Translate this page into:
Implementation of an Early Palliative Care Referral Program in Lung Cancer: A Quality Improvement Project at the Tata Memorial Hospital, Mumbai, India

*Corresponding author: Dr. Jayita Deodhar, Department of Palliative edicine, Tata Memorial Hospital, Homi Bhaba National Institute, Mumbai, Maharashtra, India. jukd2000@yahoo.co.uk
-
Received: ,
Accepted: ,
How to cite this article: Ghoshal A, Deodhar J, Adhikarla C, Tiwari A, Dy S, Pramesh CS. Implementation of an early palliative care referral program in lung cancer: A quality improvement project at the Tata Memorial Hospital, Mumbai, India. Indian J Palliat Care 2021;27(2):211-5.
Abstract
Objectives:
Access to early palliative care (EPC) for all patients with metastatic lung cancer is yet to be achieved in spite of recommendations. This quality improvement (QI) project was initialized to improve the rates of such referrals from the thoracic oncology clinic for all new outpatients in a premier cancer center in India.
Materials and Methods:
Change in the proportion of patients receiving referrals for EPC during and after intervention (April–May 2018), compared to baseline (January–March 2018) were explored. Interventions included understanding of the process flow, identification of key drivers, and root cause analysis which identified the gaps as lack of documentation for EPC. Teaching and encouraging staff at the clinic to incorporate referrals into all initial visits for patients with metastatic lung cancer were incorporated.
Results:
The bundle of QI interventions increased referrals from an average of 50% to 75%, mean difference = 12.64 (standard deviation = 10.13) (95% confidence interval = 22.01–3.29), P = 0.016 (two-tailed) on paired sample test.
Conclusion:
Improved referral rates for EPC in a multidisciplinary cancer clinic is possible with a QI project. This project also identifies the importance of data documentation and patient information processes that can be targeted for improvement.
Keywords
Early palliative care
Lung cancer
Quality improvement
INTRODUCTION
Over the last few decades, use and acceptance of palliative care (PC) has been growing for the complex care and needs of patients with cancer and their loved ones.[1] There is high quality evidence that early PC (EPC) improves outcomes including survival in metastatic nonsmall cell lung cancer (NSCLC).[2] The factors responsible are increased understanding and acceptance of the care philosophy among oncologists, acknowledging the value of interdisciplinary teams that focus on the whole person care along with the family as the unit of care, and the understanding that the goals of PC align with the priorities of all stakeholders.[3] More patients are receiving PC because the scope of practice has expanded from community-based hospices to inpatient hospitals and the offices of primary care physicians; also, the number of health care professionals seeking specialized continuing education and support to improve PC has increased.[4] Still, this scenario is largely utopian, and globally, PC referrals are not timely but are usually towards end of life.[5] In India, most centers follow isolated PC practice with less importance being given to holistic care.[6] In previous research, the authors noted similar problems even in a premier cancer center in India,[7] and therefore decided to evaluate this aspect of PC, design a bundle of interventions to improve this and quantify the improvement. They resorted to a quality improvement (QI) activity aimed to clarify how care is delivered and how care might be enhanced through realistic and sustainable interventions.[8] QI rely on data collection and analysis to understand broader patterns across health-systems, whether for program development, reimbursement, health services research, or quality assessment.[9]
This article focusses on the efforts to improve the quality of the referral process for EPC for patients with advanced lung cancer in a tertiary cancer center. A previous pilot study in the same center, looking into the feasibility of introducing EPC in lung cancer showed that out of all the patients referred for PC from lung cancer clinic, only 48% could complete 50% of the planned follow-up visits over a period of 6 months with PC clinic.[7] EPC was chosen specifically because it has the potential to impact overall survival by directly affecting well-being and experience of suffering, increasing social support, improving understanding of illness and informing decision making, less aggressive care at the EOL and earlier referral to hospice.[10]
MATERIALS AND METHODS
We researched into quantifying the improvements in EPC referrals in patients with metastatic NSCLC in a large tertiary cancer center in Mumbai between January and May 2018. Our Specific, Measurable, Achievable, Relevant, and Time (SMART) Goals for this QI project was to increase rates of EPC referrals (specific) in patients with advanced (Stage 4) NSCLC discussed in multidisciplinary team (MDT) meetings (relevant and achievable), from existent rates of 50% to 75% (measurable) over a 5-month period from Jan to May 2018 (time-bound). We used the period from January to March 2018 to measure the baseline levels of referral, instituted a bundle of interventions aimed to improve referral and consultation rates thereafter, and measured the proportion of patients referred and seen at the PC clinic during and after the active intervention phase.
