Translate this page into:
National Pediatric Palliative Care Needs from Hospital Deaths
Address for correspondence: Dr. Farah Khalid, Department of Paediatrics, Faculty of Medicine, University of Malaya, Jalan Universiti, 50603 Kuala Lumpur, Malaysia. E-mail: farahkhalid@um.edu.my
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
The objective of this study was to estimate palliative care needs and to describe the cohort of children with life-limiting illnesses (LLI) dying in hospitals.
Design:
This study was a retrospective cohort study. The national hospital admissions database was reviewed and children who had died who had life-limiting illnesses were identified.
Setting:
This study was conducted at Ministry of Health hospitals, Malaysia.
Patients:
Children aged 18 years and below who had died between January 1, 2012 and December 31, 2014.
Main Outcome Measures:
Life-limiting diagnoses based on Hain et al.'s directory of LLI or the ACT/RCPCH categories of life-limiting disease trajectories.
Results:
There were 8907 deaths and 3958 (44.4%) were that of children with LLI. The majority, 2531 (63.9%) of children with LLI were neonates, and the most common diagnosis was extreme prematurity <28 weeks with 676 children (26.7%). For the nonneonatal age group, the median age at admission was 42 months (1–216 months). A majority, 456 (32.0%) had diagnoses from the ICD-10 chapter “Neoplasms” followed by 360 (25.3%) who had a diagnoses from “Congenital malformations, deformations, and chromosomal abnormalities” and 139 (9.7%) with diagnoses from “Disease of the nervous system.” While a majority of the terminal admissions were to the general ward, there were children from the nonneonatal age group, 202 (14.2%) who died in nonpediatric wards.
Conclusion:
Understanding the characteristics of children with LLI who die in hospitals could contribute toward a more efficient pediatric palliative care (PPC) service development. PPC service should include perinatal and neonatal palliative care. Palliative care education needs to extend to nonpediatric healthcare providers who also have to manage children with LLI.
Keywords
Children
deaths
life-limiting illness
Malaysia
pediatric palliative care
INTRODUCTION
Over the past three decades, care provided for children with life-limiting illnesses (LLI) have improved albeit at variable pace in different parts of the world.[1] Palliative care for children is defined to begin at diagnosis of LLI,[2] and these children could be receiving care for a prolonged period, sometimes into adulthood, as the trajectories of these illnesses are diverse. Hence, it is challenging to quantify the actual number of children with palliative care needs for economical and rational planning of services. Prevalence studies are dependent on the local epidemiology and local healthcare data. The estimated prevalence worldwide varies greatly. In the UK, the prevalence was found to be 32/10000.[3]
In 2011, pediatric palliative care (PPC) service provision in Malaysia was reported to be at Level 2 based on the four levels of palliative care service provision developed by the international observatory of the end of life care.[4] There has since been a significant improvement in the awareness of the need for palliative care for children and the development of services especially over the recent years. Pediatricians, with interest in palliative care, are providing hospital-based consultative services in various regions of Malaysia.[5] Coordinated efforts are needed to ensure equitable delivery of care in a low-resource country such as Malaysia.
At present, the number of children with LLI who may benefit from palliative care is unknown. National policies and strategies for a more organized PPC service can be developed if a clearer understanding of the number of children with palliative care needs is available.
Mortality data have been used to provide an estimate of children who may benefit from palliative care.[678910] Murtagh et al. proposed that a reasonable estimate of patients with palliative care needs could be obtained by looking for palliative-care relevant conditions from both the underlying cause of death and contributory cause of death[11] It has been acknowledged though that these data do not reflect actual palliative care needs which are complex, individualized, and often unrelated to the actual diagnosis.[121314] Nevertheless, these numbers could contribute to service planning and development.
This retrospective audit aims to provide the estimate of children who may benefit from palliative care by using the national hospital admission data. Our objectives are to use this data to (i) identify the proportion of children dying in hospitals who have life-limiting illnesses, (ii) identify the primary team caring for these children, and (iii) map out distribustion of deaths from LLI in the various states across the country, matching them to current services. We hope this will help direct the development of PPC education and services.
