Translate this page into:
Need for Palliative Care in Patient with Rheumatoid Arthritis: A Cross-sectional Observational Study

*Corresponding author: Nishkarsh Gupta, Department of OncoAnesthesiology and Palliative Medicine, Dr. B. R. Ambedkar Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi, India. drnishkarsh@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahendru K, Gupta N, Soneja M, Malhotra RK, Kumar V, Garg R, et al. Need for palliative care in patient with rheumatoid arthritis: A cross-sectional observational study. Indian J Palliat Care 2021;27(2):275-80.
Abstract
Objectives:
Rheumatoid arthritis (RA) is a chronic disorder causing inflammation in the joints and achieving remission is often the primary goal of physicians. We evaluated the suffering from RA and assessed the need for palliative care services in these patients.
Materials and Methods:
This cross-sectional observational study was done in 100 adult RA cases who attended the outpatient department. The Disease Activity Score 28 (DAS28), Health Assessment Questionnaire Disability Index, depression, anxiety and stress score, Short Form 36 Health Survey and numeric rating scale were assessed. The relationship between DAS28 with the other parameters and scores was assessed using Spearman’s rho correlation coefficient.
Results:
About 90% of patients in our study were female and majority (50%) had a moderate disease activity. The DAS28 showed a positive correlation with the degree of depression (r = 0.671, P = 0.000), anxiety (r = 0.609, P = 0.000) and stress levels (r = 0.474, P = 0.000). The patients with severe disease had a poor quality of life (QoL) [physical functioning (r = –0.737, P = 0.000); role limitation (r = –0.662, P = 0.000); emotional problem (r = –0.676, P = 0.000); energy/fatigue (r = –0.638, P = 0.000); social functioning (r = –0.658, P = 0.000); emotional well-being (r = –0.605, P = 0.000); general health (r = –0.643, P = 0.000); health change (r = –0.376, P = 0.000) and numerical rating scale score for pain (r = 0.656, P = 0.000)].
Conclusion:
RA patients with high disease activity suffer from depression, anxiety, stress and poor QoL. Palliative care physicians and rheumatologists must be vested with the power to provide comprehensive care to these patients.
Keywords
Anxiety
Palliative care
Rheumatoid arthritis
Stress
Quality of life
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic disease that occurs due to autoimmune damage to the synovial lining of the joints along with the involvement of other organ systems. It leads to progressive disability, premature death and socioeconomic burden.[1] Global Burden of Disease 2010 study has estimated a prevalence rate of 0.24% worldwide.[2] The arthralgia in RA is symmetrical and often leads to limitations in the range of motion of the involved joints. The initial 12 weeks after initiation of symptoms of RA are considered the optimal period for therapeutic interventions as it leads to improved long-term outcomes with reduced joint destruction and fewer chances to progress toward disability.[3-5] While there is currently no cure for RA, modern pharmacological therapies aim to achieve a remission or low activity disease state rapidly. Most studies have reported that remission at any time point (point remission) in patients with RA was possible in 33–49% of patients but sustained remission was possible in only 10% of cases.[6,7] Therefore, like many other chronic diseases, a small subset of the patients with severe RA may have a gradual downhill course with phases of increased disease activity alternating with periods of remission. Despite all the treatment patient is receiving, the quality of life (QoL) may be greatly affected because of the disease progression overtime and side effects of the immunosuppressive therapy received. Patients with RA often suffer from pain, anorexia, breathlessness, debility and frequent visits to hospital needing intensive care during the last year of their lives.[8] Thus, the timely assessment of functional status and QoL is very important in these patients.
Palliative care helps in improving the QoL of patients and their families suffering from a life-threatening illness. It helps them to overcome adversity by providing relief of various symptoms such as pain and other problems (physical, psychosocial and spiritual) by timely identification, assessment and intervention.[9] Nowadays, the patient-reported outcome measures (PROMs) are an integral measure of treatment response. Several scores such as Health Assessment Questionnaire Disability Index (HAQ-DI), the PROM information system and the Short Form 36 Health Survey (SF-36) scale have been used to assess PROMs in RA patients.[10,11] There is limited literature that has explored the QoL issues in patients with RA in developing countries.