Treatment decisions for all newly registered patients with lung cancer are formulated in the Thoracic Oncology Disease Management Group (TDMG) in MDT meetings held twice a week. The working group in this QI project included PC physicians (JKD, AG, AT), oncologists (CA, CSP), and clinic administrative staff. Mentoring and expert advice were provided by SD through the PC-PAICE project. The QI project started with a baseline retrospective chart review of the year 2017 which showed that 70%–80% of patients consulted in TDMG needed PC, but only 50% were referred early in the course of their disease.
Measures
This QI project was done through A3 exercise based on the methodology of PDCA (Plan–Do–Check–Act) – a philosophy from management science that emphasizes goal-oriented and systematic approaches to increase efficiency and reduce delay.[11] We hypothesized that the pilot QI project would increase the rates of EPC referrals in lung cancer, establish standardized referral criteria, and ensure documentation of referral to PC services in patients’ medical records (paper/electronic). We secured electronic medical records (EMR) of every patient we saw in the clinic and retrieved information required for a quality audit. We adopted SMART bound goals to apply theories in QI and efficiency to current practices in the clinic to improve EPC referrals in lung cancers.[12]
The study was conducted in three phases:
-
Preintervention period (January–March 2018)
We collected data on baseline referral rates for lung cancer cases who met criteria for EPC (AJCC stages 3 and 4) prospectively by reviewing EMR of patients from the TDMG for a period of 3 months (January 1–March 31, 2018). We followed the Gemba walk/Participant Observation technique to create a Process Map of the TDMG workflow. Next, we did a root cause analysis through Fishbone and Pareto diagrams to understand the key problems for low EPC referrals [Figure 1]. Based on this, we isolated the key drivers and assigned roles for every member in TDMG to it [Figure 2]. The Gemba walk/Participant