Translate this page into:
Preference of the Place of Death Among People of Pune
Address for correspondence: Dr. Priyadarshini Kulkarni; E-mail: priyadarshini.kulkarni@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
Provision of end-of-life care requires that we have adequate information about the preferred place of death in the population. Since no such study is reported in India, this study was taken up in and around Pune, a large cosmopolitan city.
Setting and Design:
A questionnaire was designed in three parts and distributed among the people above the age of 18 in and around Pune.
Materials and Methods:
The questionnaire had three parts the first being a consent form, followed by one for collection of personal information and lastly questions specific to the subject matter. Filled forms were screened for inconsistencies, gaps of information and errors.
Results:
The population survey was mixed, both urban and rural, men and women, educated and uneducated, young and old. Despite this heterogeneity, the results were consistent to the point that most of the people surveyed preferred home as the place of death. This preference cuts across all barriers, the only difference being that women had a stronger preference for home death compared to men.
Conclusions:
Helping people to die at their preferred place is a part of end-of-life care. Majority of people surveyed by us, prefer to die at home, where they are relatively more comfortable. Public and governmental policies should be directed toward facilitating home deaths.
Keywords
Death
End-of-life
Palliative care
Place of death
INTRODUCTION
‘In this world nothing can be said to be certain, except death and taxes’ wrote Benjamin Franklin in a letter to Jean-Baptiste Leroy. Among the many possible events that may occur in an individual's life, none is as certain as death. None the less most people believe that death shall visit others, but not themselves. An outcome of this thought is that most people are not prepared for death at any stage of life, nor do they think of their place of death.
The care of its sick members is the hallmark of a civilized society. Governments of most countries ensure that their citizens have adequate access to institutions where they are treated when sick. Many countries are now making arrangements for end-of-life care for their people depending upon their choice. Helping people end their life at the place they prefer is considered as an extension of health care services. Information on preferred place of death is essential to organize these facilities at hospices, hospitals, or in the community. Walker, Read, and Priest[1] suggest that current good health-care practice suggests that end-of-life care includes choosing a place for death.
Surveys have been conducted elsewhere to elucidate the preferences of different groups of people about the place of death by Walker and co-workers[2] and delivery of end of life care by Mwangi-Powell, Powell and Harding.[3] Initiating discussions about death is challenging, but progress in medical technology, which leads to increasingly complex medical care choices, makes this imperative. Teno[4] agrees that such surveys are fraught with procedural difficulties that may be circumvented by using a retrospective design of studies; however, Ko et al.[5] point out that such research suffers from problems of reliability and validity, though winning on procedural simplicity.
Many of the surveys such as those by Ishikawa et al.[6] have focused on patients and some, such as the one by Brogaard et al.[7] on terminal cases of cancer. There are a few studies on mixed populations comprising patients and healthy subjects too, such as the one by Yamagishi et al.,[8] while others such as Fukui et al.[9] have focussed on a healthy population. These studies take care of the possible differences of opinion between the sick and the healthy members of the population. However, little is known about the preference of place of death in India and the developing world. A search of the relevant literature failed to reveal any study from the Indian subcontinent.
The present study was sponsored by the Cipla Palliative Care and Training Centre, Warje, Pune with multiple objectives. Primarily, we wanted to know if the Indian population thinks about their own death and factors that might induce such thoughts. Secondly, we wanted to know the preferred place of death and the differences if any that exist among the sub-populations toward the same.
Morhaim and Pollack[10] cite examples of countries where advanced directives are commonly used and are legally binding. These directives help doctors in decision making during medical crises and end-of-life care. In the absence of a clear cut legal position of advanced directives in India, the people have no option of recording their wishes about their end-of-life care. When the time for end-of-life care comes, most people lack the autonomy of ensuring that their wishes are followed, this makes it all the more necessary to record their wishes about the end of life.