We conducted this observational study at a tertiary care centre to assess the QoL, level of depression, anxiety, stress and the severity of pain in patients with RA and correlated it with their disease severity.
MATERIALS AND METHODS
After the Institutional Ethics Committee (IEC-145/06.04.2018) approval, this prospective observational study was done in RA patients presenting to a tertiary care hospital. All patients fulfilling the American College of Rheumatology/European league against rheumatism classification criteria, aged 18 years or above attending the outpatient department were recruited in the study.[12] Written informed consent was obtained from patients explaining the entire detail of the study in the language best understood by them.
The information was collected utilizing a structured questionnaire which includes demographic variables and validated tools for measuring the disease severity, degree of disability, depression, anxiety, stress levels and QoL. The demographic data included the patient’s name, age, education and occupation. The duration of diagnosis and numeric rating scale (NRS) to assess the pain at the time of presentation was recorded. The Disease Activity Score (DAS) was assessed by the researcher, as it describes the severity of RA using clinical and laboratory data. Whereas, all the other parameters including QoL, depression, anxiety and stress levels were assessed using freely accessible tools validated in local language (Hindi). These forms were filled by the patients and were assisted by an independent researcher if needed in the outpatient department.
DAS 28[13]
DAS28 or “DAS” assesses the severity of disease based on four parameters, namely number of swollen joints (out of 28: 20 hands joints and 2 joints each of shoulder, wrist, elbow and knee), number of tender joints, erythrocyte sedimentation rate or C-reactive protein and assesses global health assessment. The total DAS28 >5.1 signifies high activity of the disease, between 2.6 and 3.2 reduced disease activity while a score of <2.6 suggests remission.
HAQ-DI[14]
The physical functionality and degree of disability of the patients were assessed using the HAQ-DI that includes 20 questions and calculates a score from 0 to 3 to estimate disability.
Depression, anxiety and stress score (DASS)[15]
The DASS has 42 questions and uses a three scale rating system to measure the severity of symptoms. A score of 9 for depression, 7 for anxiety and 14 for stress is considered normal.
Medical outcomes study 36-item Short Form Health Survey (SF-36)[16]
SF-36 instrument assesses QoL using 36 items grouped into eight elements of physical functioning that is, role limitations or emotional problems, emotional health, social performance, fatigue, bodily pain, overall perception and change in health.
Statistical analysis
The data were entered into Microsoft Excel and analysed by SPSS version 20 for Windows (IBM SPDD Corp; Armonk, NY, USA). Descriptive statistics in the form of frequencies (percentages) were calculated for categorical variables. For quantitative variables, the approximate normality of the distribution was assessed and for variables that followed a normal distribution, mean and standard deviation were reported. The relationship between the disease activity at the time of presentation with the age, degree of disability, depression, anxiety, stress levels as well as the QoL was evaluated using Spearman’s rho correlation coefficient. There is no study evaluating the need of palliative care in patients with RA. Hence, we decided to include 100 patients in this pilot study. All tests were two tailed. P ≤ 0.05 was considered statistically significant.
RESULTS
One hundred patients were studied, of which 90 were female. The median (IQR) duration of diagnosis was 96 months (36–180) [Table 1].
