Translate this page into:
Prescription Pattern of Analgesic Drugs for Patients Receiving Palliative Care in a Teaching Hospital in India
Address for correspondence: Ms. Vishma Hydie Menezes; E-mail: vishmahmenezes@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Drugs used in the palliative care unit for managing symptoms are major contributors toward the expenditure occurring in palliative care. This study was conducted to understand the prescription pattern of analgesic drugs in the patients who are receiving palliative care in a teaching hospital in India by a retrospective study of case records.
Methods:
Case record based, retrospective, descriptive study was conducted at the Pain and Palliative Care Department of St. John's Medical College Hospital, Bengaluru. Case record files of all patients referred to Pain and Palliative Care Department for the treatment of pain in the year of 2012 were studied. Patients’ age, gender, diagnoses, numerical pain rating scale (0–10), drugs prescribed, dosage, frequency, route of administration were recorded. The difference in drug utilization between the genders was done using Chi-square test. Data were collected from 502 patients of which 280 (56%) were males and 222 (44%) were females. Twelve percent of patients had mild pain (1–3), 34% had moderate pain (4–6), and 54% had severe pain (7–10). The most commonly used analgesic drugs were opioids (47%), followed by nonsteroidal anti-inflammatory drugs (36%). The opioids used were tramadol (56%), and morphine (38%). Ninety percent of patients with numerical pain scale more than 6 received morphine. There was no difference in analgesic drug utilization with regards to gender. Prescription pattern differed depending on the severity of pain. Opioids were the most commonly used drugs for pain management.
Conclusion:
The study shows that prescription pattern in palliative care unit of this hospital was in accordance with WHO pain management guidelines. The study showed the current trend in prescription of analgesic drugs in the teaching hospital where the study was conducted.
Keywords
Analgesic
Drug utilization
Palliative
INTRODUCTION
Drug utilization studies mainly emphasize on the factors related to prescription and dispensing the medication, administration and intake of medication, and the associated events. Drug utilization studies play an important role to evaluate if the drugs used are rational or not and also help to take right decision in the healthcare sector.[1] Pain is often considered as the fifth vital sign and can explain a lot about the health condition of a person.[2] Reports indicate that significant numbers of people in the world are suffering because of lack of standardized scientific treatment plans for pain mainly due to the ignorance of physicians and lack of awareness for effective treatment strategies. Correct diagnosis and adequate treatment of pain is crucial for the well-being of the patients suffering from acute and chronic pain.[3]
The aim of palliative care is to provide the highest quality of life possible for patients with their disease conditions. In this endeavor, pain management plays a vital role. It helps patients to be pain-free or helps insufficient control of the pain, so that pain does not hamper with their ability to function or detract from their quality of life.[4] Pain management is beneficial to the patients in various aspects. In cases of patients with acute postoperative pain treated with adequate analgesic schemes, improved outcomes have been found. In patients with chronic pain, pain management can help to maintain or to improve quality of life.[5]
METHODS
A retrospective, case record based descriptive study was conducted at Pain and Palliative care Department of St. John's Medical College Hospital, Bengaluru, India. Case record files of all patients referred to Pain and Palliative Care Department for pain treatment in the year of 2012 (January 1 to December 31) were studied. Patient's age, gender, diagnosis, numerical pain rating scale (0–10), drugs prescribed, were recorded. In numerical pain rating scale 1–3 was considered as mild pain, 4–6 as moderate, 7–10 as severe pain.[6] Use of drugs for pain management with regard to age and numerical pain rating scale was ascertained in terms of percentage.
RESULTS
Data were collected from 502 patients of which 280 (56%) were males and 222 (44%) were females. Out of 502 patients, 32 patients belonged to the age group of 10–20 years, 87 patients belonged to the age group of 21–40 years, 218 patients belonged to the age group of 41–60 years and 165 patients were 61 and above years old. Maximum patients who received analgesic drugs in Palliative Care Department were of age group 41–60 years. In the age group of 41–60 years, 107 were male patients and 111 were female patients. There was no difference in analgesic drug utilization with regards to gender. Age and gender distribution of patients who received analgesic drugs is shown in Figure 1.