Planning a survey on preference of place of death poses logistic and ethical questions. There is a debate over the type of population to be included in the survey. The healthy, the sick, the terminally ill patients, or a mixed population could be studied as has been elsewhere. For an initial study, we preferred a mixed population from the society, which consists of mostly healthy, and some sick people. Subsequent studies could be conducted on specific sub-groups of the population.
There is a dilemma about the age group selected for the study. Asking children this question is certainly not ethical, nor is ethical to ask this of the very old, though both these groups may require end of life care as suggested by Griffith et al.[11] We also need to consider the availability of subjects to conduct the survey. Older adults are generally busy in their professions and may not have time to devote to answering questions of the volunteers, while students have the time and inclination. Exposure to death of near and dear ones has been known to impact the way of thinking and even make more palpable changes in the people's life. Bereavement is known to cause a significant impact on an individual and even modify the life. Whyte et al.[12] and Dietz et al.[13] studied the impact of the death of parents; while Duggleby et al.[14] and Yopp and Rosenstein[15] studied the impact of the death of a spouse. Rostila et al.[16] investigated the effect of sibbling's demise while Yeates et al.[17] studied the effect of children's death on parents, and Creighton et al.[18] showed that people are more profoundly affected by the death of friends than that of other relatives. Digiacomo et al.[19] showed that the impact of the death is more pronounced if the respondents have been closely involved in care giving during the illness.
Shah et al.[20] showed that in some instances bereavement leads to change in attitudes, while Herberman Mash, Fullerton and Ursano[21] demonstrated changes in physical health. Rostila et al.[22] showed that the death of a close one could lead to serious medical conditions and sometimes death. Bereavement is known to affect people who are related to the deceased and at times even those who are not related to the deceased (Mathews et al.[23] and Nazarko[24] ). Health-care professionals though long exposed to disease and death, are also affected by deaths of those under their care as observed by Plante and Cyr.[25] Death of colleagues was noted by Toblin et al.[26] to have profound effects especially when they are brothers in arms.
While planning the survey all these factors were considered. It was decided to conduct the survey so that the study has adequate power to differentiate between the responses at a confidence level of 99% with a confidence interval of 5. The required figure is 666. We predicted a minimum of four sub groups for analysis and hence were keen to have a minimum of 2640 subjects. Given the known inaccuracies in collecting and recording survey data it was decided to study at least 3300 (with room for 25% of questionnaires returning unusable data).
MATERIALS AND METHODS
This study used a survey methodology to elicit responses from the chosen population. The geographic area for the survey was in and around the city of Pune located between 18° 32"North latitude and 73° 51"East longitude. Pune is the sixth largest metropolis of India, and was established way back in 847 AD. The city of Pune is administered by the Pune Municipal Corporation (PMC), and to the northwest lie Pimpri and Chinchwad, which are in Pune Metropolitan area but administered by the Pimpri Chinchwad Municipal Corporation (PCMC). There is virtually no boundary between the areas of PMC and PCMC, and the city is one single contiguous block. Hence, it is virtually impossible to exclude citizens of PCMC while collecting a sample from PMC area. In any case there is no known difference in the populations in these areas, which could affect the results.
A questionnaire was developed which contained three parts. The first was the information sheet, which explained the basic objectives of the survey. The respondents were explained that there were no ‘right’ or ‘wrong’ answers to any questions, but answers were based on experiences and perspectives. The next part was the informed consent. This was the detachable portion and contained the identity of the respondent along with a code number. The final part was the questionnaire which carried only the code number but no other identity of the respondent. This part also collected the demographic information of the respondent followed by death-related questions.
Two languages are mainly used in the PMC and PCMC area. One is the regional language Marathi and the other being English. The entire questionnaire was translated into Marathi; however, no back translation was required since our staff and volunteers were familiar with these languages and agreed that the translation was faithful and acceptable.
The Ethics Committee of the Chest Research Foundation, Pune, was approached for ethical clearance of the study. The committee provided a written approval to the study.
