Translate this page into:
Impact of Different Sociodemographic Factors on Mental Health Status of Female Cancer Patients Receiving Chemotherapy for Recurrent Disease
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Deterioration in mental health and poor quality of life (QOL) among women suffering from breast and ovarian cancer is not a direct result of the illness but mediated by many other psychosocial variables.
Aims:
The study intended to examine if there was any effect of educational level, residential status, family type, duration of treatment, and income level of family on anxiety, depression, and QOL among the breast and ovarian cancer patients, undergoing second- or subsequent-line chemotherapy.
Subjects and Methods:
Forty married female cancer patients with breast and ovarian cancer, aging between 40 and 60 years, education level ranges from no formal education to postgraduate degree, income level ranges from Rs. 1000 per month to Rs. 20000 per month, and undergoing second- or subsequent-line chemotherapy for the past 1–10 years were studied. Levels of anxiety and depression were determined by Hospital Anxiety and Depression Scale. The QOL was measured by using WHO QOLBREF scale.
Statistical Analysis Used:
Mean and standard deviation and Levene's F values were calculated. If Levene's F value was significant, then Mann–Whitney U-test was done or else independent samples t-test was used.
Results:
Among all the variables, education, residential status, and income affect significantly on anxiety, depression, and QOL.
Conclusions:
Early detection of psychosocial variables is essential for better screening of the cancer patients undergoing chemotherapy, and therefore, further psychological intervention can be planned accordingly.
Keywords
Chemotherapy
psychosocial variables
quality of life
INTRODUCTION
Breast and ovarian cancer are among the most frequently diagnosed forms of cancers among women in India. Cost-effective methods for early detection of these cancers are necessary.[1] Diagnosis, treatment, and recurrence of breast and ovarian cancers are a challenging experience that might have several impacts on the woman's mental health and their family life.[2345678] The physical restraints of such an illness are undeniable, but the emotional, mental, and psychological changes that take place upon a diagnosis of breast cancer and ovarian cancer loom as well. Every aspect of an individual's life is affected by terminal illness. The fear of reliving all of these experiences with a relapse has made them worry continuously. Considerable research has focused on identifying which subgroups of patients and survivors are at increased risk of experiencing poor psychological health and poor quality of life (QOL). Various predictors have been identified including sociodemographic and clinical factors.[91011] According to various psychosocial models, psychological and sociodemographic factors contribute to the relationship between health and activities of daily life of the person.[12131415] Observation of anxiety and depression associated with diagnosis of ovarian and breast cancer has led to investigations of the potential role of sociodemographic factors.[161718] To provide effective treatment for people suffering from mental health problems, it is critical to identify the barriers that they face when accessing mental health condition.[19] Deterioration in mental health and poor QOL is not a direct result of the illness but are mediated by a plethora of other important psychosocial variables such as education level, socioeconomic status, residential status, financial burden, family type, family support, duration of illness, and many more.
The present study intended to examine if there was any effect of educational level, residential status, family type, duration of treatment, and income level of family on anxiety, depression, and QOL among the breast and ovarian cancer patients undergoing second- or subsequent-line chemotherapy.
SUBJECTS AND METHODS
In the present study, the technique of purposive sampling has been used. Forty married female cancer patients, aging between 40 and 60 years, education level ranges from no formal education to postgraduate degree, income level ranges from Rs. 1000 per month to Rs. 20000 per month, and undergoing second- or subsequent-line chemotherapy for the past 1–10 years were studied between April and October 2016. Among 40 patients, 17 patients were suffering from breast cancer and the remaining had ovarian cancer. Data for the present study have been collected by a registered clinical psychologist under individual administration condition. At first, consent was taken from the patients. Psychological distress was assessed by the Hindi version of Hospital Anxiety and Depression Scale (HADS).[20] According to the scoring system, scores <11 were taken as cutoff for “normal limit” for both anxiety (HADS-A) and depression (HADS-D).[21] QOL of the patients were assessed by WHO QOL-BREF scale.[22] This has four different domains: physical health, psychological, social relationship, and environment. According to the literature, the cutoff score in all domains is 60.[23] Thus, any score below 60 was regarded as poor QOL. Standard scoring procedures were followed. To determine the central tendency and the variability of the scores, the mean and standard deviation were calculated for all participants. To test the significance of difference of mean in terms of duration of treatment, residence, education level, family type, and income level, Levene's F values (df: 38) were calculated. If Levene's F value was significant, then nonparametric statistic Mann–Whitney U-test (df: 38) has been done or else parametric statistic independent samples t-test (df: 38) has been done. Statistical analysis was done using SPSS V20 software (IBM, Armonk, NY, United States of America).