METHODOLOGY
This is a retrospective audit of deaths among patients of 18 years old and below who were admitted to Ministry of Health Hospitals (MOH) in Malaysia between January 1, 2012 and December 31, 2014. The MOH's Informatics Centre keeps a database of all hospital admissions to MOH hospitals. From this database, the patients who had died who were 18 years old or less on admission were selected. The variables obtained were demographics, hospital location, admission diagnosis, underlying diagnosis, comorbidities, cause and date of death, admitting ward, admitting discipline, ward, and primary team at death. All the diagnoses were in the form of a written diagnosis and/or international statistical classification of diseases and related health problems – 10th Revision (ICD-10) codes.[15]
Figure 1 illustrates the process of identifying children with life-limiting diagnoses. Both investigators looked at all the patients’ diagnoses together. The ICD-10 codes that were immediately excluded were “Mental and Behavioral Disorders,” “Pregnancy,” “Childbirth and Puerperium,” and “Injury and Poisoning” chapters.
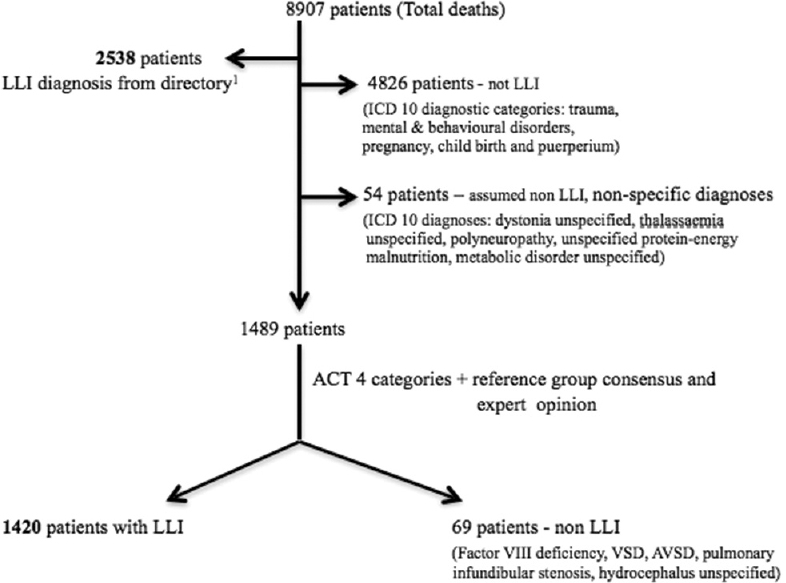
- Process of identifying patients with life-limiting illness (LLI)
Diagnoses in all four categories of each patient (“admitting diagnosis,” “underlying diagnosis,” “cause of death,” “comorbidities”) were looked at to ensure that a life-limiting diagnosis was not missed. The patients were selected if any one of these four categories had a life-limiting diagnosis according to the directory of LLI from Hain et al.[1617] Diagnoses that were not in the directory but considered to be life-limiting by both the investigators based on the ACT/RCPCH categories of life-limiting disease trajectories[18] were sent to members of the Malaysian PPC Reference Group (MyPPC) for their consensus. MyPPC is the only reference group in Malaysia represented by pediatricians leading PPC in Malaysia. When consensus could not be reached, consultants from the related specialties were consulted.
Descriptive analysis was used for demographic data, cross-tabulation analysis for categorical data, Mann–Whitney U-test to compare medians, and logistic regression models for identifying significant factors for deaths in the intensive care units. Analyses were performed with IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp. In this study, we have decided to analyze neonates separately as we feel this group of children have diagnoses and disease trajectories that are unique to them.
Ethical approval was obtained from the Medical Research and Ethics Committee (NMRR-14-320-19030).
