Translate this page into:
Pilot Testing of Triage Coding System in Home-based Palliative Care Using Edmonton Symptom Assessment Scale
Address for correspondence: Dr. Sunil Dhiliwal; E-mail: dr.sunil.dhiliwal@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Home-based palliative care is an essential model of palliative care that aims to provide continuity of care at patient's own home in an effective and timely manner. This study was a pilot test of triage coding system in home-based palliative care using Edmonton Symptom Assessment System (ESAS) scale.
Methods:
Objective of the study was to evaluate if the triage coding system in home-based palliative care: (a) Facilitated timely intervention, (b) improved symptom control, and (c) avoided hospital deaths. Homecare services were coded as high (Group 1 - ESAS scores ≥7), medium (Group 2 - ESAS scores 4–6), and low (Group 3 - ESAS scores 0–3) priority based on ESAS scores. In high priority group, patients received home visit in 0–3 working days; medium priority group, patients received home visit in 0–10 working days; and low priority group, patients received home visit in 0–15 working days. The triage duration of home visit was arbitrarily decided based on the previous retrospective audit and consensus of the experts involved in prioritization and triaging in home care.
Results:
“High priority” patients were visited in 2.63 ± 0.75 days; “medium priority” patients were visited in 7.00 ± 1.5 days, and “low priority” patients were visited in 10.54 ± 2.7 days. High and medium priority groups had a statistically significant improvement in most of the ESAS symptoms following palliative home care intervention. Intergroup comparison showed that improvement in symptoms was the highest in high priority group compared to medium and low priority group. There was an 8.5% increase in home and hospice deaths following the introduction of triage coding system. There was a significant decrease in deaths in the hospital in Group 1 (6.3%) (χ2 = 27.3, P < 0.001) compared to Group 2 (28.6%) and Group 3 (15.4%). Group 2 had more hospital deaths. Interval duration from triaging to first intervention was a significant predictor of survival with odds ratio 0.75 indicating that time taken for intervention from triaging was more significantly affecting survival than group triaging.
Conclusion:
Pilot study of testing triaging coding system in home-based palliative care showed, triage coding system: (a) Facilitated early palliative home care intervention, (b) improved symptom control, (c) decreased hospital deaths, predominantly in high priority group, and (d) time taken for intervention from triaging was a significant predictor of survival.
Keywords
Home-based palliative care
Priority
Triage coding
INTRODUCTION
Patients with advanced life-limiting illness have complex physical and psychosocial issues and need multidisciplinary specialist palliative care input at various clinical settings including home.[1] Studies have showed effectiveness of specialist home-based palliative care with regards to improvement in physical symptoms, psychosocial issues, and quality of life at both urban and rural setting.[23] Early and timely referral to home-based palliative care avoids needless hospital admission at the end of life[4] and people in both developing and developed world, with advanced life-limiting illness, in their last days of life prefer to remain at home.[56] Home-based death is commonly viewed as dignified and comfortable experience than hospital death.[789] In a country like India, lack of expertise in palliative and end of life care and poor access to essential medications for symptom control are important barriers that preclude quality home-based palliative care. To meet the needs of a large patient population and ensure timely intervention, a triage coding system based on patient needs is critical. A retrospective audit of 82 case records in 2010 on effectiveness of triage system in home-based palliative care unit demonstrated triage coding system improved physical symptoms, psychological distress, and family satisfaction. However, retrospective audit of case records of past years in our institution showed that 25–30% of patients referred to home-based palliative care died before the first visit by the home care team and most of these patients died at a hospital in an acute care setting.[10] There are also studies that support the role of triage coding in inpatient admissions and after-hours telephone support.[111213] Hence, this pilot study was conceived intending to evaluate impact of triage coding system on facilitation of timely home visit, symptom control and avoiding needless hospitalization.
METHODS
This was a pilot prospective nonrandomized observational study conducted at a tertiary oncology setting between January 1, 2012, and December 31, 2012. The home care division of the palliative care department services around 500–600 new patients annually.
The aim of the study was to evaluate impact of triage coding system in home-based palliative care. The primary objective was to determine whether triage-coding system facilitates timely intervention. The secondary objectives were if the triage-coding symptom improved symptom control and avoided hospital deaths.
All patients registered under home based palliative care at Tata Memorial Centre and residing within the geographic area of coverage of home care service in the year 2012 were included in the study. Those with physician predicted survival of <4 weeks and those patients who later migrated to territory beyond homecare service were excluded from the study.
Triage coding system
The patients were coded as “high” (1*), “medium” (2*), and “low” (3*) priority.