RESULTS
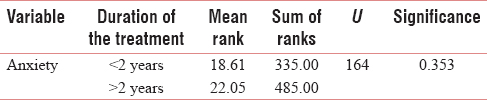
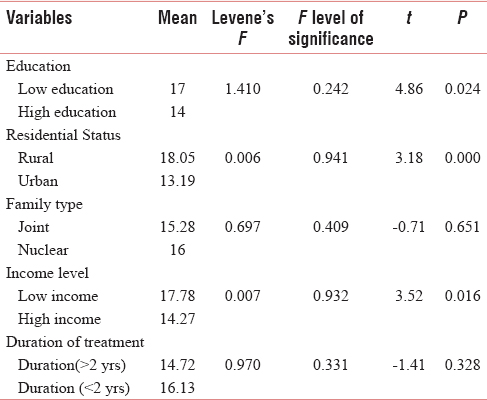
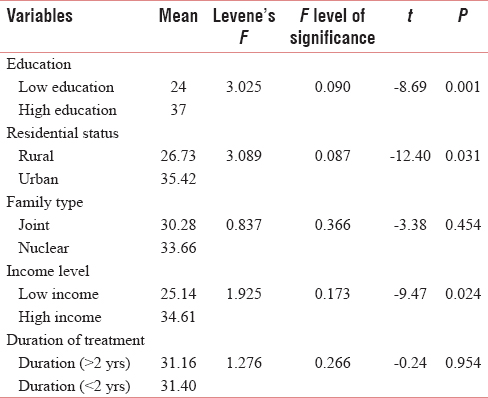
Among 40 patients, 17 patients were suffering from breast cancer and the remaining had ovarian cancer. All breast cancer and 19 ovarian cancer patients were receiving second-line chemotherapy. Four ovarian cancer patients were on the third line of chemotherapy. Out of 40 individuals, 21 were in high education group and 19 were in low education group, persons having education above Class X were considered as high group, and those below were low group. Nineteen individuals were from rural and 21 from urban region. Twenty-two women were in high-income group and 18 were in low-income group; those who have monthly income Rs. 5000 and above were considered as high group. Seventeen persons were from joint family and 23 were from nuclear family type. Twenty-four out of forty women were suffering from the illness for 2 years or more. It can be said that there was a significant effect of educational level on anxiety [Tables 1 and 2], depression [Table 3], and QOL [Table 4] among the patients. There was a significant effect of residential status on anxiety [Tables 1 and 2], depression [Table 3], and QOL [Table 4]. Income level had a significant impact on anxiety [Tables 1 and 2], depression [Table 3], and QOL [Table 4]. However, there was no significant effect of family type on anxiety [Tables 1 and 2], depression [Table 3], and QOL [Table 4] among all the patients. Results on Table 1 revealed that Levene's F value was also significant, showing lack of homogeneity and implying large variations within group. Hence, nonparametric statistics Mann–Whitney U-test has been done to test the significance for anxiety. There was no significant effect of duration of treatment on anxiety [Tables 1 and 2], depression [Table 3], and QOL [Table 4] among the patients undergoing second- or subsequent-line chemotherapy.

DISCUSSION
Breast cancer and ovarian cancer are common cancers among women associated with distressing symptoms.[242526] It is important to take into consideration pain, anxiety, depression, the impairment of cognitive functions, and the QOL, both during and after cancer treatment. If left untreated, anxiety and depression may even be associated with lower survival rates from cancer. Patients often observe emotional, cognitive, and behavioral changes after relapse of the disease that gives rise to increased subjective level of distress, leading to refusal of therapy.[272829] Partners and family members of the patients also face a time of readjustment after diagnosis and treatment of breast and ovarian cancer. Various studies have described the effect of chemotherapy on life and behavior.[30] Psycho-oncology focuses on two important psychological aspects of cancer: psychological, emotional, or behavioral reaction of cancer and various psychosocial contributing factors that may influence the disease progression.[31] The role of psychosocial factors in female cancer patients has been recognized as important since a long time by researchers.[3233] There are many potential psychosocial factors associated with poor mental health and poor QOL in female cancer patients which have been analyzed in the present study.