RESULTS
Life-limiting diagnoses of all patients
From the diagnoses of the entire cohort of patients, we identified 84 diagnoses not in Hain et al.'s directory of LLI but met the criteria based on the ACT/RCPCH definition. Members of MyPPC excluded “unspecified hydrocephalus (G91.9).” Pediatricians of the relevant specialties were consulted for six diagnoses. Following that, “hemophilia” (D66), “emphysema, unspecified” (J43.9), “ventricular septal defects” (Q21.0), “atrioventricular septal defects”, (Q21.2) and “pulmonary infundibular stenosis” (Q24.3) were excluded, while rheumatoid arthritis (M05.3) was thought to be life-limiting given the potential systemic involvement of the illness. Hence, there were 78 diagnoses that were thought to be life-limiting but were not in Hain et al.'s directory of LLI [Table 1].
| ICD-10 Diagnostic Category | ICD-10 Codes and Diagnosis |
|---|---|
| Neoplasms | D38.1 Neoplasm of uncertain or unknown behavior: trachea, bronchus, lung |
| D38.3 Neoplasm of uncertain or unknown behavior: mediastinum | |
| D38.5 Neoplasm of uncertain or unknown behavior: other respiratory organs | |
| D40.1 Neoplasm of uncertain or unknown behavior: testes | |
| D44.5 Neoplasm of uncertain or unknown behaviour: pineal gland | |
| D46.9 Myelodysplastic syndrome; unspecified | |
| Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | D61.3 Idiopathic aplastic anemia |
| D80.9 Immunodeficiency with predominantly antibody defects, unspecified | |
| D84.9 Immunodeficiency, unspecified | |
| Endocrine, nutritional and metabolic diseases | E43 Unspecified severe protein-energy malnutrition |
| E51.2 Wernicke encephalopathy | |
| E66.2 Extreme obesity with alveolar hypoventilation (ROHHAD) | |
| E70.9 Disorder of aromatic amino-acid metabolism, unspecified | |
| E88.4 Mitochondrial metabolism disorder | |
| E88.8 Other specified metabolic disorders | |
| E88.9 Metabolic disorder, unspecified | |
| Diseases of the nervous system | G37.2 Central pontine myelinosis |
| G37.3 Acute transverse myelitis in demyelinating disease of central nervous system | |
| G80.9 Cerebral palsy, unspecified | |
| G91.1 Obstructive hydrocephalus | |
| G91.8 Other hydrocephalus | |
| G93.1 Anoxic brain damage, not elsewhere classified | |
| G93.4 Encephalopathy, unspecified | |
| G93.8 Other specified disorders of brain | |
| ICD-10 Diagnostic Category | ICD-10 Codes and Diagnosis |
| Diseases of the circulatory system | I08.3 Combined disorders of mitral, aortic and tricuspid valves |
| I24.9 Acute ischaemic heart disease, unspecified | |
| I27.1 Kyphoscoliotic heart disease | |
| I27.2 Other secondary pulmonary hypertension | |
| I27.8 Other specified pulmonary heart diseases | |
| I50.0 Congestive cardiac failure | |
| I50.1 Left ventricular failure | |
| I50.9 Heart failure; unspecified | |
| I61.0 Intracerebral haemorrhage in hemisphere, subcortical | |
| I61.4 Intracerebral haemorrhage in cerebellum | |
| I61.5 Intracerebral haemorrhage, intraventricular | |
| I61.6 Intracerebral haemorrhage, multiple localized | |
| I61.9 Intracerebral haemorrhage, unspecified | |
| I62.9 Intracranial haemorrhage (nontraumatic), unspecified | |
| I63.9 Cerebral infarction, unspecified | |