High priority (1*) code was assigned for patients with scores more than 7 for one or more symptoms in Edmonton Symptom Assessment System (ESAS) scale. These patients were to be seen in 0–3 working days by the home care team. Medium priority (2*) code was assigned for patients with scores between 4 and 6 for one or more symptoms in ESAS scale. These patients were to be seen within 10 working days by the home care team. Low priority (3*) code was assigned for patients with scores between 0 and 3 for one or more symptoms in ESAS scale. These patients were to be seen within 15 working days by the home care team. The triage duration of home visit was arbitrarily decided by the prior retrospective chart studies and experience derived from previous practices in prioritization and triaging.
Intervention
The palliative home care visit team comprised of a palliative care physician, palliative care nurse, and medical social worker. During the initial visit, the multidisciplinary team assessed and managed pain, physical symptoms, and psychosocial issues. Family and caregivers received education and practical demonstration on care of stomas, malignant wounds, and pressure ulcers; management of lymphedema; care of bed ridden patients and mucosa; medication administration; route of administration (subcutaneous access and administration); and adherence (maintaining medication log). The team also facilitated liaison with local general practitioner and provided out of hours telephonic support.
Study tools
Edmonton System Assessment Scale
The ESAS scale is a 9-item patient-rated symptom visual analog scale developed for use in assessing the symptoms of patients receiving palliative care. ESAS is a valid instrument with good test-retest validity with overall Cronbach alpha for the ESAS instrument being 0.79.[1415]
Timelines of measurement
The timelines of measurements were the first and second home visit. During the second visit patients were re-coded as high (1*), medium (2*), or low (3*) priority based on the Edmonton Symptom Assessment Scores.
Outcome measures
The study end points were (1) recording the time taken for the first visit home visit from the point of referral, (2) recording ESAS scores during the first and second home visit, and (3) recording frequency of hospital deaths.
Statistical analysis
Data were analyzed using SPSS version 20 (IBM SPSS Version 20.0, Chicago, Illinois) for windows. Data were not normally distributed for Edmonton symptom rating scale and hence Kruskal–Wallis and Mann–Whitney tests were used to compare triage groups. For interval duration of home care intervention among three groups, a one-way ANOVA was used. For category variables such as hospital death as outcome, a Chi-square test of proportions was used. For survival outcomes, we used the triage groups based on different cutoff scores and duration of interval for home care intervention as predictors in a multiple hierarchical regression model.
Ethics clearance
Tata Memorial Centre, Institutional Review Board, has approved the study.
RESULTS
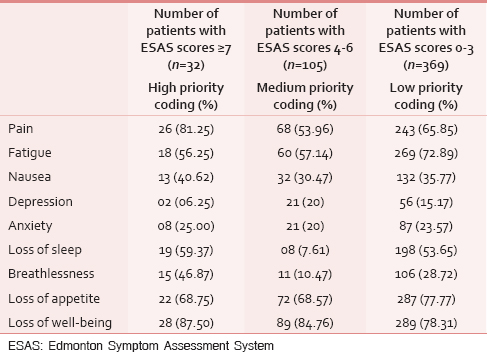
A total of 506 new patients were registered in 2012. As per the triage code criteria, 32 (6.32%) patients were categorized into “High priority” code, 105 (20.75%) into “Medium priority” code, and 369 (72.92%) into “Low priority” code. Table 1 shows patients who were coded into “High priority” patients had at least one ESAS symptom score 7 or above. Most common symptoms that triggered high priority coding was loss of well-being (87.50%), pain (81.25%), loss of appetite (68.75%), sleep disturbances (59.37%), and fatigue (56.25%). “Medium priority” patients had at least one ESAS symptom score between 4 and 6. Most common symptoms that triggered medium priority coding was loss of well-being (84.76%), loss of appetite (68.57%), pain (64.76%), fatigue (57.14%), and nausea (30.47%).
High priority patients were visited in 2.63 ± 0.75 days; medium priority patients were visited in 7.00 ± 1.5 days, and low priority patients were visited in 10.54 ± 2.7 days. The average time taken for home care intervention was significantly less for Group 1 (high priority patients - ESAS scores ≥7) when compared to other groups (P < 0.001).
In both high and medium priority patients, comparison of ESAS symptom scores during the first and second home visits demonstrated a statistically significant improvement in ESAS symptom scores post home-based palliative care intervention [Tables 2 and 3].


