Translate this page into:
Intramedullary Spinal Cord Metastases of Malignant Melanoma: A Rare Case Report on Paraplegia in Palliative Care
Address for correspondence: Dr. Arunangshu Ghoshal, Department of Palliative Medicine, Tata Memorial Hospital, Mumbai - 400 012, Maharashtra, India. E-mail: arun.bata@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Rates of malignant melanoma have been increasing in frequency. Studies have shown that up to 46% of patients with melanoma will experience metastases to the central nervous system. Intramedullary spinal cord metastasis of malignant melanoma is rare. In advanced cancers, surgery might not be possible, and radiotherapy with corticotherapy is a viable option. In the following case, a 54-year-old male presented to the clinic with an intramedullary tumor in the D1 region. He was successfully managed with an integrated palliative care approach with concomitant cancer-directed therapy.
Keywords
Intramedullary metastasis
melanoma
palliative care
INTRODUCTION
Development of intramedullary spinal cord metastases (ISCM) is a rare event in the course of malignant diseases. However, it is on the rise probably due to more effective therapies that result in the prolongation of survival.[1] This is reflected in the volume of recently published case reports and case series of ISCM.[2] Most of the ISCMs are asymptomatic and, therefore, are not diagnosed; however, autopsy studies have demonstrated an incidence of ISCM up to 2%.[3] Because of the low frequency of treated cases, therapy standards are still to be defined. The main goal in treating ISCM is to maintain mobility and neurological functions for patients with limited life expectancy. Surgery is favored but is still second to primarily anti-edematous systemic therapy combined with or followed by radiation. However, the clinical benefit thereby achieved is often very limited, and palliation is associated with considerable side effects, particularly from continuous steroid therapy.[4] To our knowledge, this is the first case report of clinical outcomes from ISCM managed through an integrated palliative care model.
CASE REPORT
Mr. JHF was a 54-year-old banker who was diagnosed with Stage 2 melanoma on the right lateral aspect of the heel 3 years ago. He has been married for 20 years and has three children, with the age range of 7, 9, and 11 years. He underwent wide excision surgery with skin grafting and was subsequently treated every 3 weekly with chemotherapy and followed up as needed in case of any adverse events. Cancer recurred in regional lymph nodes after 4 months. He underwent further excision surgeries and was started on immunotherapy with nivolumab and ipilimumab. He developed toxicity after five cycles and was thus treated only with nivolumab for four more cycles. Staging scans showed disease progression and he was then shifted to pembrolizumab for three more cycles.[5]
He presented to the emergency department with severe (10/10) mid-back pain with no radiation of pain. The pain was worse with Valsalva maneuver, straining at stool, cough, and at night. It was not pleuritic. It was a deep, aching pain, without burning or electric shock-like sensations. There was no tenderness to palpation at the site of the pain and no changes in the skin of the back. He was taking acetaminophen with tramadol but without any relief. The physical examination revealed bilateral lower limb weakness 4/5 with reflexes 1+, normal sensation, and no bowel or bladder incontinence. His laboratory studies were within normal limits except for hemoglobin of 10 g/dl. Positron emission tomography–computerized tomography scan showed evidence of metastatic disease in the liver, retroperitoneal lymph nodes, and multiple marrow lesions. He underwent a biopsy of the liver lesions, which revealed metastatic melanoma. Spinal magnetic resonance imaging (MRI) showed a single D1 intramedullary lesion, without any hemorrhage or cord compression [Figure 1].