| I64 Stroke, not specified as haemorrhage or infarction | |
| P57.9 Kernicterus, unspecified | |
| P91.0 Neonatal cerebral ischaemia | |
| P29.1 Neonatal cardiac dysrhythmia | |
| P52.2 Intraventricular (nontraumatic) haemorrhage, grade 3, of fetus and newborn | |
| P52.3 Unspecified intraventricular (nontraumatic) haemorrhage of fetus and newborn | |
| Diseases of the digestive system | K76.7 Hepatorenal syndrome |
| Diseases of the respiratory system | J44.9 Chronic obstructive pulmonary disease, unspecified |
| J47 Bronchiectasis | |
| Diseases of the musculoskeletal system and connective tissue | M05.3 Rheumatoid arthritis with involvement of other organs and systems |
| Conditions originating in perinatal period | P07.0 Extremely low birth weight (<999g) |
| P07.2 Extreme prematurity <28wks | |
| P11.1 Other specified brain damage due to birth injury | |
| P20.9 Intrauterine hypoxia, unspecified | |
| P27.1 Bronchopulmonary dysplasia originating in the perinatal period | |
| P29.1 Neonatal cardiac dysrhythmia | |
| P52.2 Intraventricular (nontraumatic) haemorrhage, grade 3, of fetus and newborn | |
| P52.3 Unspecified intraventricular (nontraumatic) haemorrhage of fetus and newborn | |
| P57.9 Kernicterus, unspecified | |
| P91.0 Neonatal cerebral ischaemia |
Following this list of diagnoses, we identified 3958 (44.4%) patients who had a life-limiting illness; 2538 of whom had a diagnosis from Hain et al.'s directory.
All deaths from January 1, 2012 to December 31, 2014
There were 8907 deaths during the study period, and 42.3% were female. The vast majority (91.0%) were Malaysian citizens, and 51.1% were older than 28 days old (nonneonates). Over a third of deaths occurred on general pediatric wards [Table 2].
| All patients (n =8907) | LLI (n=3958) | |
|---|---|---|
| Age | ||
| ≤28 days | 4355 (48.9%) | 2531 (63.9%) |
| 29 days to 12 months | 1367 (15.3%) | 478 (12.1%) |
| 12 months to 72 months | 1092 (12.3%) | 360 (9.1%) |
| 73 months to 156 months | 10 (9.1%) | 275 (6.9%) |
| 157 months to 216 months | 1283 (14.4%) | 314 (7.9%) |
| Gender | ||
| Females | 3772 (42.3%) | 1714 (43.3%) |
| Males | 5093 (57.2%) | 2211 (55.8%) |
| No information | 42 (0.5%) | 33 (0.8%) |
| Nationality | n=8860 | n=3940 |
| Malaysians | 8063 (91.0%) | 3637 (92.3%) |
| Admission ward | ||
| Intensive care (PICU + ICU + HDU)* | 780 (8.8%) | 218 (5.5%) |
| NICU/SCN | 3073 (34.5%) | 1829 (46.2%) |
| General ward | 3741 (42.0%) | 1396 (35.3%) |
| Other wards** | 1313 (14.7%) | 515 (13.0%) |
| Deaths | n=8868 | |
| Intensive care (PICU + ICU + HDU) | 1234 | 378 (9.5%) |
| NICU/SCN | 3115 | 1836 (46.4%) |
| General ward | 3350 | 1273 (32.2%) |
| Other wards | 1169 | 471 (11.9%) |
*PICU: Paediatric Intensive Care Unit, ICU: Intensive Care Unit, HDU: High Dependency Unit ** Surgical, neurosurgical, cardiothoracic, plastic surgery, orthopedics
Of the 3958 (44.4%) patients who had LLI, a large majority (63.9%) were neonates and neonatal intensive care units (ICU) or special care nurseries were the most common admission wards 46.4%.
The distribution of the proportion of death of children with LLI was fairly constant throughout the different regions in Malaysia [Figure 2].
