero to ten.
The primary measure was the confidence score on a scale of 0–10 from the hospice doctor who would report how confident they were about the plan of care for the patient who had just transitioned from hospital to hospice. The secondary measure was the confidence score reported by the hospice counsellor. We felt this would be a direct measure of how close or how far we were from our goal: which was improved care coordination when a patient was transitioned from hospital-based palliative care to hospice. We wanted to get the input of nurses also, but since the nurses at hospice receiving patients kept changing depending on the shifts, we decided to restrict data collection to the fixed staff-doctor and counsellor.
Data were collected from January to May 2018. After each hospice transfer one of the study investigators called the hospice doctor and counsellor and asked them to score their level of confidence regarding making a clear plan of care for that patient. The confidence scores reported by the doctor and the counsellor were plotted against the dates on which hospice transfers occurred [Figure 1].
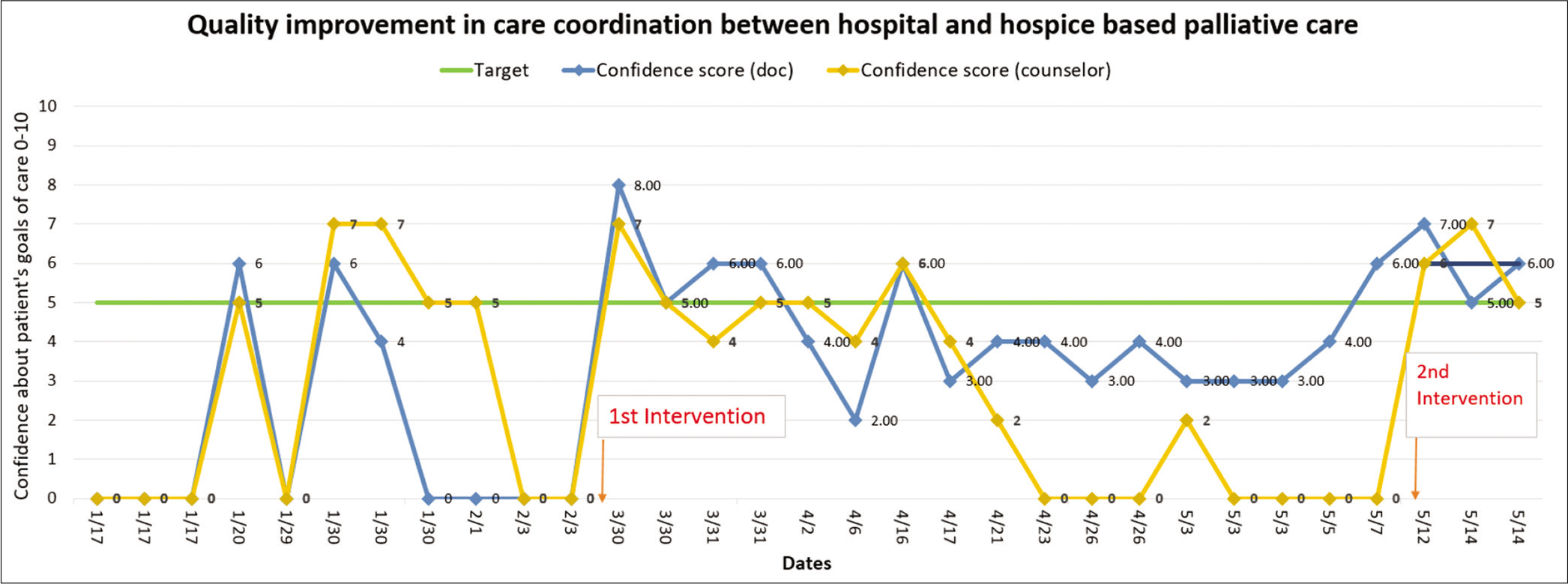
- Run chart.
Baseline data were collected between January and March. It revealed baseline mean of primary measure was 1.5 out of 10. We defined the target improvement as mean of primary measure equal to or greater than 5.0 by May 2018.