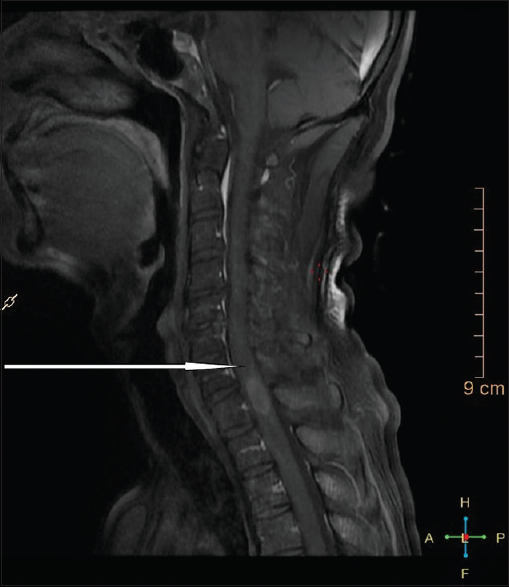
- D1 intramedullary lesion (pointed with arrow)
Mr. JHF's pain became tolerable after a bolus of 10 mg of IV dexamethasone and 3 mg of IV morphine. His goals were to remain at home, be independent in his activities of daily livings and instrumental activities of daily livings, and work part-time. He was started on 4 mg oral dexamethasone four times a day. On the second hospital day, his case was presented to the multidisciplinary solid tumor disease management group and attended by clinicians from neurosurgery, radiation oncology, medical oncology, diagnostic and interventional radiology, and pathology. He did not have spinal instability (Spinal Instability Neoplastic Score = 5 points)), but his prognosis was bad (modified Bauer = 1 point). Hence, though his lesion was in the thoracic or semi-rigid spine, and surgery could be done from a single posterior approach, given the findings, the group recommended radiation therapy (RT) and no surgery [Figure 1]. JHF underwent five fractions of palliative RT, began physical therapy (PT), and returned home ambulatory with a wheeled walker and home PT.
Over the next 3 months, JHF continued with systemic therapy and monthly zoledronic acid but developed new onset of 8/10 pain between his scapulae with radiation of pain and paresthesia to his left 6th and 7th intercostal spaces. Scans showed metastatic disease in his lungs with left 6th rib lesion associated with soft-tissue component. He was Eastern Cooperative Oncology Group PS2. Dexamethasone and opioids were restarted; 8 Gy in single fraction was given to the left 6th rib. JHF completed his RT and continued with systemic chemotherapy for metastatic melanoma. A month later, he gradually developed pain in his lower thoracic and lumbar spine with associated bladder incontinence. He had now difficulty in climbing onto his bed from the chair. MRI showed multifocal epidural disease from T9-L1, with compression of the conus/cauda equina. His goals were to be mobile in the house and to regain urinary continence so that he can continue to socialize and be active. His wife is a healthy, 50-year-old woman, able to take care of him at home. Given JHF's findings and goals, palliative re-irradiation to the spine, 20 Gy in five fractions from T8-L2, was recommended. His lower motor neuron injuries produced a flaccid, rather than the tonic, neurologic bladder which caused socially devastating incontinence. His lower-extremity weakness prevented independent transfers or household-level mobility. Intensive rehabilitation therapy was recommended. His wife arranged for the recommended home modifications with air bed for the patient, and JHF was discharged home after 2 weeks. He had mastered a self-catheterization program that restored urinary continence. With assistive devices and caregiver assistance for stair climbing, he could be in his home safely. The patient was also started on tablet dexamethasone on tapering doses for spinal cord compression symptoms. He was started on fentanyl transdermal patch (37.5 mcg/h/72 hourly) for pain and oral tablet morphine 10 mg SOS for breakthrough pain and tablet etoricoxib (60 mg twice daily) as an adjuvant. A local physician was contacted, explained about the management, and was asked to be available in case of emergency. JHF was also put on weekly home care services.