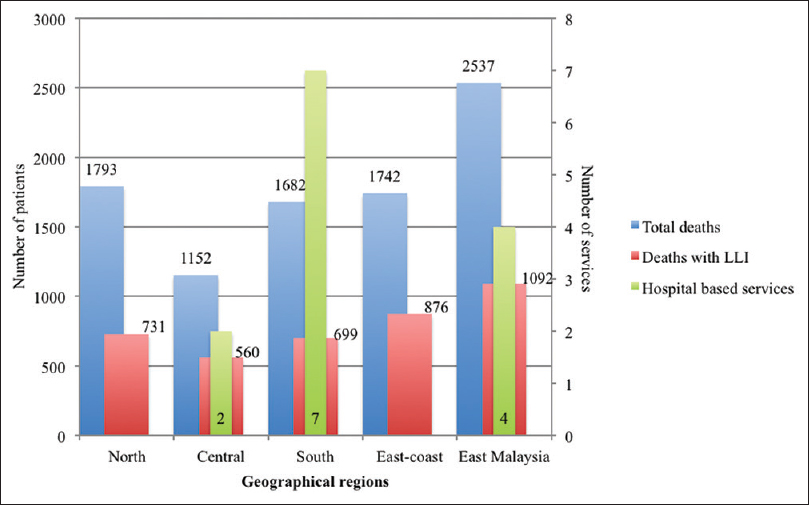
- Distribution of deaths with life-limiting diagnoses across Malaysia and the existing hospital-based palliative care services
Nonneonates with life-limiting illnesses
There were 4552 deaths of children older than 28 days, and 1427 (31.3%) of them had a LLI. The median age at terminal admission for children with LLI was 42 months (1–216 months). There is a statistically significant difference in the median age at terminal admission between children with LLI and children who do not have LLI, (P < 0.01) [Table 3].
| Variable | Diagnosis | Median (IQR) | Z-stat* | P | |
|---|---|---|---|---|---|
| All deaths | Age at admission (months) | With LLI | 42 (139) | ||
| Without LLI | 64 (165) | -5.86 | <0.01 | ||
| ICU deaths | Age at admission (months) | With LLI | 17 (78) | ||
| Without LLI | 35 (138) | -4.711 | <0.01 | ||
| Hospital stay (days) | With LLI | 6 (15) | |||
| Without LLI | 3 (9) | -4.754 | <0.01 |
*Mann-Whitney Test
Majority, 456 (32.0%), of children had diagnoses from ICD-10 chapter of “Neoplasms” followed by 360 (25.2%) with diagnoses from ICD-10 chapter of “Congenital malformations, deformations, and chromosomal abnormalities.” The majority of those, who died from neoplasms, were young children beyond infancy and below 12 years of age while the majority of children with “Congenital malformations, deformations, and chromosomal abnormalities” died before their first birthday. Of all the nonneonates with LLI, 41.3% were of school-going age (6–18 years) [Table 4].
| ICD-10 code | ICD 10 Diagnostic group | 1 month to 12 months | 13 months to 72 months | 73 months to 156 months | 157 months to 216 months | n (%) |
|---|---|---|---|---|---|---|
| C00 - D48 | Neoplasms | 34 | 132 | 132 | 158 | 456 (32.0%) |
| Q00 - Q99 | Congenital malformations, deformations and chromosomal abnormalities | 241 | 75 | 28 | 16 | 360 (25.2%) |
| G00 - G99 | Diseases of the nervous system | 27 | 41 | 33 | 38 | 139 (9.7%) |
| I00 - I99 | Diseases of the circulatory system | 39 | 29 | 25 | 36 | 129 (9.0%) |
| P00 - P96 | Certain conditions originating in the perinatal period | 58 | 11 | 11 | 3 | 83 (5.8%) |
| N00 - N99 | Diseases of the genitourinary system | 13 | 18 | 15 | 25 | 71 (5.0%) |
| K00 - K93 | Diseases of the digestive system | 29 | 22 | 6 | 7 | 64 (4.5%) |
| D50 - D89 | Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 9 | 8 | 8 | 12 | 37 (2.6%) |
| E00 - E90 | Endocrine, nutritional and metabolic diseases | 3 | 13 | 9 | 9 | 30 (2.1%) |
| A00 - B99 | Certain infectious and parasitic diseases | 17 | 6 | 6 | 1 | 34 (2.4%) |
| J00 - J99 | Diseases of the respiratory system | 8 | 5 | 1 | 5 | 19 (1.3%) |
| M00 - M99 | Diseases of the musculoskeletal system and connective tissue | 0 | 0 | 1 | 4 | 5 (0.4%) |
P<0.01
While most of the terminal admissions were to the general pediatric ward, 951 (66.6%), 202 (14.2%) were admitted to nonpediatric wards [Figure 3].