Observation technique helped to ascertain a root cause analysis which highlighted the key problems for low EPC referrals – lack of information to the staff about EPC services and referral process, and irregular documentation of the referrals when made [Figure 1]. Often the patients must attend to multiple clinics/diagnostic services post TDMG decisions, and they need to be explained clearly about EPC referral and the location of the PC clinic in the hospital. Joint discussions were held, based on which key drivers [Figure 2] were identified and every member of the TDMG was assigned roles.
-
Intervention and postintervention period (since April 2018)
We started sensitizing the TDMG group for EPC referrals from April 2018. This was done through academic sessions directed at the healthcare staff in TDMG outpatient clinics. These sessions were designed to give a clear picture of the QI project and on reasons for referral of patients for EPC, the importance of documentation, details about the PC outpatient clinic and the process of registration and assessment. For a better understanding of the patients, we created handouts in local languages to be verbally explained by staff at the clinic.
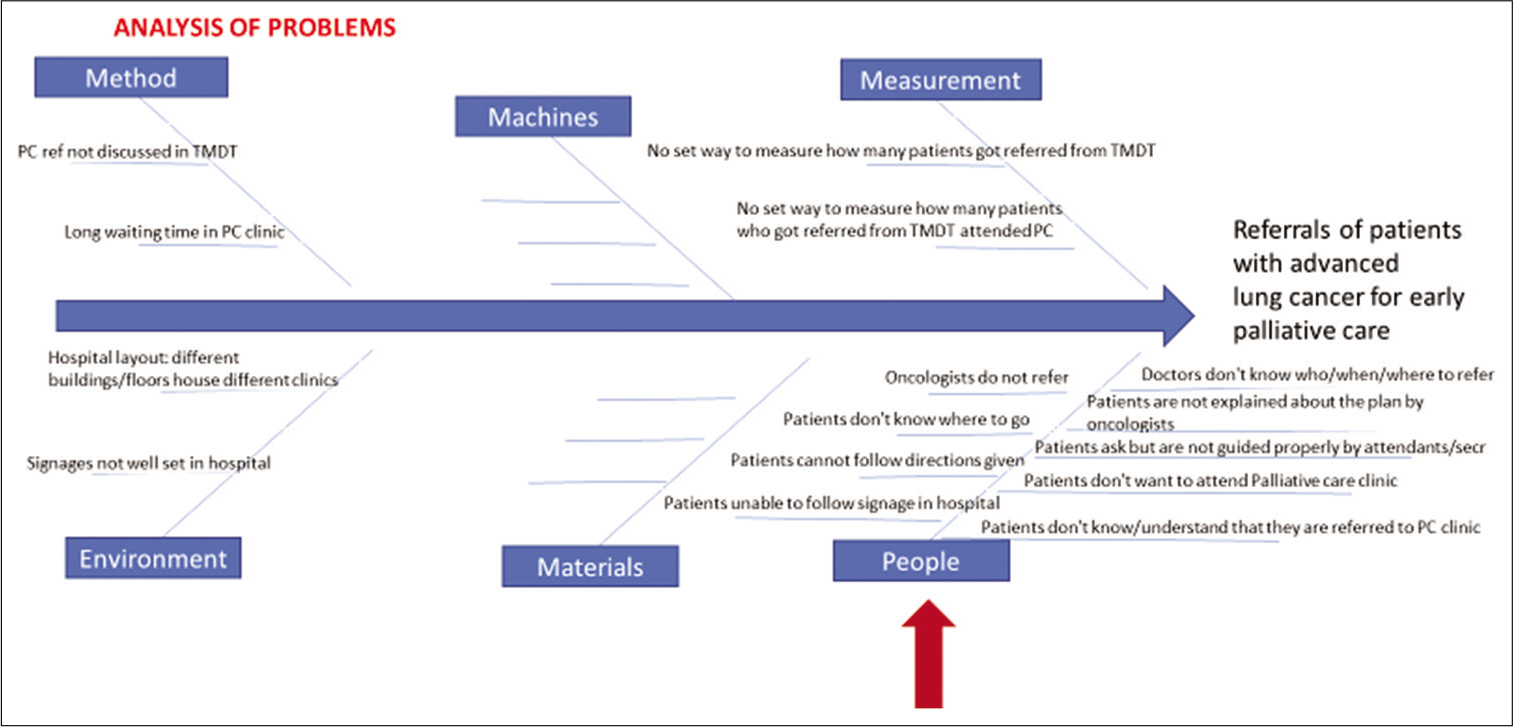
- Fish bone diagram
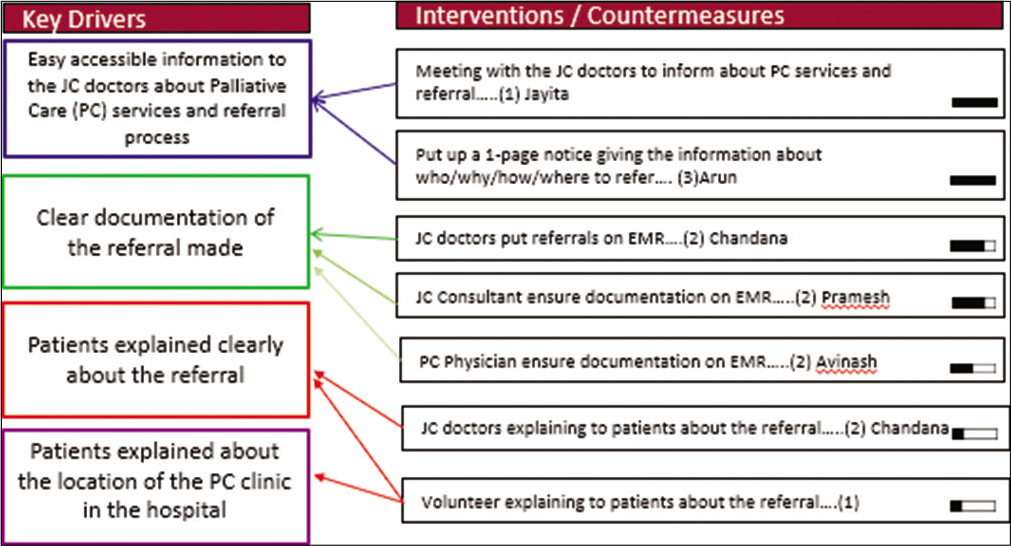
- Key drivers and intervention
Throughout this time, we reviewed EMR weekly to collect data on EPC referral rates from TDMG for patients with lung cancer. Weekly variations were recorded in run charts (data collected till May 2018). These steps were planned to be repetitive and cyclical to sustain the effect of the intervention. Additionally, regular stakeholder feedback was taken in those sessions for continuous improvement of the QI program. No extra costs were involved for the patients or the clinic for program implementation. Formal ethics review was not sought as this was a quality audit, de-identified patient information was used, and the project did not include any confidential individual patient information in the final charts.