Volunteers who conducted the study, were from our center, educational institutes and research students. They were trained to conduct the survey in a half day training session. They were provided with the printed questionnaires and guided about the areas they could survey. On receipt of the filled forms, the consent form was separated and filed separately. The rest of the questionnaire was sent for data entry.
The data from the forms were entered in Microsoft Excel. Data validation was done using available tools to eliminate erroneous or questionable data. The balance data was analyzed using conventional statistical methods.
RESULTS
Sample characteristics
This was a large survey, conducted with the help of a number of volunteers both within and without the organization. Despite the training and their dedication some of the responses were not complete. In many questionnaires few questions were left blank. Such questionnaires were excluded from analysis of individual parameters.
A total of 3440 respondents were approached for the survey, of these 1457 were male and 1983 were female.
Age
While an attempt was made to record the age of all responders accurately, age details were available in only 3189 responders. Thus, data was available and accurately recorded in 92.7% responders. The lowest age was 18 years while the highest was 88.3 years. The average age of the population was 35.27 years and the median age was 30.2 years.
Income
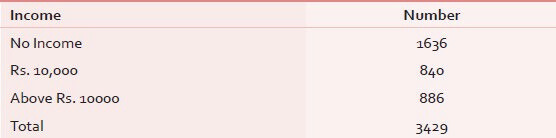
Of the total responders 67 did not give any information about their income. The largest group was one which had no income (it must be clarified that housewives are generally included in this group, though this inclusion may not be justified). Of the earning respondents about half had an income of less than Rs. 10,000 per month while half had an income exceeding that [Table 1].
Discussion about death
A majority of our respondents (59%) stated that they were comfortable discussing about death in general. However, a lower percentage (52%) had actually discussed death in general with friends and family, and only 41% admitted to having discussed their own death.
Exposure to death
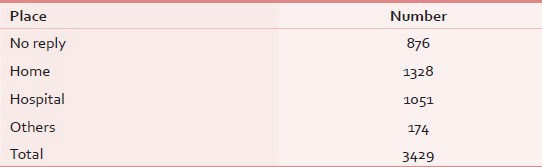
A majority of our respondents (75%) had gone through the experience of death among those close to them, while 25% had not. Most of these deaths had taken place more than 2 years prior to filling the questionnaire. The place where the deaths took place is shown in Table 2. Table 3 shows the relation of the deceased with the respondent and the impact of the death on the respondent.

In a majority of cases the death was due to illness (68%) and over half of the respondents were involved in care giving (62%). Each death, whether of a parent or other relatives made the respondents think of their own death, but the percentage was steady and did not vary. It appears that in each group between 50% and 60% thought of death as a result of any death in their relatives or friends, and 41% even pondered about the preferred place of death.
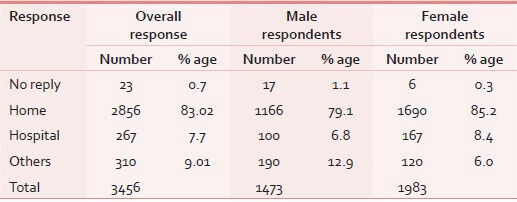
The preferred place of death for the entire survey population was home (83%) followed by elsewhere (9.2%) and lastly hospital (7.7%). It was noted that the preference for home was slightly greater in female respondents (85.2%) as against males (79.1%), as shown in Table 4.
DISCUSSION
Care of the dying is one of the core aspects of palliative care. Supporting the patient and honoring his/her last wishes gives dignity to death, which the disease cannot take away. For many patients of cancer this is the least that can be done in a country where palliative care is so thinly spread. The vulnerability of such patients is so extreme that no decisions are left to the patient, everything from where is the patient to be treated, to where he is to die is decided by others. It is time that the patient is allowed to exercise his choice at least in the place of death.