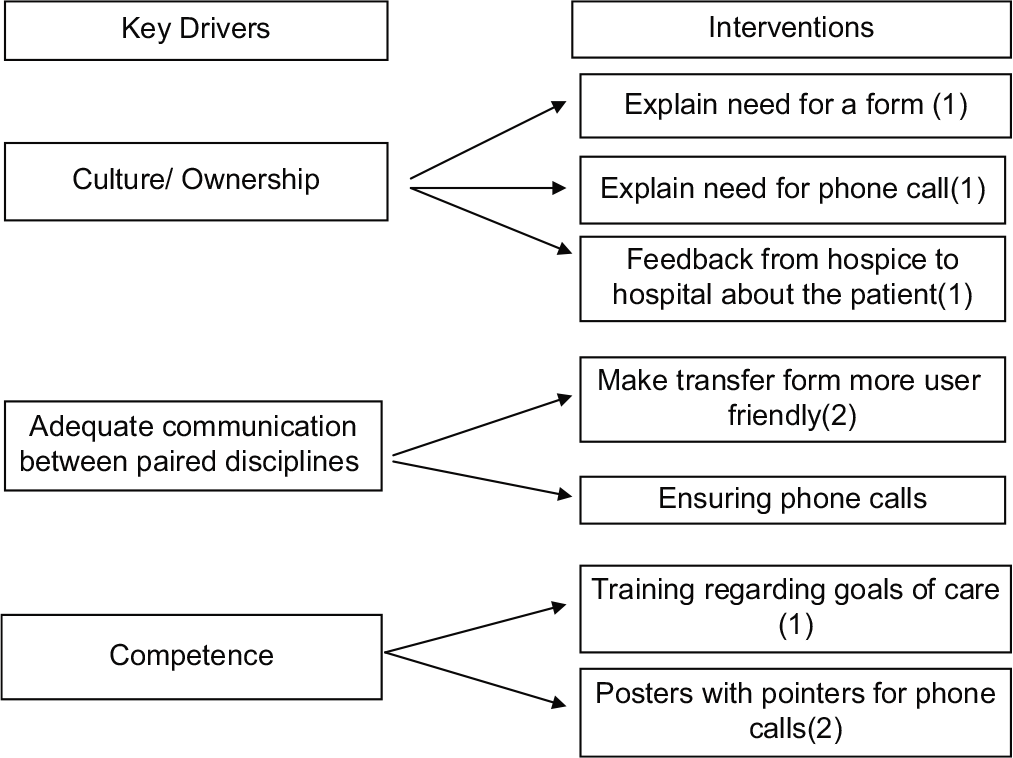
To explore the problem further, we performed a GEMBA walk at the hospital and hospice at the time of patient transfer. We identified the potential points where things could and did go wrong during a transfer that could lead to poor care coordination and plotted those on a fish-bone diagram. For example, we observed that care coordination during hospice transfer depended on a transfer form that was rarely filled out and phone calls between health-care staff at hospital and hospice that was rarely made. Next we did a pareto chart analysis [Figure 2] to find out among all the potential causes which were the most significant and occurred most frequently. We found that 80% of root causes for poor care coordination were due to four events as a result of poor communication, that is, transfer forms being inadequately filled by doctor and counsellor, doctor-to-doctor and counsellor-to-counsellor phone calls not happening. Based on these four root causes, we defined three key drivers, or processes that had to happen consistently for us to achieve the target [Figure 3]. These key drivers, in turn, informed our interventions.
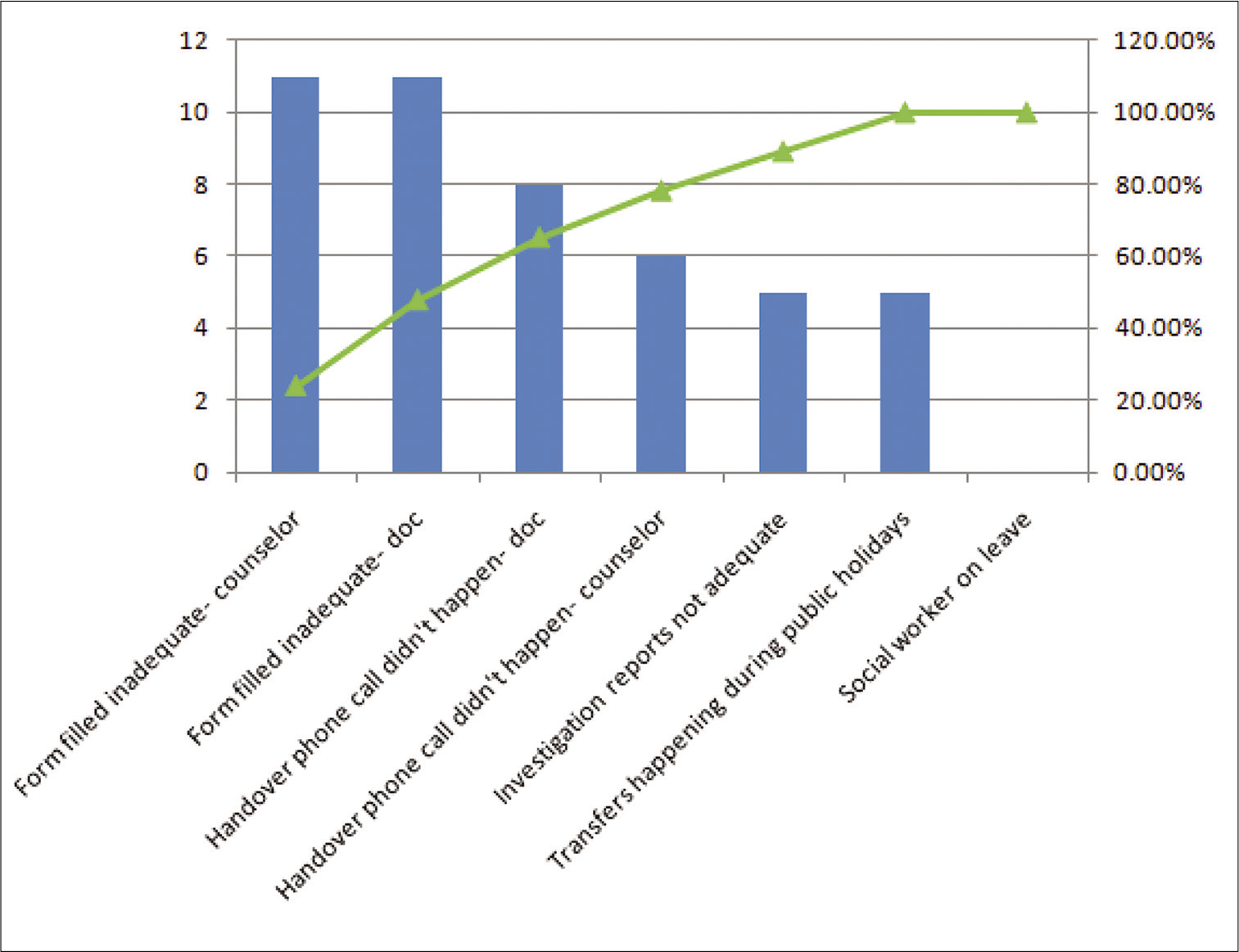
- Pareto chart depicting various contributors.
- Key drivers and interventions.
We realised early on in the analysis that there was a workplace culture issue that would need to be addressed before we made other interventions. The hospital team felt that once the patients were planned for hospice transfer that it was no longer their concern. They felt the hospice transfer forms and phone calls were just extra paperwork for them.
Hence, our first key driver was building a culture of ownership: Making this transfer care coordination relevant and important for the hospital team, making the team understand the need of a completed transfer form and those phone calls. Accordingly, our first intervention was a training session involving all the hospital and hospice staff, in which we explored the current status of care coordination during transfers and the need to improve. During this session, we also invited feedback from staff about how the transfers could be improved.