- Wards at admission and deaths of non-neonates with life-limiting illnesses (N = 1427). (a) Wards at terminal admission (b) Wards at death. *Surgical, neurosurgical, cardiothoracic, plastic surgery, orthopedics
Deaths in the intensive care units
There were 1370 deaths in the intensive care wards and 419 (30.6%) were that of children with a LLI. The median age of children with life-limiting and non life-limiting illnesses was 17 months (1–216 months) and 35 months (1–215 months) (P < 0.01), respectively. The median length of stay was longer in children with LLI; 6 days (0–289 days) as compared to 3 days (0–381 days) in those who did not have a LLI, (P < 0.01) [Table 3].
When adjusting for age, there is no statistically significant relationship between having an LLI with dying in the ICU [Table 5].
| Variable | P | OR (95% CI for odds ratio) | |
|---|---|---|---|
| All deaths in the intensive care units | Age (months) | <0.01 | 0.995 (0.995-0.996) |
| LLI diagnosis (ref. not LLI diagnosis) | 0.08 | 0.884 (0.769-1.107) | |
| All deaths with a life-limiting illness in intensive care units | Age (months) | <0.01 | 0.995 (0.993-0.996) |
| LLI diagnosis categories | |||
| ‘Congenital malformations, deformations and chromosomal abnormalities’ (ref ‘Neoplasms’) | <0.01 | 0.444 (0.319-0.618) | |
| ‘Diseases of the Central Nervous System’ (ref Neoplasms) | 0.03 | 0.703 (0.312-0.966) | |
| ‘Diseases of the Cardiovascular System’ (ref Neoplasms) | 0.01 | 0.555 (0.354-0.872) | |
| ‘Others’(ref Neoplasms) | 0.06 | 0.656 (0.418-1.028) | |
ICU deaths was considered as reference category for dependent variable (ICU deaths=1, Deaths in other wards=0). Note: *P (P<0.01). Multicolinearity were checked using SE and no multicollinearity found
Of all the children with a life-limiting diagnosis, the overall association between age and diagnostic categories with dying in ICU is statistically significant. When adjusting for age, children with “Congenital malformations, deformations, and chromosomal abnormalities” and “Diseases of the Cardiovascular System” were significantly less likely to die in the ICU as compared to children with “Neoplasms,” (P ≤ 0.01) [Table 5].
Neonates with life-limiting illnesses
There were a total of 4355 neonatal deaths with 2531 having a LLI. The most common ICD-10 diagnostic category was “Certain conditions originating in the perinatal period” and the most common diagnosis in this category was extreme prematurity <28 weeks [Table 6].