Advanced Directives are not common in our country, neither are they legally enforceable. There is little patients can do to protect their interests as they slip down the slope toward death, losing their autonomy steadily as they go nearer and nearer to death. It is essential that we ask the patients for their preference for place of care and death.
An overwhelming majority of our respondents preferred the place of death at home. Overall the choice of home was noted in 83.02% of all responders as shown in Table 4. Among women the preference for home was seen in 85.2% while in men this preference was voiced by 79.1% respondents. The difference was minor and not statistically significant, yet such differences have been found by others too.
In our sample there was a bias toward younger population. This could be because most of volunteers were young; they chose respondents of their own age group. There is also a greater and easier availability of the younger respondents. A volunteer visiting an educational institute would find large number of youngsters who are willing to take the survey, hence the bias.
A large number of studies have been conducted, elsewhere in the world, and an overwhelming majority of respondents was found to wish to die at home. In Germany, 98% of dementia patients and 77.5% of their relatives preferred to die at home as reported by Pinzon et al.[27] In the same country, 93.8% of healthy people wanted to die at home, 0.7% in a hospital, 2.8% in palliative care setting, 2.4% in a nursing home, and 0.3% elsewhere as reported by Escobar Pinzon et al.[28] In the US Fischer et al.[29] reported that 75% of hospitalized patients preferred to die at home while Wilson[30] reported that in Canada 70.8% of people preferred to die at home. Miccinesi et al.[31] found that 67% of patients with advanced cancer in Italy preferred to die at home, and Brogaard et al.[7] found preference for home death among 71% of Danish cancer patients. As per the observations of Becarro et al.,[32] there was a wide difference between the preferred place and the actual place of death among Italian patients, they suggested that policymakers should ensure healthcare providers to meet patients preferences, making conditions conducive to home deaths. Gomes et al.[33] conducted a multinational telephonic survey and found that the preference for home death was 51% from Portugal and above 70% in Netherlands, Flanders, Spain Germany and England. They identified conditions and values as factors that influence the preference for the place for dying, but not experiences of death or dying. In a large survey in Japan Yamagishi et al.[8] found that about 50% showed a preference for home both among the general population and among cancer patients. Fukui et al.[9] found in another survey in Japan that 44% of the general population preferred home, 15% preferred hospital, 19% preferred palliative care unit, 10% preferred public nursing home, 2% preferred private nursing home, and the remaining 11% was unsure about their preferred place of death.
Neergaard et al.[34] investigated where Danish cancer patients preferred to die and whether this preference changed during the course of palliative care. The preferred place of death was home for 80.7% of patients, but during palliative care this preference weakened to reach 64.4%. In Turkey, 63% of patients stated that they would like to know all the details about their disease and they preferred a sudden, painless death, without any intervention at the last moment, but Durusoy et al.[35] found that their preference was for a hospital death, result quite contrary to those observed elsewhere.
In many counties including the UK, a low percentage of patients achieve their desire for dying at the place of preference and hence an attempt is being made to discharge the patients in time to die at home as reported by Moback et al.[36] The efficacy of the end-of-life healthcare strategy of the UK Department of Health was evaluated by Gerrard et al.[37] The preferred place of care (PPC) wishes were ascertained for 87% of the patients seen by the team. The PPC was achieved in 76% of cases. The number of patients wishing to die in hospital significantly increased over the audit cycle (from 10% to 30%) over a period of 2 years.
To date we have not found a single study on the preferred place of death having been conducted in India or other countries of the subcontinent. The present study stands out in this respect, and is the first of its kind. Since India differs from most countries where studies on preference of place of death have been conducted, we were not really sure of what Indian data would reveal. The economic conditions, availability of medical support, family networks are so greatly different that we expected a totally different result but were surprised that our results showed little difference from that of many countries.