This study had shown that persons belonging to lower educational group tend to have higher level of depression [Table 3], anxiety [Tables 1 and 2], and poor QOL [Table 4]. From the interview with the patients, it has been revealed that in India, many schools included information regarding cancer and various terminal illnesses as a part of mandatory subject and thus help in spreading awareness among their pupils. The person who does not have higher education gets deprived of these kinds of important social education and thus has less amount of knowledge regarding terminal illness, treatment outcome, and probable recurrence of the disease which might lead to increased inner discomfort, tension, and anxiety. Individuals with low education level might have lower level of confidence that might be a reason of their proneness toward social inhibition and loneliness. Education level is an important indicator of an individual's socioeconomic status and is considered one of the predisposing factors toward the use of mental health-care services.[34] Results of various studies concluded that cancer patients with lower education are more likely to feel unhappy, depressed, and to be tensed or easily irritated, less likely to experience positives mood states, and has inadequate QOL.[3536] The findings of the present study concur well with the above-mentioned studies.
It was seen that rural region group results in higher depression [Table 3], anxiety [Tables 1 and 2], and QOL [Table 4]. Cultural background affects the emotional expression and in many times obstructs the detection and the treatment of depression. The majority of controlled studies reported worse outcomes for rural patients, who appear to have higher needs in the domains of daily living and limited access to resources.[37] Various studies concluded that living in a rural area may mean that individuals must travel long distances to the nearest hospital to get treatment facilities.[3839] The need to travel for treatment caused many practical, emotional, and financial problems for patients and burdened them with additional worry concerning family and work commitments leading to high level of anxiety, depression, and poor QOL.
It was evident from the result that belongs to low-income group associated with higher levels of depression [Table 3], anxiety [Tables 1 and 2], and poor QOL [Table 4]. From the interview, it was found that the majority of the women belong to a family with single earning member. After a diagnosis of cancer, it is important to think about the different types of costs that could add up during treatment and recovery. A long-term illness like cancer requires continuous follow-up, which has made the patient's condition worse. The continuous expense for cancer has coupled with the existing financial problem and has made the present situation very difficult to handle. Depleted financial resources may magnify the impact of a relapse of cancer and it has also made the patient's perceived burden of illness and poor QOL and increases level of depression and anxiety. According to Heilemann et al.,[40] a correlation was found between financial stress and depressive symptoms in patients with cancer. As per various research findings, the severity of psychiatric diseases was reported to be higher among those with a low socioeconomic status.[4142] Sufficient evidence exists to suggest that differences in mental health status, QOL, adjustment, treatment outcome, and survival may be attributable to low socioeconomic status and a lack of insurance coverage.[4344]
We did not get any significant impact of family type on mental health status or QOL. The actual connection between family type and mental health status has been a subject of debate as there are numerous disagreements among researchers. Some of the research findings support the fact that healthy mental state and QOL are associated with joint family,[4546] whereas many other research findings contradicted the aforementioned findings and concluded that healthy mental, emotional, and behavioral states are common among women belonging to a nuclear family.[474849] However, our study was not in accordance. In our study, there are no significant differences in the level of depression, anxiety, and QOL among the patients, living with nuclear or joint family setup. One possible reason for this finding could be that genuine support and nonjudgmental acceptance from the closed one are much more important than the number of family members. Positive mental health and QOL is related to integrity, empathetic reciprocity, and adjustment among family members. From the interview of the present study, majority of the patients reported that their husbands were caring and provide emotional support to them. When considering all the sources of support, patients often identify their husbands or partners as their most important confidant from whom to seek support.[5051]
Duration of treatment does not have any significant impact on mental health status or QOL among cancer patients. One possible reason for this finding could be that the duration of the treatment in the present study was considered to be ranged from 1 to 10 years; because of the vast range, the result could be confounded and other moderator variables (such as socioeconomic status, education, residential status, and personality pattern of the patient) might affect the result. Recurrence of cancer itself is a psychological trauma, and every patient tries to cope with or gets rid of the worry about it. Immediate reactions to cancer can include feelings of vulnerability, sadness, fear, denial, and anger. With the passing of time, such emotions constitute normal coping mechanisms, allowing individuals to come to terms with the implications of their disease gradually and organically. In the present study, patients have the treatment history of at least 1 year, and according to many studies, after a year of disturbance, the patients usually readapt to life and rediscover a certain pleasure in emotional and social relationships and continue to live with it.[5253]
Most of the variables explored in this study are emerging issues in the present-day world which influence female cancer patients highly but are not yet adequately and widely been explored in the Indian culture; there is enough room for future exploration and research on these areas. Larger sample should have been taken which might lead to greater generalization of the findings. The stage of diseases and duration of marriage could not be controlled.