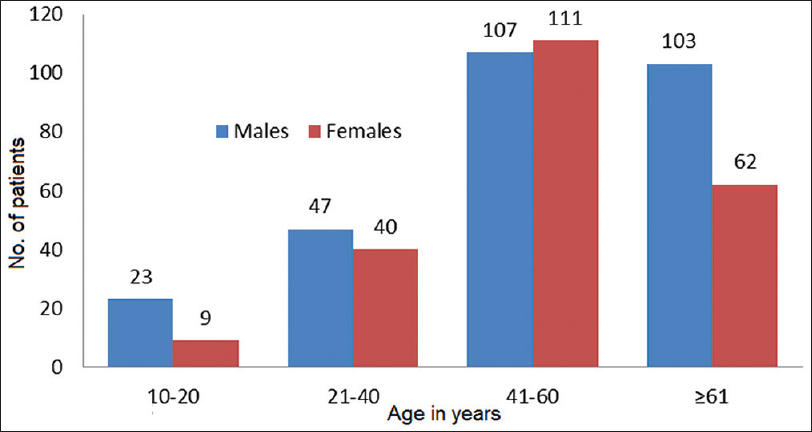
- Age and gender distribution of patients who received analgesic drugs (n=502)
Mild pain was reported by 60 (12%) patients, moderate pain was reported by 170 (34%) patients and severe pain was reported by 272 (54%) patients. For cancer-related pain 354 (70.5%) patients visited Palliative Care Department, followed by 63 (12.5%) patients for neuropathic pain due to amputation, trigeminal neuralgia, multiple sclerosis, etc. In our study, 3.5% of the patients with viral and fungal infection visited Palliative Care Department for the treatment of pain, which mainly included patients with human immunodeficiency virus infection and herpes infection. Different causes of pain in palliative care patients are shown in Figure 2.

- Causes of pain in palliative care patients
A total of 360 patients were prescribed nonsteroidal anti-inflammatory drugs (NSAIDs). Opioids were prescribed to 322 patients, anticonvulsants to 92 patients. Tricyclic antidepressants (TCAs) were prescribed to 52 patients and corticosteroids to 92 patients. Prescription of different groups of analgesic drugs for different age groups is given in Table 1.

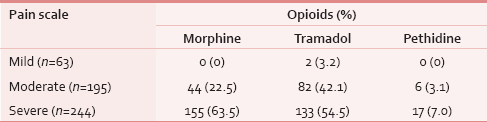
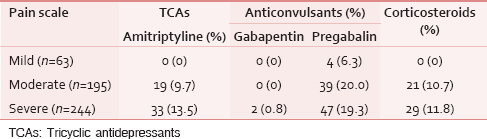
In our study, 57.1% (36 of 63) of patients with mild pain received paracetamol as the analgesic drug. In case of moderate pain, 56.9% (111 of 195) patients received paracetamol followed by 42.1% (82 of 195) patients received tramadol. Out of 244 patients with severe pain 67.6% (165 of 244) of patients have received paracetamol and 63.5% (155 of 244) of patients have received morphine. Tramadol was received by 54.5% (133 of 244) patients with severe pain. Our study showed 17 patients (7%) with severe pain and 6 patients (3.1%) with moderate pain had received pethidine for a short duration. The patients who received pethidine were patients with burns. Prescription of various analgesic drugs based on pain rating scale is given in Tables 2–4.

Two fixed drug combinations were used. Prescription of fixed drug combinations of analgesic drugs among patients is shown in Table 5.