The second key driver we chose was communication: Specifically between the paired disciplines that is doctor-doctor, nurse-nurse and counselor-counselor communication- through forms and through the calls. We received several inputs from the hospital and hospice teams to make the transfer forms more user-friendly, more tick boxes, involving less writing as they have a busy schedule. We re-worked the transfer forms [Appendix 1] to make them more user-friendly and optimised to meet our target. The third key driver was competence – making sure that all members of the team were equally confident about understanding what was meant by goals of care and what exactly was it that needed to be communicated during the transfer. For this, we planned regular training sessions and readily available resources for the staff.
RESULTS
The initial data collected from the hospice doctor as the confidence score regarding the information received about the individual patients transferred from hospital to hospice showed a mean of 1.5. Following the first intervention of a training session with a feedback from the hospital team there was an immediate demonstrable increase in the confidence score reported above 5, which dipped back to below 5 after few days. The next intervention was making the forms more user-friendly, which led to an increase in the confidence score to around 6.5 at the end of the project.
We noticed that since our counsellor was considerably more experienced and also had the tough job of breaking bad news to the family and prepare them for the progressive deterioration of the health of their loved ones, the confidence score reported was steeply affected.
DISCUSSION
Key learning points
The QI process as a whole helped the team to analyse the steps involved in the process of complete information transfer for the continuity of care of a patient from hospital to hospice. The culture of ownership can be inculcated through team discussions, receiving active feedback and making the team stakeholders in the process. However, that alone is not sufficient to reach a sustainable goal
QI is a continuous process, the end of the project does not mean end of the process
Bringing a change in the system though difficult is possible. The staff at hospice now demands for a properly filled form and for adequate prior communication before transfer as they have seen better clarity in providing required care for a patient.