Understanding the factors that contribute to physical or mental illness is very essential as it may help clinicians and all those who participate in community care in preventing, controlling it, or mitigating its impact. However, taking into account the huge number of possibly depressed and anxious persons with poor QOL within breast cancer and ovarian cancer group, it would be beneficial to consider the psychological and social issues as well, so that integrated attention can be given to achieve full benefit of their physical treatment.
CONCLUSION
The present study is concerned both with the effects of breast and ovarian cancer on a woman's psychological health as well as the psychosocial factors that may affect the disease process of cancer and psychophysical outcome of it. It is necessary to find the psychosocial factors (such as low income, low education, and rural background) associated with poor mental health status and poor QOL. Early detection of these psychosocial variables is essential for better screening of the patients who need psychological concerns, so that further psychological intervention and management plan can be prepared accordingly, to help the patient to get back to the normal rhythm of life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank all the female cancer patients attending our institution.
REFERENCES
- Detection of high frequency of mutations in a breast and/or ovarian cancer cohort: Implications of embracing a multi-gene panel in molecular diagnosis in India. J Hum Genet. 2016;61:515-22.
- [Google Scholar]
- Marital adaptation and interaction of couples after a mastectomy. J Psychosoc Oncol. 1993;11:69-82.
- [Google Scholar]
- Breast cancer survivors: Psychosocial concerns and quality of life. Breast Cancer Res Treat. 1996;38:183-99.
- [Google Scholar]
- Relationships in Chronic Illness and Disability. CA, Thousand Oaks: SAGE; 1995.
- Intrusion, avoidance, and psychological distress among individuals with cancer. Psychosom Med. 2001;63:658-67.
- [Google Scholar]
- Couples' adjustment to breast cancer and benign breast disease: A longitudinal analysis. Psychooncology. 1998;7:37-48.
- [Google Scholar]
- Psychological predictors of marital adjustment in breast cancer patients. Psychol Health Med. 2002;7:37-51.
- [Google Scholar]
- Breast cancer surgery: Comparing surgical groups and determining individual differences in postoperative sexuality and body change stress. J Consult Clin Psychol. 2000;68:697-709.
- [Google Scholar]
- Psychiatric morbidity among patients with cancer of the esophagus or the gastro-esophageal junction: A prospective, longitudinal evaluation. Dis Esophagus. 2007;20:523-9.
- [Google Scholar]
- A review on oxaliplatin-induced peripheral nerve damage. Cancer Treat Rev. 2008;34:368-77.
- [Google Scholar]
- Brief assessment of adult cancer patients' perceived needs: Development and validation of the 34-item supportive care needs survey (SCNS-SF34) J Eval Clin Pract. 2009;15:602-6.
- [Google Scholar]
- Disability in America: Toward a National Agenda for Prevention. In: Pope A, Tarlov A, eds. Disability in America: Toward a National Agenda for Prevention. Washington DC: National Academy Google Scholar; 1991.
- [Google Scholar]
- The increasing disparity in mortality between socioeconomic groups in the united states, 1960 and 1986. N Engl J Med. 1993;329:103-9.
- [Google Scholar]
- Physical function and social class among Swedish oldest old. J Gerontol. 1994;49:S196-201.
- [Google Scholar]
- Association of education and income with estrogen receptor status in primary breast cancer. Am J Epidemiol. 1995;142:796-803.
- [Google Scholar]
- Ethnic differences in risk and prognostic factors for breast cancer. Cancer. 1995;76:268-74.
- [Google Scholar]
- Race/ethnicity, social class, and prevalence of breast cancer prognostic biomarkers: A study of white, black, and Asian women in the San Francisco bay area. Ethn Dis. 1997;7:137-49.
- [Google Scholar]
- Socioeconomic position predicts specialty mental health service use independent of clinical severity: The TRAILS study. J Am Acad Child Adolesc Psychiatry. 2010;49:647-55.