DISCUSSION
This study revealed that majority of the patients who received palliative care for pain had reported severe pain. The demographic results of patients over a period of 12 months revealed that majority of the patients who received palliative care were of age group 41–60 years. The major cause for pain among patients who visited palliative care unit was cancer. According to WHO pain ladder (1986) in mild pain, nonopioids ± adjuvants (include TCA, anticonvulsants, and steroids) are recommended. In moderate pain, weak opioids ± nonopioids ± adjuvants and in severe pain, strong opioids ± nonopioids ± adjuvants are recommended.[7]
Our study revealed that 64.14% patients received opioids as analgesic drugs. In our study, tramadol was the most frequently prescribed opioid. Different factors contribute toward the widespread use of tramadol by the prescribers, primarily the knowledge regarding tramadol's effectiveness. The other important factor is a lower incidence of respiratory depression shown in tramadol when compared with other opioid agonists.[5] In our study, 63.5% of patients with severe pain had received morphine. A study by Thota et al. had shown 52% of patients had received correct dose of morphine. Morphine was received by 31.5% of the patients with severe pain.[7] Our study showed an association between strength of analgesic and intensity of pain: More intense pain resulted in a stronger drug. In addition to NSAIDs, anticonvulsants and TCAs were prescribed to treat neuropathic pain. Fixed drug combination of tramadol and paracetamol was frequently used to treat mild and moderate pain. Depending on the severity of pain and the improvement after initiating the treatment, doses of the analgesic drugs were adjusted and treatment was modified by addition of analgesics or replacement of one analgesic with another depending on patients’ clinical condition.
In our study, paracetamol was the most commonly used NSAID for pain treatment. Axelsson et al. in their study have shown that addition of paracetamol to existing opioid therapy had enhanced analgesic effects in cancer patients.[8] Our study showed that for limited number of patients with burns, pethidine was used for short duration. Study conducted by Gallagher et al. mentioned the use of pethidine for short duration in patients with burns. Due to the accumulation of a toxic metabolite long-term use of pethidine is contraindicated.[9]
It has been suggested that a specialist hospital palliative care team can significantly improve pain management. The availability of such teams can help the physicians to evaluate and coordinate the treatment program.[10] Appropriate assessment of pain plays a vital role in the appropriate management and relief of pain. Doctors should evaluate the frequency, cause, severity of pain. Healthcare professional should know differentiation between different types of pain. If pain assessment is adequate, appropriate treatment can be given. Adequate and rational use of analgesic drugs is the cornerstone in management of pain in patients receiving palliative care.
Prescription pattern differed depending on the severity of pain and also depending on age. While prescribing analgesic drugs physicians had also considered other concomitant diseases, severity of the disease, tolerance of the patient to the treatment. Our study focused on different drugs used for the patient. The limitation of our study was that it was a single center study with limited sample size. As this was a retrospective, observational study in many circumstances it was difficult to analyze why particular drugs were used and why not others due to lack of details in the records. Based on the results and overall trend observed in drug prescription, conducting a prospective study will give more insight into the reason behind different drugs used as analgesic drugs.
CONCLUSION
The study showed that prescription pattern in palliative care unit of St. John's Hospital was in accordance with WHO three-step analgesic ladder pattern. In the future, widespread use of prescription databases and disease registries will serve as powerful tools to evaluate different therapeutic strategies for pain management and improve the quality of patient care.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- World Health Organization. What is drug utilization research and why is it needed. In: Introduction to Drug Utilization Research. Norway: World Health Organization; 2003. p. :8.
- [Google Scholar]
- Prevalence of pain in patients with HIV/AIDS: A cross-sectional survey in a South Indian State. Indian J Palliat Care. 2009;15:67-70.
- [Google Scholar]
- World Health Organization. WHO Normative Guidelines on Pain Management. Geneva: World Health Organization; 2007. p. :3-4.
- [Google Scholar]
- A review of opioid prescription in a teaching hospital in Colombia. J Pain Res. 2012;5:237-42.
- [Google Scholar]
- Opioid-prescribing Practices in Chronic Cancer Pain in a Tertiary Care Pain Clinic. Indian J Palliat Care. 2011;17:222-6.
- [Google Scholar]
- Analgesic effect of paracetamol on cancer related pain in concurrent strong opioid therapy. A prospective clinical study. Acta Oncol. 2008;47:891-5.
- [Google Scholar]
- Appropriateness of cancer pain management in Saudi teaching hospital. Gulf J Oncolog. 2009;5:37-43.
- [Google Scholar]