| Parameter | Percentage or mean±SD |
|---|---|
| Age* | 43 (37–55) |
| Duration of diagnosis (months)* | 96 (36–180) |
| DAS28 | 4.33±1.46 |
| HAQ-DI | 0.89±0.71 |
| Depression | 9.55±5.45 |
| Anxiety | 7.75±4.95 |
| Stress | 11.56±5.67 |
| Physical functioning* | 50 (36.3–90.0) |
| Role limitation due to physical health* | 0.0 (0.0–100.0) |
| Role limitation due to emotional problem* | 0.0 (0.0–100.0) |
| Energy/fatigue | 51.85±21.08 |
| Emotional well-being | 61.04±19.29 |
| Social functioning | 62.28±27.09 |
| Pain | 57.43±26.6 |
| General health | 50.35±22.69 |
| Health change* | 50.0 (25.0–75.0) |
| NRS for pain | 5.37±2.5 |
| DAS 28 (%) | |
| Remission (<2.6) | 16 |
| Low disease activity (2.6–3.2) | 4 |
| Moderate disease activity (3.2–5.1) | 50 |
| High disease activity (>5.1) | 30 |
| HAQ-DI | |
| Mild difficulties to moderate disability (0–1) | 61 |
| Moderate-to-severe disability (1–2) | 33 |
| Severe-to-very severe disability (2–3) | 6 |
The majority of the patients were having moderate disease activity (50%) with mild difficulties to moderate disability (61%) in their day-to-day activity [Table 1]. Most of them were managed with a combination of various drugs including methotrexate, folic acid, hydroxychloroquine, sulfasalazine, leflunomide, prednisolone, calcium, naproxen and diclofenac. Out of all, 32% of the patients were suffering from mild depression, 14% from mild anxiety and 10% from mild stress. Few patients (1–3%) had severe to very severe depression, anxiety or stress [Figure 1].

- Distribution of patients with depression, anxiety and stress as assessed by depression, anxiety and stress score.
There was no significant correlation between the DAS28 and the age of the patient (r = 0.006, P = 0.954). Table 2 depicts the correlation between disease activity and other variables studied. There was a strong correlation between the disease activity and degree of disability, depression, anxiety, stress levels, QoL and NRS score for pain (P = 0.000) [Figures 2-4].
| DAS28 (n=100) | Spearman’s rho correlation coefficient | P |
|---|---|---|
| Age | 0.006 | 0.954 |
| HAQ-DI | 0.816 | 0.000 |
| Depression | 0.671 | 0.000 |
| Anxiety | 0.609 | 0.000 |
| Stress | 0.474 | 0.000 |
| Physical functioning | −0.737 | 0.000 |
| Role limitation due to physical health | −0.662 | 0.000 |
| Role limitation due to emotional problem | −0.676 | 0.000 |
| Energy/fatigue | −0.638 | 0.000 |
| Emotional well-being | −0.605 | 0.000 |
| Social functioning | −0.658 | 0.000 |
| Pain | −0.687 | 0.000 |
| General health | −0.643 | 0.000 |
| Health change | −0.376 | 0.000 |
| NRS for pain | 0.656 | 0.000 |
HAQ-DI: Health assessment questionnaire disability index, NRS: Numeric rating scale, DAS28: Disease Activity Score 28
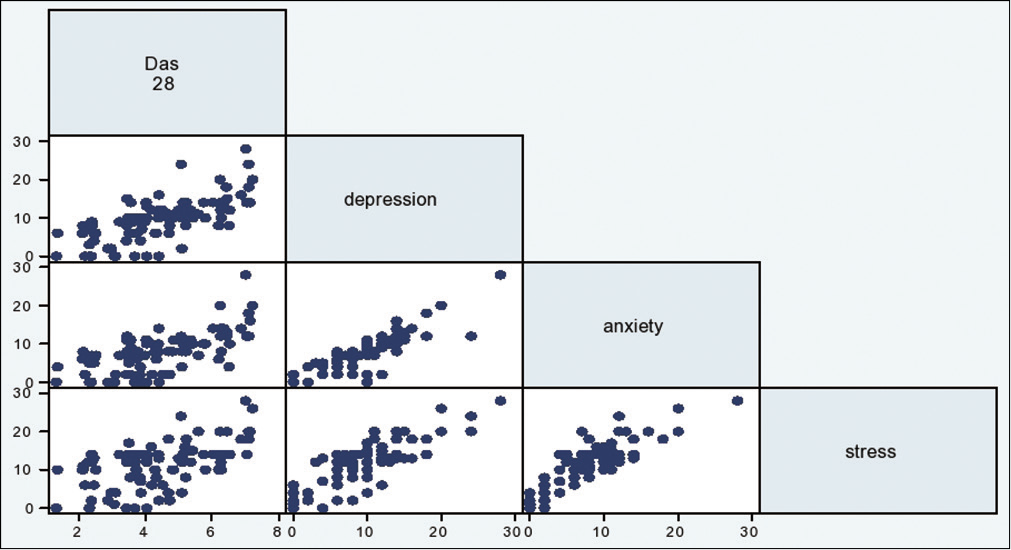
- Correlation between disease activity (Disease Activity Score 28) and depression, anxiety and stress levels.