- [Google Scholar]
- Quality of life and psychiatric co- morbidity in Indian migraine patients: A headache clinic sample. Neurol India. 2013;61:355-9.
- [Google Scholar]
- Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL group. Psychol Med. 1998;28:551-8.
- [Google Scholar]
- Cut-off point for WHOQOL-bref as a measure of quality of life of older adults. Rev Saude Publica. 2014;48:390-7.
- [Google Scholar]
- Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;32:57-71.
- [Google Scholar]
- Depression and anxiety in women with early breast cancer: Five year observational cohort study. BMJ. 2005;330:702.
- [Google Scholar]
- Effects of breast conservation on psychological morbidity associated with diagnosis and treatment of early breast cancer. Br Med J (Clin Res Ed). 1986;293:1331-4.
- [Google Scholar]
- The Psychosocial Dimensions of Cancer. New York: Free Press; 1983.
- Recent advances in the pharmacologic and behavioral management of chemotherapy-induced emesis. Arch Intern Med. 1984;144:1029-33.
- [Google Scholar]
- Adjuvant chemotherapy for breast carcinoma: Psychosocial implications. Cancer. 1979;43:1613-18.
- [Google Scholar]
- Update: NCCN practice guidelines for themanagement of psychosocial distress. Oncology. 1999;13:459-507.
- [Google Scholar]
- Life after breast cancer: Understanding women's health-related quality of life and sexual functioning. J Clin Oncol. 1998;16:501-14.
- [Google Scholar]
- Quality of life after breast carcinoma surgery: A comparison of three surgical procedures. Cancer. 2001;91:1238-46.
- [Google Scholar]
- Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36:1-0.
- [Google Scholar]
- Depression in palliative care patients – A prospective study. Eur J Cancer Care (Engl). 2001;10:270-4.
- [Google Scholar]
- Age-related differences in the quality of life of breast carcinoma patients after treatment. Cancer. 1999;86:1768-74.
- [Google Scholar]
- Psychosocial well-being and supportive care needs of cancer patients living in urban and rural/regional areas: A systematic review. Support Care Cancer. 2012;20:1-22.
- [Google Scholar]
- Racial/Ethnic Minorities in Rural Areas: Progress and Stagnation 1980-1990 (AER-731). Washington, DC: US Department of Agriculture; 1996.
- Meeting the needs of rural breast cancer survivors: What still needs to be done? J Womens Health Gend Based Med. 2000;9:667-77.
- [Google Scholar]
- Strengths and vulnerabilities of women of Mexican descent in relation to depressive symptoms. Nurs Res. 2002;51:175-82.
- [Google Scholar]
- Mental health service use in a nationwide sample of Korean adults. Soc Psychiatry Psychiatr Epidemiol. 2009;44:943-51.
- [Google Scholar]
- Factors associated with child mental health service use in the community. J Am Acad Child Adolesc Psychiatry. 1997;36:901-9.
- [Google Scholar]
- The excess burden of breast carcinoma in minority and medically underserved communities: Application, research, and redressing institutional racism. Cancer. 2000;88:1217-23.
- [Google Scholar]
- Family change and support of the elderly in Asia: What do we know? Asia Pac Popul J. 1992;7:13-32.
- [Google Scholar]
- Marital quality and family typology: Effects of Pakistani adolescent's mental health. Eur Sci J. 2014;2:228.
- [Google Scholar]
- The Changing face of family & its implications on the mental health profession in Delhi. Delhi Psychiatry J. 2011;14:5-8.
- [Google Scholar]
- Marital adjustment among women: A comparative study of nuclear and joint families. Int J Indian Psychol. 2016;3:26-32.
- [Google Scholar]
- Marital Adjustment in Tribal and Non-Tribal Working Women. New Delhi: MD Publications Pvt. Ltd.; 1997.
- The role of disclosure patterns and unsupportive social interactions in the well-being of breast cancer patients. Psychooncology. 2004;13:96-105.
- [Google Scholar]
- Psychoemotional aspects of mastectomy: A review of recent literature. Am J Psychiatry. 1975;132:56-9.
- [Google Scholar]
- Event-related potential changes in chronic alcoholics. Electroencephalogr Clin Neurophysiol. 1979;47:637-47.
- [Google Scholar]