The results demonstrate that human preferences are similar in many parts of the world, and there is little if any, difference in the preference of people when it comes to the desired place of death. The study reveals that end of life preferences are not influenced by geography, politics, religion, economics, medical facilities or culture. Barring Portugal and Turkey, people across the world seems to prefer home as the preferred place of death. We are all human, and at least towards the end of life, we think alike.
Very often there is little congruence between the wishes of the patients and those of care givers. While patients would like end-of-life care at home, not all care givers are comfortable. Care givers are often aware of their own shortcomings in terms of expertise, or of their ability to provide adequate medication or supportive therapy. Increasing patient-family congruence on preferred place of death not only requires knowledge of the patient's prognosis and advance planning by both parties but also making available the equipment and medication for terminal care. Tang et al.[38] suggest that support to family caregivers will ensure that managing patients dying at home does not create an intolerable burden for family caregivers.
There is a difference between the place of care and place of death notes Agar et al.,[39] in so far as patient's preference seems to be concerned. In an idealist situation, most patients will be taken care of at home and will die at home. Medical facilities are better in the western and developed world, the high doctor to patient ratio, the easy availability of hospital beds and the round the clock services that are affordable, in addition to almost 100% insurance coverage. These make conditions in these countries incomparable to those in India, yet governmental efforts should continue toward helping patients die at the place they prefer.
Home is where we are most comfortable, and in times of crises we would like to be back home. We return to this place to celebrate and mourn, it is strange that home is also synonymous with death. In prose and verse, home has been compared with the eventual resting place. Rabindranath Tagore's ‘The Home Coming’ allegorically defines the final destination as home, while the following lines adorn the gravestone of RL Stevenson.
This be the verse you grave for me
Here he lies, where he longed to be
Home is the sailor, home from sea
And the hunter, home from the hill
It is hardly surprising that most patients want to go home.
CONCLUSIONS
The structured survey among general population in and around Pune, revealed that majority of the respondents prefer home, as the place of death. The next preference is for a hospital, and more women prefer home than men. However age, income, education, and prior exposure to death do not seem to have any bearing on this. Since helping patients reach their end at the place of their preference is one of the components of health care, all efforts should be made to help more and more people die at home.
ACKNOWLEDGMENTS
The authors are thankful to Cipla Palliative Care and Training centre for sponsoring the study and supporting the authors during the study.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- An audit around preferred place of death: One UK hospice experience. BMJ Support Palliat Care. 2011;1:226-7.
- [Google Scholar]
- Identifying, documenting, and reviewing preferred place of death: An audit of one UK hospice. Int J Palliat Nurs. 2011;17:546-51.
- [Google Scholar]
- Models of delivering palliative and end-of-life care in sub-Saharan Africa: A narrative review of the evidence. Curr Opin Support Palliat Care. 2013;7:223-8.
- [Google Scholar]
- Measuring end-of-life care outcomes retrospectively. J Palliat Med. 2005;8(Suppl 1):S42-9.
- [Google Scholar]
- EURO IMPACT. Awareness of general practitioners concerning cancer patients' preferences for place of death: Evidence from four European countries. Eur J Cancer. 2013;49:1967-74.
- [Google Scholar]
- Family preference for place of death mediates the relationship between patient preference and actual place of death: A nationwide retrospective cross-sectional study. PLoS One. 2013;8:e56848.
- [Google Scholar]
- Congruence between preferred and actual place of care and death among Danish cancer patients. Palliat Med. 2013;27:155-64.
- [Google Scholar]
- Preferred place of care and place of death of the general public and cancer patients in Japan. Support Care Cancer. 2012;20:2575-82.
- [Google Scholar]
- Japanese people's preference for place of end-of-life care and death: A population-based nationwide survey. J Pain Symptom Manage. 2011;42:882-92.
- [Google Scholar]
- End-of-Life care issues: A personal, economic, public policy, and public health crisis. Am J Public Health. 2013;103:e8-10.
