Translate this page into:
Patient and Health-Care Provider Interpretation of do not Resuscitate and do not Intubate
Address for correspondence: Dr. John Ashurst; E-mail: ashurst.john.32.research@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Advance directives and end of life care are difficult discussions for both patients and health-care providers (HCPs). A HCP requires an accurate understanding of advanced directives to educate patients and their family members to allow them to make an appropriate decision. Misinterpretations of the do not resuscitate (DNR), do not intubate (DNI), and the Physicians Orders for Life-Sustaining Treatment (POLST) form result in ineffective communication and confusion between patients, family members, and HCPs.
Methodology:
An anonymous, multiple choice online and paper survey was distributed to patients, family members of patients (PFMs), and HCPs from December 12, 2012 to March 6, 2013. Data regarding demographics, the accuracy of determining the correct definition of DNR and DNI, the familiarity of the POLST form and if a primary care physician had discussed advanced directives with the participants were collected.
Results:
A total of 687 respondents participated in the survey. Patients and PFMs could not distinguish the definition of DNR (95% confidence interval [CI] [1.453–2.804]) or DNI (95% CI (1.216–2.334)) 52% of the time while HCPs 35% and 39% of the time (P < 0.0005). Regarding the POLST form, 86% of patients and PFMs and 50% of HCPs were not familiar with the POLST form. Sixty-nine percent of patients and family members reported that their primary care physician had not discussed advance directives with them. Twenty-four percent of patients and family members reported that they had previous health-care experience and this was associated with increased knowledge of the POLST form (P < 0.0005). An association was also seen between the type of HCP taking the survey and the ability to correctly identify the correct definition of DNR (P < 0.0005).
Conclusion:
Discussion of end of life care is difficult for patients and their family members. Often times multiple discussions are required in order to effectively communicate the definition of DNR, DNI, and the POLST form. Education of patients, family members, and HCPs is required to bridge the knowledge gap of advance directives.
Keywords
Do not intubate
Do not resuscitate
Physicians Orders for Life Sustaining Treatment
INTRODUCTION
Varying interpretation of do not resuscitate (DNR) by patients, families and staff impacts the DNR consent process in the hospital setting.[1] The misunderstanding of advance directives has been noted among those at the health-care provider (HCP) level, therefore making it difficult for patients and family members to agree on advance directives when they are receiving incongruence of the meaning of DNR.[12] Most often due to illness on hospital admission, a patient may be unable to be his/her own health-care advocate, leaving family members with the difficult decision of end of life care. Regarding end of life care, a shift from the “legal transactional approach” to the “communication approach” over the years has become apparent.[3]
The Physicians Orders for Life-Sustaining Treatment (POLST) form has been recently implemented in many extended care facilities and HCPs are beginning to encounter this form in the emergency department, as well as other areas of the hospital. The POLST form differs from advance care directive/living will, which only applies should a person be deemed to be permanently unconscious or suffering from an end-stage medical condition, which would result in death despite full medical treatment.[4] The POLST form is a medical order, immediately and continually applicable, that dictates one's wishes regarding life-sustaining treatments to be honored in all health-care settings, and is a result of a discussion between the patient/surrogate decision-maker and the physician.[56] If HCPs have a clear and uniform understanding of the POLST form, DNR, and do not intubate (DNI), it can avoid confusion and ensure appropriate concepts are communicated to patient and family members during admission.
We sought to quantify the percentage to which both patients, family members of patients (PFMs) and HCPs misinterpret the advanced directives of DNR and DNI. In addition, this study sought to highlight the overall need for both HCPs and patients to be educated regarding the POLST form.
METHODOLOGY
Study design and population
This study was a prospective survey consisting of patients, PFMs and HCPs in a community teaching hospital. The study was undertaken from December 12, 2012 to March 6, 2013 at Conemaugh Memorial Medical Center in Johnstown, Pennsylvania, USA, after the Institutional Review Board approval.
Study procedures
Eligible participants were 18 years of age or older, were patients or PFMs used English as their primary language and presented to an outpatient registration desk. These individuals were asked to complete a paper copy of the survey [
Statistical analysis
For the purpose of statistical hypothesis testing of DNR and DNI, the answers given to the pertinent questions were coded into a dichotomous response, either incorrect or correct. The survey questions with the correct answers are: “What is the definition of DNR? – No cardiac resuscitation (including chest compressions, electrically shocking the heart, and use of medications to restart the heart)” and “What is the definition of DNI? – no intubation and no mechanical ventilation (breathing tube, breathing machine).” IBM SPSS version 19 (Armonk, NY, USA) was used for all statistical analyses. A Chi-square test of association was applied separately to DNR versus DNI, DNR versus POLST, and DNI versus POLST for both groups.