RESULTS
The retrospective review of TDMG EMR found that the EPC referral rates for lung cancer were 50% over a period of 1 year (January 1–December 31, 2017). The intervention and postintervention period (since April 2018) saw a gradual rise in EPC referral rates to an average of 75% (range 40%–78%) in the run chart [Figure 3], mean difference = 12.64 (SD = 10.13) (95% confidence interval = 22.01–3.29), P = 0.016 (two-tailed) on Paired samples test. Documentation of EPC referrals improved from 50% pre intervention to 75% postintervention and was sustained thereafter.
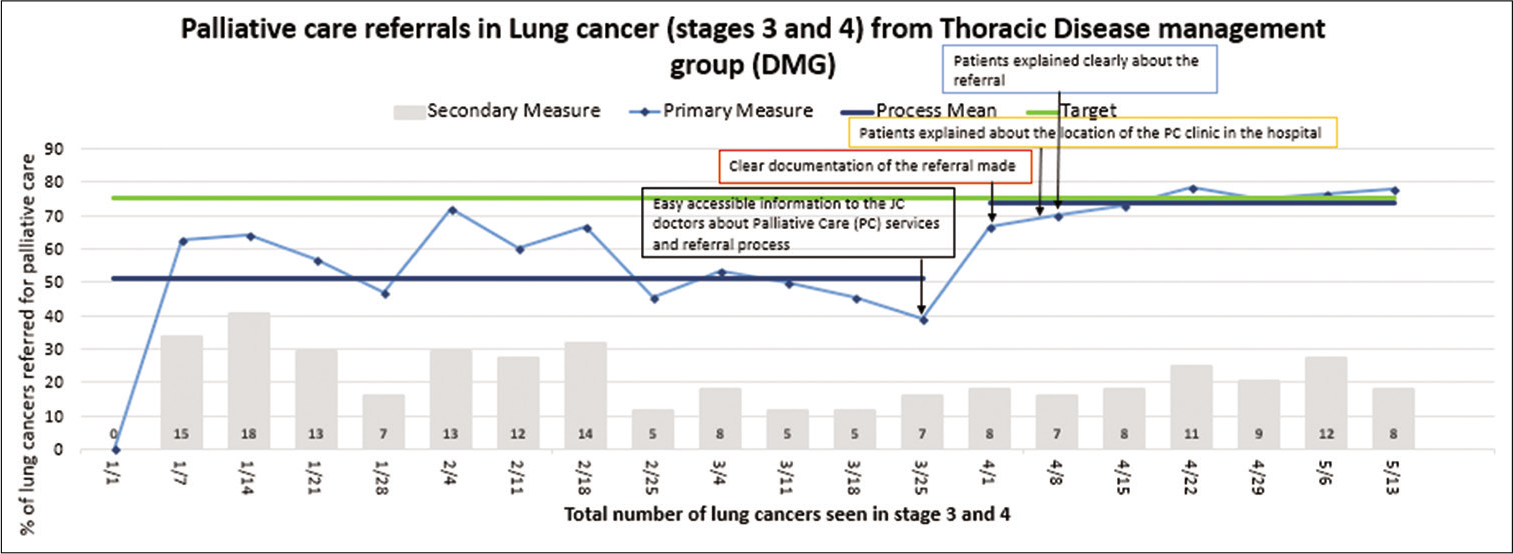
- Run chart
DISCUSSION
Our study showed an improvement in EPC referrals from 50% to 75%. These improvements seemed to be maintained consistently over time. The interventions we used were a bundle of information, education, and care coordination about EPC. These are simple interventions which do not require additional resources or infrastructure. QI initiatives reflect the natural evolution of the evidence base in PC. Use of PC has grown in the last decade, with its roots beginning in the hospice movement in the late 1970s.[13] Administrators, health care professionals, and researchers are beginning to recognize that robust data analytics are crucial for improving patient-and family-centered advanced illness care.[14] Our study demonstrates that a simple bundle of interventions improves utilization of PC services and can be implemented without draining scarce resources.
Such results have been reflected elsewhere in reducing the average time to referral to PC,[15] improving compliance with antiresorptive agents in metastatic breast cancer,[16] and better readiness to quit tobacco prior to treatment with radiation therapy.[17] The quality-improvement and dissemination efforts elaborated in this article were a part of a wider nationwide program as has been described elsewhere.[18] One important, ongoing challenge for new and existing quality-improvement initiatives is how to make the effort as invisible and integrated as possible amid the fabric of usual clinical operations. The seamless integration of validated, quality metric data collection into EMR is ideal but has major cost and time implications. However, overcoming these barriers is crucial to allow for increasingly robust reporting of data, which can then be used to aid PC program development, sustainability, and growth.