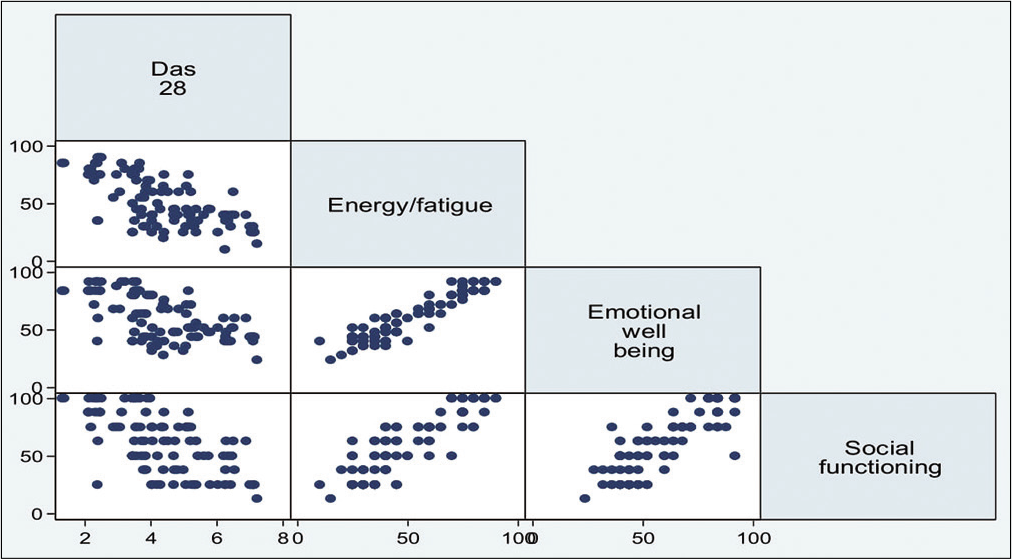
- Correlation between disease activity (Disease Activity Score 28) and quality of life variables energy/fatigue, emotional well-being and social functioning.

- Correlation between disease activity (Disease Activity Score 28) and quality of life variables pain, general health and health change.
DISCUSSION
The management of RA is mainly focused on the control of synovitis and limits the joint injury. Several drugs are used depending on the disease activity and the patient’s response to interventions. Despite all this, the inability to achieve sustained remission in most of the patients leads to poor QoL. In this study, we correlated the level of disease activity with the QoL in patients with RA to assess the need for palliative care services in these patients.
In our study, though most of the patients had moderate disease activity, most of them had only mild-to-moderate disabilities in their daily activities. Disability in RA patients occurs due to the combination of the disease activity, deformity, pain and extra-articular disease. Other components such as age, gender, psychosocial environment and comorbid diseases also influenced the degree of disability experienced by patients. A patient suffering from severe depression along with RA may intensify the pain and its associated disability despite having a low disease activity.[17] This explains the discrepancy between the disease activity and degree of disability seen in our results.