- [Google Scholar]
- Determining what is in the best interests of a critically ill child. Br J Nurs. 2013;22:112-3.
- [Google Scholar]
- Medical students' experience of personal loss: Incidence and implications. BMC Med Educ. 2013;13:36.
- [Google Scholar]
- Cortisol response to social stress in parentally bereaved youth. Biol Psychiatry. 2013;73:379-87.
- [Google Scholar]
- The quality of life of male spouses of women with breast cancer: Hope, self-efficacy, and perceptions of guilt. Cancer Nurs. 2014;37:E28-35.
- [Google Scholar]
- A support group for fathers whose partners died from cancer. Clin J Oncol Nurs. 2013;17:169-73.
- [Google Scholar]
- Mortality from myocardial infarction after the death of a sibling: A nationwide follow-up study from Sweden. J Am Heart Assoc. 2013;2:e000046.
- [Google Scholar]
- Poor psychological wellbeing particularly in mothers following sudden cardiac death in the young. Eur J Cardiovasc Nurs. 2013;12:484-91.
- [Google Scholar]
- After the death of a friend: Young men's grief and masculine identities. Soc Sci Med. 2013;84:35-43.
- [Google Scholar]
- The effect of unexpected bereavement on mortality in older couples. Am J Public Health. 2013;103:1140-5.
- [Google Scholar]
- Complicated grief and bereavement in young adults following close friend and sibling loss. Depress Anxiety. 2013;30:1202-10.
- [Google Scholar]
- Fatal stroke after the death of a sibling: A nationwide follow-up study from Sweden. PLoS One. 2013;8:e56994.
- [Google Scholar]
- Traumatic death at work: Consequences for surviving families. Int J Health Serv. 2012;42:647-66.
- [Google Scholar]
- Health care professionals' grief after the death of a child. Paediatr Child Health. 2011;16:213-6.
- [Google Scholar]
- Grief and physical health outcomes in U.S. soldiers returning from combat. J Affect Disord. 2012;136:469-75.
- [Google Scholar]
- Dying with dementia: Symptom burden, quality of care, and place of death. Dtsch Arztebl Int. 2013;110:195-202.
- [Google Scholar]
- Where do you want to spend your last days of life. Low concordance between preferred and actual site of death among hospitalized adults? J Hosp Med. 2013;8:178-83.
- [Google Scholar]
- The preferred place of last days: Results of a representative population-based public survey. J Palliat Med. 2013;16:502-8.
- [Google Scholar]
- End-of-life preferences in advanced cancer patients willing to discuss issues surrounding their terminal condition. Eur J Cancer Care (Engl). 2012;21:623-33.
- [Google Scholar]
- ISDOC Study Group. Actual and preferred place of death of cancer patients. Results from the Italian survey of the dying of cancer (ISDOC) J Epidemiol Community Health. 2006;60:412-6.
- [Google Scholar]
- PRISMA. Preferences for place of death if faced with advanced cancer: A population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Ann Oncol. 2012;23:2006-15.
- [Google Scholar]
- Preference for place-of-death among terminally ill cancer patients in Denmark. Scand J Caring Sci. 2011;25:627-36.
- [Google Scholar]
- Cancer patients› satisfaction with doctors and preferences about death in a university hospital in Turkey. Patient Educ Couns. 2011;85:e285-90.
- [Google Scholar]
- Evaluating a fast-track discharge service for patients wishing to die at home. Int J Palliat Nurs. 2011;17:501-6.
- [Google Scholar]
- Achieving the preferred place of care for hospitalized patients at the end of life. Palliat Med. 2011;25:333-6.
- [Google Scholar]
- Determinants of patient-family caregiver congruence on preferred place of death in Taiwan. J Pain Symptom Manage. 2010;40:235-45.
- [Google Scholar]
- Preference for place of care and place of death in palliative care: Are these different questions? Palliat Med. 2008;22:787-95.
- [Google Scholar]