Comparison of improvement in ESAS symptoms between high and medium priority group showed that there was a significant decrease in following ESAS symptom scores post home care intervention in pain (P < 0.001), fatigue (P < 0.001), nausea and vomiting (P < 0.001), loss of sleep (P < 0.001), breathlessness (P < 0.001), loss of appetite (P < 0.05), depression (P < 0.05), and loss of well-being (P < 0.001) on Mann–Whitney tests in Group 1 (high priority patients - ESAS scores ≥7) compared to Group 2 (medium priority - ESAS scores 4–6) [Table 4].

Comparison of improvement in ESAS symptoms between high and low priority group showed that there was a significant decrease in following ESAS symptom scores post home care intervention in pain (P < 0.001), fatigue (P < 0.001), nausea and vomiting (P < 0.001), loss of sleep (P < 0.001), breathlessness (P < 0.001), loss of appetite (P < 0.001), depression (P < 0.001), anxiety (P < 0.001) and loss of well-being (P < 0.001) on Mann–Whitney tests in Group 1 (high priority patients - ESAS scores ≥ 7) compared to Group 2 (medium priority - ESAS scores 4–6) [Table 4].
In the year 2012, out of 466 deaths, 377 died at home and hospice when compared to 2011, out of 378 deaths, 275 died at home and hospice. In comparison to 2011, there was 8.5% increase in home and hospice deaths in 2012. There was a significant decrease in deaths in the hospital in Group 1 (6.3%) (χ2 = 27.3, P < 0.001) compared to Group 2 (28.6%) and Group 3 (15.4%). Group 2 had more deaths in the hospital (28.6%) compared to group 3 (15.4%) [Table 5].

A multiple hierarchical logistic regression was conducted to analyze the effects of triaging and duration of the interval for home care from triaging. Group 1 (high priority patients - ESAS scores ≥7) triage emerged as a significant predictor of survival with respect to group triaging with the odds ratio of 0.04. Interval duration from triaging to first intervention was a significant predictor of survival with odds ratio 0.75 indicating that time taken for intervention from triaging was more significantly affecting survival than group triaging.
DISCUSSION
In a resource-limited setting, the burden on the palliative care team is high as there is a paucity of human and financial resources. Our results highlight the need to develop a selection process for triaging patients in the outpatient and inpatient departments referred to palliative home care, so as to provide comprehensive and timely care for the patients. ESAS has been widely used in clinical practice since its introduction and validated as an easy and reliable instrument for the assessment of symptoms in various populations.[12] The clinician and nursing team can thus administer the scale with ease for triaging the patients in the outpatient department. The primary goal of the study was to direct the limited available resources to those who are most likely to benefit from them. Chronic debility, advanced nature of illness, poverty, and enormity of distance to travel to the tertiary hospital often preclude the utilization of hospital palliative care services emphasizing the need for a robust palliative home care service.
The palliative care patients who received community-based domiciliary services required less frequent and shorter hospitalization as compared to the patients not receiving homecare services.[16] A study by Sasha Shepherd et al. demonstrated those patients who received home-based palliative care were more likely to die at home as compared to those receiving usual care.[17]
In our study, with home-based palliative care intervention, we found a significant improvement in the ESAS symptom with a noticeable shift in the triage coding after the home visit. The triage coding at the outpatient and inpatient level was only based on ESAS symptom score, which in turn meant that the patients were prioritized predominantly on the basis of physical symptoms and less on psychosocial issues and distress. Future studies should be directed at coding patients separately on the basis of physical, psychological, social, and spiritual needs and then prioritized, as this will help in providing a holistic approach to care. Training the health care providers to use triage tools will help in standard and unbiased triaging.
Studies show significant cost advantages of palliative care at home as compared to alternative care models of palliative care delivery.[18] In India, annually 39 million families are pushed into poverty due to rising health-related costs, and most of these costs are related to care in an acute hospital setting at the end of life.[19] Hence, palliative care at home, especially in a resource limited setting like India will avoid needless hospitalization and minimize health care-related costs.[4] A survey done in India in a healthy adult population about preference of place of death showed that 83% of the Indians prefer to die at home.[6] However, significant number of patients in India with advanced life-limiting illness die in an acute medical care setting with poorly controlled symptoms and compromised quality of life. Home death is commonly viewed as more dignified and comfortable experience than hospital deaths[7] and patients with cancer who die in a hospital or intensive care unit have worse quality of life as compared with those who die at home, and their bereaved caregivers are at increased risk for developing psychological morbidity.[20]
Studies have shown that patients referred to a specialist palliative care services are likely to receive continuity of care and coordinated care. They are more likely to have local general practitioners, liaison between palliative care team and local general practitioners, and receive out of hours support.[21] Easy access to the health care professionals, better liaisoning of palliative care team with local general practitioners, and the availability of out of hours care boosts patient and family confidence.[22]
This study has shown that triage coding system facilitates timely intervention, improves physical symptoms, and reduces needless hospitalization. The other important outcome of the study was that hospital deaths were highest in medium priority group, showing that medium priority group also need early intervention. Hence, it may be appropriate just to have high and low priority groups. The time taken for intervention from triaging was more significantly affecting survival than group triaging. This accentuates the need to have a better and comprehensive triage tool that can be validated and applied to a larger population. There is no available literature on how to triage patients for home-based palliative care. This pilot study may help us to design larger multicentric studies to address this need.