The illness of a person suffering from chronic diseases like RA may follow one of the three trajectories, namely rapid decline, worsening pattern with episodes of decompensation or slowly progressive disability.[18-20] The goal of management is to achieve sustained remission overtime as it will have a better outcome than remission at a single time point.[6,21] If sustained remission is not possible in patients with longstanding disease or multiple morbidities, a low disease activity (DAS28 ≤3.2) is targeted.[22,23]
The unpredictable course of RA makes it difficult for the primary physician to select the patients suitable for palliative care referral and advanced care planning. There is a lack of data assessing the levels of disease activity, degree of disability, depression, anxiety, stress levels and QoL in patients with RA worldwide. Due to chronic nature of the disease, the patient with RA usually lives for decades with a variable course of the disease activity leading to possible disability, systemic involvement of various organ systems, various psychological issues and hence the poor QoL.
Cho et al. reported in patients with rheumatic disease repeated admissions (85%), pain (81.4%), anorexia (80.1%), dyspnoea (77%) and functional decline (64.6%) were common in the last year of their lives but only 15.5% of patients were referred to palliative care physicians. Out of the referred patients, 72% were seen at the time of terminal admission with the median time to referral to the palliative physician being 8 days before death.[8]
In our study, we assessed the level of disease activity, disability, depression, anxiety, stress levels and QoL. Majority of the patients had moderate disease activity (50%) with mild difficulties and moderate disability in their daily activities (61%). Providing these patients, palliative care from the very beginning of the disease trajectory will help improve the QoL. No previous study has compared the disease activity with disability, depression, anxiety, stress levels and QoL.
The literature on the need to integrate palliative care with the branch of rheumatology is scarce. Palliative care physicians are mostly involved during the end-of-life care decisions in non-oncological chronic diseases. We studied the correlation of disease severity with symptom burden, thereby emphasising the need to provide palliative care from the time of diagnosis.
Palliative care intends to reform the QoL. There is often a misconception that a patient receiving palliative care has reached the end stage of life. Early referrals to palliative care physician will not only provide relief of physical symptoms but also give them psychosocial support. It will help develop better communication between the patient and the primary care physician as well as allow a smooth transition from repeated hospital admissions at the terminal stage to home-based care. Hence, it is important to evaluate and provide the best supportive care from the initial stage of the disease based on patients’ need for symptom palliation and psychosocial management, considering the chronic progressive nature of the disease with a median duration of 96 months in our study. This will also help to facilitate early advanced care planning due to the development of good rapport with the patient.
Human beings have specific roles and responsibilities in various life activities. It has been seen that pain and other associated symptoms of arthritis forewarns the ability of a person to engage in day-to-day activities[24] and may compromise the psychosocial well-being.[25] Modern medicine emphasises integrating PROMs in disease management. In our study, the patients with high DAS28 during the initial presentation were suffering from pain, depression, anxiety or stress leading to poor QoL. These findings suggest the need to institute palliative care in rheumatology like other chronic diseases to provide supportive care for the improvement of the function and QoL in patients.
In our opinion, these tools should be used to triage patients according to the symptom burden and help them to consult supportive care before they unexpectedly decompensate. This will also serve as a platform for further studies in the field of palliative care and rheumatology.
Limitations
The study included patients with RA only and the results cannot be generalised to patients with systemic rheumatic diseases. Furthermore, the study was done at a time point to assess the severity of disease and correlate them with QoL parameters. A follow-up may have helped to analyse the effect on QoL and overall patient satisfaction.
CONCLUSION
RA patients with increased disease activity tend to have a higher incidence of depression, anxiety, stress and poor QoL. Palliative care physicians and rheumatologists must work together to provide holistic care to RA patients keeping physical, psychosocial and spiritual domains in mind.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Rheumatoid arthritis: Pathological mechanisms and modern pharmacologic therapies. Bone Res. 2018;6:15.
- [CrossRef] [Google Scholar]
- The global burden of rheumatoid arthritis: Estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:1316-22.
- [CrossRef] [Google Scholar]
- Long-term impact of delay in assessment of patients with early arthritis. Arthritis Rheum. 2010;62:3537-46.