Limitations
While this QI project could measure the increase in referral rates from the TDMG/JC meetings, the percentage of referred patients who successfully attended and utilized our PC early is yet to be studied. The postintervention period is one of the most important because it is typical for improvements to fade over time. It is human nature to slip back to previous ways unless measures are put in place to make the solutions permanent. Our study did not measure the sustained effects of this intervention, but the TDMG has been very consistent to maintain the high level for EPC referrals.
Beyond the project
It expanded the scope for PC along with a sound base for collaborative QI activity. The learning from this project was employed for a similar A3 methodology-based QI project in the Psycho-oncology service in the hospital in 2019–2020 to implement a protocol for distress screening and improve screening rates in cancer inpatients. It is likely that such structured problem-solving approaches will provide an objective and systematic method of enhancing quality in healthcare institutions across India. Central to this also will be buy-in from the leadership, identification of a core faculty or team that will be the initiators of change, understanding the need for faculty training and education in QI, measurement of issues to identify key priorities to focus on, and enhanced information systems.
CONCLUSION
Oncologists and PC physicians could employ a QI project successfully to increase referrals for EPC in lung cancers over a period of 5 months. The improvements were achieved without the need for additional resources and can be potentially applied to other oncology units and hospitals. The QI exercise led to better workflow and patient care.
Acknowledgments
Indian Association of Palliative Care, PC: Promoting Access and International Cancer Experience (PC-PAICE) team, Thoracic Oncology Disease Management Group, and administrative staff of Thoracic Oncology and Palliative Medicine out-patients clinic.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Public, patient and carers' views on palliative and end-of-life care in India. Int Nurs Rev. 2018;65:292-301.
- [CrossRef] [Google Scholar]
- Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733-42.
- [CrossRef] [Google Scholar]
- Integrating palliative care into the trajectory of cancer care. Nature Rev Clin Oncol. 2016;13:159-71.
- [CrossRef] [Google Scholar]
- Palliative care in India: Situation assessment and future scope. Indian J Cancer. 2015;52:99-101.
- [CrossRef] [Google Scholar]
- Barriers to accessing palliative care: A review of the literature. Prog Palliat Care. 2014;22:1-19.
- [Google Scholar]
- Provision of palliative care in national cancer grid treatment centres in India: A cross-sectional gap analysis survey. BMJ. 2020;2020:2152.
- [Google Scholar]
- study to assess the feasibility of introducing early palliative care in ambulatory patients with advanced lung cancer. Indian J Palliat Care. 2017;23:261-7.
- [CrossRef] [Google Scholar]
- Basics of quality improvement in health care. Mayo Clin Proc. 2007;82:735-9.
- [CrossRef] [Google Scholar]
- Evidence for the impact of quality improvement collaboratives: Systematic review. BMJ. 2008;336:1491-4.
- [CrossRef] [Google Scholar]
- Early palliative care for adults with advanced cancer. Cochrane Database Syst Rev. 2017;6:CD011129.
- [Google Scholar]
- Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23:290-8.
- [CrossRef] [Google Scholar]
- Be SMART: Examining the experience of implementing the NHS Health Check in UK primary care. BMC Fam Pract. 2015;16:1.
- [CrossRef] [Google Scholar]
- From margins to centre: A review of the history of palliative care in cancer. Lancet Oncol. 2007;8:430-8.
- [CrossRef] [Google Scholar]
- Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technol Forecast Soc Change. 2018;126:3-13.
- [CrossRef] [Google Scholar]
- Implementation of an early palliative care referral program: A pilot study in quality improvement. Palliat Med. 2016;19:1241-2.
- [CrossRef] [Google Scholar]
- Quality improvement in breast cancer project: Compliance with antiresorptive agents and changing patterns of drug use. J Natl Compr Cancer Netw. 2014;12(Suppl 1):S33-5.
- [Google Scholar]
- Quality improvement study to improve assessment of patient readiness to quit tobacco prior to treatment with radiation therapy. Int J Radiat Oncol. 2016;96:E408.
- [Google Scholar]
- PC-PAICE palliative care-Promoting access and international cancer experience in India collaborative (QI717) Pain Symptom Manage. 2019;57:465.
- [CrossRef] [Google Scholar]