| ICD-10 code | ICD-10 Diagnostic group | n (%) |
|---|---|---|
| P00 - P96 | Certain conditions originating in the perinatal period | 1418 (56.0%) |
| 5 most common diagnoses P07.2 extreme Prematurity <28 wks | 676 | |
| P29.3 Persistent foetal circulation | 162 | |
| P91.6 HIE of newborn | 133 | |
| P21.9 birth asphyxia | 114 | |
| P07.0 extremely low birth weight, <999g | 81 | |
| Q00 - Q99 | Congenital malformations, deformations and chromosomal abnormalities | 983 (38.8%) |
| C00 - D48 | Neoplasms | 20 (0.8%) |
| G00 - G99 | Diseases of the nervous system | 32 (1.3%) |
| I00 - I99 | Diseases of the circulatory system | 28 (1.1%) |
| N00 - N99 | Diseases of the genitourinary system | 9 (0.4%) |
| K00 - K93 | Diseases of the digestive system | 8 (0.3%) |
| E00 - E90 | Endocrine, nutritional and metabolic diseases | 20 (0.8%) |
| D50 - D89 | Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 2 (0.1%) |
| A00 - B99 | Certain infectious and parasitic diseases | 6 (0.2%) |
| J00 - J99 | Diseases of the respiratory system | 4 (0.2%) |
| R00 - R99 | Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 1 (0.0%) |
Of those with LLI, the median age at admission was 0 days (0–28 days), and the median length of stay was 2 days (0–408 days). A large majority 2335 (92.2%) died within 24 h of admission. Majority were admitted to intensive care wards, 1752 (69.2%) to neonatal intensive care unit, and 21 (0.9%) to the pediatric intensive care unit. The median length of stay in the intensive care wards was 1 day (0–260 days).
Primary teams responsible for patient's care
Although majority of patients were cared for by pediatricians, there were 802 (20.3%) who had physicians of various specialties as their primary healthcare providers.
DISCUSSION
This study showed 44.4% of children who died in hospitals had a LLI and this is consistent with other hospital-based published studies.[710] We believe this provides a reliable estimate as all contributing diagnoses were reviewed to identify life-limiting diagnoses. The common diagnostic categories for children in the nonneonatal age group are also similar to other published studies.[368]
LLI are defined as illnesses where there is no reasonable chance of cure. However, opportunities for cure are determined by local context and resources. We have shown that subjective assessment of the diagnoses presented in this study uncovered additional life-limiting diagnoses that could expand the existing directory of LLI by Hain et al.[1617]
We hope this study creates an awareness of the heterogeneity of diagnoses of children with palliative care needs. However, diagnoses alone will not accurately identify children's palliative care needs. It is essential that palliative care education emphasizes on identifying needs based on the impact of diseases on the patients and family rather than the diagnosis alone.
Our results show that some children with LLI die in nonpediatric wards. Hence, in planning a comprehensive national PPC service, training needs to include nonpediatricians. Children with life-limiting diagnoses were found distributed all across the age groups highlighting the need for palliative care providers to be competent in managing children at different developmental stages. A multidisciplinary approach, including social and education services, will be important.
Having LLI does not increase the likelihood of dying in intensive care; however, those who do have LLI have a longer hospital stay. There were also children transferred from general wards for intensive care during their terminal admissions [Figure 3]. Addressing advanced care planning and end-of-life issues may have been able to prevent invasive life-sustaining interventions, thus allowing more opportunities for palliative care support. There is now increasing evidence that palliative care allows for better utilization of healthcare resources.[19] Keele et al. had demonstrated fewer invasive procedures and less admissions to the intensive care in patients with LLI receiving palliative care[2021] This is an important consideration for countries with limited resources, as in Malaysia.
Neonates were majority (63.9%) in this study with extreme prematurity being the most common diagnosis. This emphasizes the need for perinatal and neonatal palliative care services to develop concurrently with PPC services.
A large proportion (40.7%) of children who died with LLI was from two regions in Malaysia not known to have hospital-based consultative PPC services [Figure 2]. The development of hospital-based services in the country has been driven by individuals and advocates leading to disparities between available services and numbers of children needing palliative care. Hence, national strategies are required to ensure equitable palliative care for children.
Limitations
This study looked at deaths in all MOH which represents the majority of hospitals in the country. There is no data from the private hospitals or from the university hospitals in the country. Hence, not all deaths in the country are represented in this study. However, the in-patient load in university hospitals is much smaller than that in the Ministry of Health hospitals. From the 2015 census, all three university hospitals recorded 14 575 in-patients as compared to 407 198 in-patients from MOH hospitals (personal communication, Dr. Raymond Warouw, 2016). Whereas we do not have figures for the private hospitals, we know from experience that most chronic and seriously ill children in Malaysia are seldom managed in private hospitals. The accuracy of ICD-10 diagnosis from the national dataset is dependent on the quality of collection at each hospital and cannot be verified by the authors.