DISCUSSION
ISCM is an unusual type of cancer metastases. The most common location of ISCM is the thoracic cord (42%) followed by the cervical cord (31%).[6] In our patient, the metastasis was located at the thoracic cord. In 50%–59% of cases, there are concurrent brain metastases,[7] but no brain metastasis was determined in our patient. There are many suggested pathogenetic mechanisms for ISCM — hematogenous spread, dissemination through the vertebral venous plexus and direct invasion of nerve roots.[6] As reported in a review by Grem et al.,[6] the most frequent presenting complaints are pain and motor deficit. In our patient, the pain was the initial symptom and was followed by weakness of the extremities. Sudden onset of neurological deficit and rapid progression are the most consistent characteristics of ISCM, and this is helpful in distinguishing it from the slow-growing primary spinal intramedullary tumors.[8] Paresthesia is less frequent as an initial symptom. Dysfunction of the bowel and bladder is an unusual early manifestation of ISCM. MRI (especially T2-weighted) is the gold standard modality for detection of ISCM. The use of gadolinium-enhanced MR images has further improved sensitivity because they make it possible to distinguish metastatic tumor sites from the surrounding edema. However, there is still difficulty in distinguishing ISCM from primary spinal cord neoplasm or other nonneoplastic lesions.[9] MRI is also helpful to evaluate the response to therapy and to discern the presence of multiple metastatic lesions in the neuraxis.[10] Radiotherapy, chemotherapy, and surgery are treatment options for ISCM. However, there is no consensus on which treatment is the best one due to the lack of controlled studies. Most of the ISCMs are unresectable without causing additional neurological deficits. Since these tumors invade the spinal cord, ISCM resection and dissection from normal tissues are difficult. Radiotherapy with or without steroids is accepted as a gold standard worldwide, especially in patients with early diagnosis and radiosensitive tumors. Combination of steroids and RT has no additional survival benefit, but steroids can provide an improvement in the symptoms by acutely reducing peritumoral edema. Our patient had poor performance status that led us and the patient to choose a short-course radiotherapy. Chemotherapy alone is not the choice of treatment for ISCM cases but can be used in combination with other treatment modalities, especially in chemosensitive tumors.[11]
Providing successful palliation and improving patients’ quality of life require multidisciplinary strategic treatment planning. Our patient's treatment started with corticotherapy, and then he underwent radiotherapy with the tapered continuation of corticotherapy. An integrative approach to palliative care in acute care oncology setups could create a healing environment, like the one which supported our patient, his family, and health-care professionals. In the case of our patient, appropriate use on analgesics for pain helped reduce the anxiety. Mindful use of language enhanced the innate healing response, improved communication, and empowered patient and family to participate in his care planning. Continued weekly home care also helped in empowering the family and caregivers. The patient was thus able to get back home and could engage in meaningful activities of daily life.
CONCLUSION
This is a rare case report of a patient with malignant melanoma presenting with ISCM. He was managed with radiotherapy with concomitant corticotherapy and immunotherapy along with palliative care in an integrated fashion with oncology care. At present, the therapeutic treatments available for ISCM are controversial due to the lack of controlled studies, and early diagnosis is the key to improve prognosis. Palliative care clinicians are routinely consulted to assess and manage pain in cancer patients and must, therefore, have a high index of suspicion for neuraxis metastasis in these cases with painful motor weakness without sensory symptoms. Although disease progression might eventually cause paresis, paralysis, and loss of bowel/bladder function, integrated palliative care can preserve patients’ quality of life, autonomy, and dignity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the patient and his relatives and departmental staff.
REFERENCES
- Retrospective study of 19 patients with intramedullary spinal cord metastasis. Clin Neurol Neurosurg. 2009;111:10-7.
- [Google Scholar]
- Intramedullary spinal cord metastases: An increasingly common diagnosis. Neurosurg Focus. 2015;39:E15.
- [Google Scholar]
- Survival and functional outcome after surgical resection of intramedullary spinal cord metastases. World Neurosurg. 2012;77:370-4.
- [Google Scholar]
- Clinical outcome in patients with intramedullary spinal cord metastases from lung cancer. Clin Transl Oncol. 2007;9:172-6.
- [Google Scholar]
- American Cancer Society. Treatment of Melanoma Skin Cancer, by Stage. 2016. American Cancer Society. Available from: https://www.cancer.org/cancer/melanoma-skin-cancer/treating/by-stage.html
- [Google Scholar]
- Clinical features and natural history of intramedullary spinal cord metastasis. Cancer. 1985;56:2305-14.
- [Google Scholar]
- Intramedullary spinal cord metastases: A 20-year institutional experience with a comprehensive literature review. World Neurosurg. 2013;79:576-84.
- [Google Scholar]
- Intramedullary spinal cord tumors: A review of current and future treatment strategies. Neurosurg Focus. 2015;39:E14.
- [Google Scholar]
- Magnetic resonance imaging of intramedullary spinal cord lesions: A pictorial review. Curr Probl Diagn Radiol. 2010;39:160-85.
- [Google Scholar]
- Multimodality therapy improves survival in intramedullary spinal cord metastasis of lung primary. Hematol Oncol Stem Cell Ther. 2017;10:143-50.
- [Google Scholar]