CONCLUSION
Triage coding system in home-based palliative care:
-
Facilitated timely home based palliative care visit
-
Improved pain and symptom control
-
Avoided hospital deaths, predominantly in high priority group
-
Time taken for intervention from triaging was a significant predictor of survival.
Study limitations
This was a pilot study with a relatively small sample size. Only ESAS was used for triaging. Patients were assessed only on two occasions (first and second home visit) and assessments were not carried out at fixed intervals.
Authors recommend doing a larger study using a standard validated triage-coding tool with assessments done more comprehensively with multiple parameters taken into account at a fixed interval and on multiple occasions.
Financial support and sponsorship
Global Cancer Concern India (GCCI) and Tata Memorial Centre.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are grateful to the patients who participated in this study and acknowledge Global Cancer Concern India (GCCI) and the Tata Memorial Centre for the financial support.
REFERENCES
- Development and validation of a core outcome measure for palliative care: The palliative care outcome scale. Palliative care core audit project advisory group. Qual Health Care. 1999;8:219-27.
- [Google Scholar]
- Assessment of status of patients receiving palliative home care and services provided in a rural area-Kerala, India. Indian J Palliat Care. 2012;18:213-8.
- [Google Scholar]
- Outcome measures in palliative care for advanced cancer patients: A review. J Public Health Med. 1997;19:193-9.
- [Google Scholar]
- Early admission to community-based palliative care reduces use of emergency departments in the ninety days before death. J Palliat Med. 2013;16:774-9.
- [Google Scholar]
- Preparing for the end of life: Preferences of patients, families, physicians, and other care providers. J Pain Symptom Manage. 2001;22:727-37.
- [Google Scholar]
- Preference of the place of death among people of pune. Indian J Palliat Care. 2014;20:101-6.
- [Google Scholar]
- Home-based support for palliative care families: Challenges and recommendations. Med J Aust. 2003;179(6 Suppl):S35-7.
- [Google Scholar]
- Effectiveness of a home-based palliative care program for end-of-life. J Palliat Med. 2003;6:715-24.
- [Google Scholar]
- Home-based palliative care services for underserved populations. J Palliat Med. 2010;13:413-9.
- [Google Scholar]
- Triage system in a high-volume domiciliary palliative care unit in urban India. J Clin Oncol. 2011;29:15. [Suppl; abstr e19663]
- [Google Scholar]
- Improving access to specialist palliative care through a telephone triage service. Eur J Palliat Care. 2011;18:122-5.
- [Google Scholar]
- The development and evaluation of an inpatient palliative care admission triage tool. J Palliat Med. 2010;13:965-72.
- [Google Scholar]
- After-hours telephone triage: A palliative care support service in Australia. Eur J Palliat Care. 2013;20:69-71.
- [Google Scholar]
- The edmonton symptom assessment system (ESAS): A simple method for the assessment of palliative care patients. J Palliat Care. 1991;7:6-9.
- [Google Scholar]
- Home-based advance care programme is effective in reducing hospitalisations of advanced heart failure patients: A clinical and healthcare cost study. Ann Acad Med Singapore. 2013;42:466-71.
- [Google Scholar]
- Hospital at home: Home-based end of life care. Cochrane Database Syst Rev. 2011;7:CD009231. doi: 10.1002/14651858.CD009231
- [Google Scholar]
- Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst Rev. 2013;6:1-279. doi: 10.1002/14651858.CD007760.pub2
- [Google Scholar]
- Place of death: Correlations with quality of life of patients with cancer and predictors of bereaved caregivers’ mental health. J Clin Oncol. 2010;28:4457-64.
- [Google Scholar]
- A method for defining and estimating the palliative care population. J Pain Symptom Manage. 2006;32:5-12.
- [Google Scholar]
- Providing palliative care in primary care: How satisfied are GPs and district nurses with current out-of-hours arrangements? Br J Gen Pract. 2000;50:477-8.
- [Google Scholar]