CONCLUSION
Almost half of the children dying in hospitals in Malaysia have a LLI and potentially have palliative care needs. Current services are not distributed equitably in the country. We hope this study reinforces the need to integrate palliative care into the different pediatric subspecialties and the surgical-based specialties that manage children. Efforts to develop palliative care for children by policymakers, service providers, researchers, and advocates need to be coordinated to ensure needs of children with LLI throughout the country are met. Programs to develop PPC as a specialized field is timely, and should run concurrently with education and training of all nonpediatricians who care for children.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors would like to acknowledge Dr. Md Khadzir bin Sheikh Ahmad and Suhaya binti Komari from the Health Informatics Centre, Ministry of Heath, Malaysia for their assistance with data extraction from the national admissions database.
REFERENCES
- History and epidemiology. In: Ann Goldman RH, Stephen Liben, eds. Oxford Textbook of Palliative Care for Children (2nd ed). United States: Oxford University Press; 2012. p. :3-12.
- [Google Scholar]
- 2013. WHO Definition of Palliative Care. Available from: http://www.who.int/cancer/palliative/definition/en/
- Rising national prevalence of life-limiting conditions in children in England. Pediatrics. 2012;129:e923-9.
- [Google Scholar]
- The international observatory on end of life care: A global view of palliative care development. J Pain Symptom Manage. 2007;33:542-6.
- [Google Scholar]
- Clinical spectrum of children receiving palliative care in Malaysian hospitals. Med J Malaysia. 2017;72:32-6.
- [Google Scholar]
- Pediatric deaths attributable to complex chronic conditions: A population-based study of Washington State, 1980-1997. Pediatrics. 2000;106:205-9.
- [Google Scholar]
- Characteristics of deaths occurring in children's hospitals: Implications for supportive care services. Pediatrics. 2002;109:887-93.
- [Google Scholar]
- Estimating the size of a potential palliative care population. Palliat Med. 2005;19:556-62.
- [Google Scholar]
- Assessing need for palliative care services for children in Mexico. J Palliat Med. 2015;18:162-6.
- [Google Scholar]
- How many people need palliative care? A study developing and comparing methods for population-based estimates. Palliat Med. 2014;28:49-58.
- [Google Scholar]
- Palliative care needs to be provided on basis of need rather than diagnosis. BMJ. 1999;318:123.
- [Google Scholar]
- Palliative care for infants, children, adolescents, and their families. J Palliat Med. 2006;9:163-81.
- [Google Scholar]
- Assessing palliative care needs: Views of patients, informal carers and healthcare professionals. J Adv Nurs. 2007;57:77-86.
- [Google Scholar]
- International Statistical Classification of Diseases and Related Health Problems. (10th Revision). Available from: http://apps.who.int/classifications/icd10/browse/2016/en
- Directory Of Life-limiting Conditions 2011. Available from: http://www.togetherforshortlives.org.uk/assets/0000/7089/Directory_of_LLC_v1.3.pdf
- Paediatric palliative care: Development and pilot study of a ‘directory’ of life-limiting conditions. BMC Palliat Care. 2013;12:43.
- [Google Scholar]
- Disease trajectories and ACT/RCPCH categories in paediatric palliative care. Palliat Med. 2010;24:796-806.
- [Google Scholar]
- Community-based pediatric palliative care for health related quality of life, hospital utilization and costs lessons learned from a pilot study. BMC Palliat Care. 2016;15:73.
- [Google Scholar]
- Differences in characteristics of dying children who receive and do not receive palliative care. Pediatrics. 2013;132:72-8.
- [Google Scholar]
- Evidence on the cost and cost-effectiveness of palliative care: A literature review. Palliat Med. 2014;28:130-50.
- [Google Scholar]