- [CrossRef] [Google Scholar]
- Early medication use in new-onset rheumatoid arthritis may delay joint replacement: Results of a large population-based study. Arthritis Res Ther. 2015;17:197.
- [CrossRef] [Google Scholar]
- Factors associated with time to diagnosis from symptom onset in patients with early rheumatoid arthritis. Korean J Intern Med. 2019;34:910-6.
- [CrossRef] [Google Scholar]
- Sustained remission improves physical function in patients with established rheumatoid arthritis, and should be a treatment goal: A prospective observational cohort study from Southern Sweden. J Rheumatol. 2016;43:1017-23.
- [CrossRef] [Google Scholar]
- Prevalence of sustained remission in rheumatoid arthritis: impact of criteria sets and disease duration, a Nationwide Study in Sweden. Rheumatology (Oxford). 2019;58:227-36.
- [CrossRef] [Google Scholar]
- Palliative and end-of-life care in rheumatology: High symptom prevalence and unmet needs. Semin Arthritis Rheum. 2019;49:156-61.
- [CrossRef] [Google Scholar]
- WHO Definition of Palliative Care. Available from: http://www.who.int/cancer/palliative/definition/en/ [Last accessed on 2016 Apr 09]
- [Google Scholar]
- Progress in assessing physical function in arthritis: PROMIS short forms and computerized adaptive testing. J Rheumatol. 2009;36:2061-6.
- [CrossRef] [Google Scholar]
- Relative performance of commonly used physical function questionnaires in rheumatoid arthritis and a patient-reported outcomes measurement information system computerized adaptive test. Arthritis Rheumatol. 2014;66:2900-8.
- [CrossRef] [Google Scholar]
- 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580-8.
- [CrossRef] [Google Scholar]
- The Disease Activity Score (DAS) and the Disease Activity Score using 28 joint counts (DAS28) in the management of rheumatoid arthritis. Clin Exp Rheumatol. 2016;34:S40-4.
- [Google Scholar]
- Measures of functional status and quality of life in rheumatoid arthritis: Health Assessment Questionnaire Disability Index (HAQ), Modified Health Assessment Questionnaire (MHAQ), Multidimensional Health Assessment Questionnaire (MDHAQ), Health Assessment Questionnaire II (HAQ-II), Improved Health Assessment Questionnaire (Improved HAQ), and Rheumatoid Arthritis Quality of Life (RAQoL) Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S4-13.
- [Google Scholar]
- Manual for the Depression Anxiety Stress Scales (2nd ed). Sydney: Psychology Foundation of Australia; 1995.
- [Google Scholar]
- Measuring disability and quality of life in established rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2007;21:827-40.
- [CrossRef] [Google Scholar]
- How much disability in rheumatoid arthritis is explained by rheumatoid arthritis? Arthritis Rheum. 1999;42:1712-21.
- [Google Scholar]
- Early mortality in a multinational systemic sclerosis inception cohort. Arthritis Rheumatol. 2017;69:1067-77.
- [CrossRef] [Google Scholar]
- Progressive decline of lung function in rheumatoid arthritis-associated interstitial lung disease. Arthritis Rheumatol. 2017;69:542-9.
- [CrossRef] [Google Scholar]
- Sustained remission in rheumatoid arthritis: Latest evidence and clinical considerations. Ther Adv Musculoskelet Dis. 2017;9:249-62.
- [CrossRef] [Google Scholar]
- Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis. 2016;75:3-15.
- [CrossRef] [Google Scholar]
- Treating rheumatoid arthritis to target: Recommendations of an international task force. Ann Rheum Dis. 2010;69:631-7.
- [CrossRef] [Google Scholar]
- Prevalence and predictors of disability in valued life activities among individuals with rheumatoid arthritis. Ann Rheum Dis. 2006;65:763-9.
- [CrossRef] [Google Scholar]