RESULTS
A total of 687 participants responded to the survey with 474 being HCPs (69%) and 213 (31%) being patients or PFMs. HCP responses consisted of 68.2% registered nurses (322/474), 18.9% attending physicians (89/474), 7.8% resident physicians (37/474), and 5.1% physician assistants (24/474). Sixty-nine percent of patients and family members reported that their primary care physicians had not discussed advance directives with them. Of the patients/family members surveyed, 52% could not identify DNR or DNI correctly (DNR confidence interval [CI] 1.453–2.804 and DNI CI 1.216–2.334), while 35% and 39% of HCPs (n = 474) were unable to correctly define DNR and DNI, respectively (P < 0.0005) [Table 1]. There was a statistically significant association between correctly identifying DNR and years of practice (P < 0.0005) and correctly identifying DNI with the type of health-care provider (P < 0.0005).

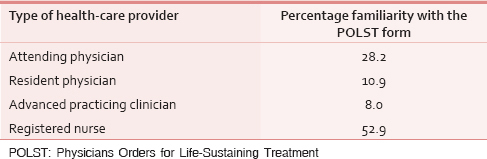
Patients and PFMs were not familiar with the POLST form 86% of the time while health-care workers 50% of the time [Table 2]. Twenty-four percent of patients and PFMs indicated that they had worked as a HCP previously. A Chi-square test found a statistically significant association only between the POLST and previous employment as a HCP (P < 0.0005) and the type of health-care worker (P < 0.0005).
DISCUSSION
As an HCP, one will most likely take part in an end of life discussion with a patient and/or their family members. These discussions occur both in the inpatient and outpatient setting. Fueled by this sensitive and emotional topic, conversations can become time consuming and frustrating for all participants. Providers seek support from colleagues and staff to parallel the information communicated to patients and families. This prospective study illustrates that we cannot rely on another HCP to correctly address DNR/DNI. The knowledge deficiency among HCPs can lead to inconsistent and incorrect information on advance directives being communicated to patients and their family members.
Based upon our study, patients and PFMs do not have a clear understanding of advance directives and require public education on the subject. Quantification of the hypothesized knowledge gap could provide insight into the type and degree of required education for patients, family members, and HCPs. This education, in turn, would allow for more effective communication and implementation of a patient's wishes. By educating patients on the definition of DNR and DNI, they can make informed decisions on their wishes for end of life care, providing an individualized continuity of care by both HCPs and family members in the future. Sixty-nine percent of patients and family members replied that their primary care physicians have never addressed advance directives with them on routine office visits. With education, providers could become more comfortable with the subject matter and in turn be motivated to discuss advance directives with patients.
The POLST form has been recently implemented in many extended care facilities and HCPs are beginning to encounter this form more frequently in than the past. The POLST is aimed at preserving patient dignity and includes comfort measures, supportive and full treatment options for patients to choose from.[7] The POLST form is poised to be a powerful tool in the near future, increasing communication between HCPs and patients. However, the lack of knowledge of the POLST form with patients, PFMs, and HCP could hinder its usage.
Future studies can focus on the same survey to be performed after education of advance directives for both patient/family member and HCPs. Exploration of POLST-ordered comfort measure patients and appropriate utilization of emergency room (ER) resources/decrease in inappropriate transfers to ER could also be area for future studies.
Limitations
This was a single study institution survey study; therefore the applicability of the results may differ in another hospital. Further studies will be necessary to determine if these results are applicable on a more general scale. Due to attending physicians and registered nurses being the majority of HCP responses, we were unable to perform an independent weighing analysis of distribution versus disparity between the groups of HCPs surveyed. Therefore, a supplementary study should be completed on HCPs, so that a statistical analysis can be performed at a higher level of power on stratification of the providers. In addition, the survey did not indicate whether or not the HCP worked in a nonacute as opposed to an acute department, where the subjects of advance directives are more likely to occur.
CONCLUSION
Discussion of end of life care often requires many attempts to effectively communicate the definition of DNR, DNI, and the POLST form to patients and families. A clear and uniform understanding by HCPs would avoid confusion and ensure that appropriate concepts are communicated. This study illustrates the knowledge gap on advance directives (specifically DNR, DNI, and the POLST form) that is present not only in the patient population but also among HCPs. Education is required to bridge the gap of advance directives with the goal of implementing consistent patient end of life care decisions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The meaning of DNR status: Oncology nurses’ experiences with patients and families. Cancer Nurs. 1998;21:212-21.
- [Google Scholar]
- TRIAD III: Nationwide assessment of living wills and do not resuscitate orders. J Emerg Med. 2012;42:511-20.
- [Google Scholar]
- The evolution of health care advance planning law and policy. Milbank Q. 2010;88:211-39.
- [Google Scholar]
- A prospective study of the efficacy of the physician order form for life-sustaining treatment. J Am Geriatr Soc. 1998;46:1097-102.
- [Google Scholar]
- Physician orders for life-sustaining treatment and emergency medicine: Ethical considerations, legal issues, and emerging trends. Ann Emerg Med. 2014;64:140-4.
- [Google Scholar]