CONCLUSION
Transitional care is defined as a set of actions designed to ensure the coordination and continuity of healthcare as patients transfer between different locations or different levels of care in the same location. Our QI process helped ensure the smooth transition of patients with high symptom burden between two different facilities. The learning acquired through the team help us not to jump to the obvious solutions alone rather use A3 methodology to zero in on the actual issues and work to find answers.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Lost in transition: Challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141:533-6.
- [CrossRef] [Google Scholar]
- National hospice and palliative care organization (NHPCO) position statement and commentary on the use of palliative sedation in imminently dying terminally ill patients. J Pain Symp Manage. 2010;39:914-23.
- [CrossRef] [Google Scholar]
- RAND-Southern California Evidence-Based Practice Center. A systematic review of satisfaction with care at the end of life: (See editorial comments by Dr. Jean S. Kutner, 160-162) In: J Am Geriatr Soc. Vol 56. 2008. p. :124-9.
- [Google Scholar]
- Abandonment at the end of life from patient, caregiver, nurse, and physician perspectives: Loss of continuity and lack of closure. Arch Intern Med. 2009;169:474-9.
- [CrossRef] [Google Scholar]
- Passing the clinical baton: 6 principles to guide the hospitalist. Am J Med. 2001;111:36-9.
- [CrossRef] [Google Scholar]
- The relationship between general practitioners, hospital consultants and community nurses when caring for people in the last year of their lives. Family Pract. 1991;8:350-5.
- [CrossRef] [Google Scholar]
- Compliance with guidelines for continuity of care in therapeutics from hospital to community. Med J Aust. 2001;174:277-80.
- [CrossRef] [Google Scholar]
- Communications between general practitioners and consultants. Br Med J. 1974;4:456-9.
- [CrossRef] [Google Scholar]
APPENDIX
Appendix 1: Hospice referral form
Patient Name: _______ MNJ Reg. No: _________
Date of Hospice Transfer: ________ In Homecare Program:
□ Yes □ No
Age: ____ Sex: □M □F Address: □ Hyderabad □ Outside Hyderabad □ PSK
Patient phone #: _____ Relative phone #:________
Diagnosis:
Stage of disease: □ Diagnosis □ Acute toxicity
□ Disease recurrence/progression □End of life care Goal of care: □Curative □Symptom control □Improve function
□Respite Care □End of life care
| Tumour-specific treatment received | Last Date | Details |
|---|---|---|
| Chemotherapy | □Curative | |
| □ Palliative | ||
| Radiotherapy | □Curative | |
| □ Palliative | ||
| Site: | ||
| Surgery | Name of_________ | |
| surgery:_______ | ||
| Last Blood/RDP | ||
| Transfusion |
| S. No. | Name | To be Included |
|---|---|---|
| 1 | CBP | □ |
| 2 | LFT | □ |
| 3 | RFT | □ |
| 4 | CXR PA view | □ |
| 5 | CT/PET Scan | □ |
| 6 | Biopsy report | □ |
| 7 | Bone scan report | □ |
| 8 | Other: | □ |
| Palliative care issues | Interventions and doctor’s orders |
|---|---|
| ECOG score: 1 2 3 4 Symptoms: □Pain □Shortness of breath □Fatigue □Nausea/vomiting □Constipation □Depression □Anxiety □Delirium □Drowsiness □Disturbed sleep □Loss of appetite □Diarrhoea Nursing issues □Wound dressing □Oral care □Bed bound patient □Tracheostomy care □Colostomy care □Bleeding wound □Ascitic tapping □Pleural tapping □Nasogastric tube □Foley’s catheter □Lymphedema care □Subcutaneous line care □Physiotherapy □Regular bowel regimen with enema Communication Patient is aware of: □Diagnosis □Prognosis Family is aware of: □Diagnosis □Prognosis |
Rx 1 |
Expected duration of hospice stay:
Other comments from doctor:
Doctor’s name:
Nurse’s Note:
| Medicines Given | Procedures done |
|---|---|
Nurse’s name:
Counsellor’s Note:
Diagnosis and prognosis discussed with (Name and relation to patient):
Issues to be addressed: □Collusion and breaking bad news to patient □Patient fear of pain/suffering □Patient fear of death □Patient has death wish □Body image □Marital life □Worried about children □ Patient angry □Family angry □Patient withdrawn □Social stigma
Other Social issues: □Monthly rations required □Money for last rites □School fees for children □Vocational rehabilitation for dependents □Facility for transport of body □Other: ___
Checklist (to be completed by Counsellor at the end):
Phone Handover: □ Doctor to doctor □ Nurse to nurse □ Counsellor to Counsellor
Investigations included Purpose of admission explained One attendant rule explained Expected duration of hospice stay explained
Any other relevant information:
Counsellor’s name:






