Translate this page into:
Structural Challenges of Providing Palliative Care for Patients with Breast Cancer
Address for correspondence: Dr. Maryam Rassouli; E-mail: Rassouli.m@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
To establish a palliative care system (PCS) in Iran, it is necessary to identify the potential barriers.
Aim:
This study aims to highlight the views of stakeholders to know the challenges of providing palliative care for women with breast cancer.
Materials and Methods:
Semi-structured in-depth interviews are used with purposeful sampling conducted in Tehran, Iran; from January to June 2015. Twenty participants were included in the study: nine patients with breast cancer and ten health-care providers. The interviews were analyzed using qualitative directed content analysis based on Donabedian model. Data credibility was examined using the criteria of Lincoln and Guba.
Results:
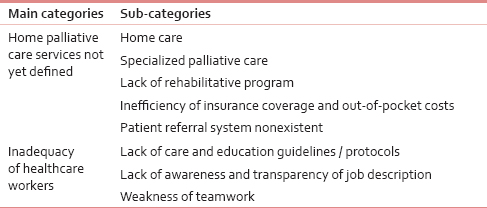
Based on the pattern of Avedis Donabedian model, two main categories were identified: (1) palliative care services in the health system still remain undefined and (2) lack of adequate care providers. The subcategories emerged from the main categories are: (1) Inexistent home care, (2) specialized palliative care being in high demand, lack of: (a) Rehabilitation program and guidelines, (b) treatment/training protocols, (c) inefficient insurance and out-of-pocket costs, (d) patient referral system, (e) nontransparency of job description, and (f) weakness of teamwork.
Discussion:
The findings of the study identify views and perceptions of patients as well as the health professionals around the challenges of providing palliative care. To establish a structured PCS, we need to meet the challenges and remove perceived barriers to, including but not limited to, building up knowledge and awareness of health professionals, educating professional, and developing updated, well-defined, and standard treatment protocols, tailored to local conditions.
Keywords
Breast cancer
Iran
Palliative care
Qualitative research
INTRODUCTION
The high incidence of breast cancer in Iran and reduced age of contracting this hard-to-cope-with and costly illness persuaded cancer specialists to apply the term “cancer tsunami” in a bid to highlight the severity of country's human and financial losses stemming from this disease.[1] In Iran, breast cancer is the most common cancer in women.[2] it does comparatively incur the highest direct costs of treatment so much so that the average total cost of pay out-of-pocket costs on breast cancer has been estimated at 2,053,000 Tomans ($ 684 USD) per month.[34]
Due to the high cost of health care and lack of skilled manpower to provide health care, it requires a heightened level of specialized services in palliative care, owing to the increased incidence as well as lower age distribution, as compared to other countries.[56] Today, provision of a comprehensive quality care is an undeniable necessity.[78] However, providing integrated client-based services, for some reason, including changes in the trajectory of diseases toward chronic diseases and aging population, still remains a major challenge for health-care system.[9]
Palliative care, as a basic human right, is essential for cancer patients.[810] Yet palliative care is defined as a care philosophy and a structure-based system to provide organized care that attempts to alleviate or extenuate suffering through early identification and management of pain and other physical, mental, and intellectual problems, which should be accessible based around patients’ needs.[11] Palliative care programs encompass a wide range of services including home care, day care, inpatient/outpatient units, hospital teams, and nursing home as required by patients with chronic diseases.[1213] These services are not limited only to specialized palliative care services, with level varying from one country to another. It is, however, estimated that over 20 million people are in need of palliative care in low- and middle-income countries across the world.[13] Taking into account the role of PC in cutting down on unwanted hospital admissions[14] and enhancing the quality of life,[15] as well as reducing the financial burden of cancer bearing heavily on the health system,[16] the health-care professionals are trying to provide the highest quality care using available resources.[17] In addition to providing clinical PC services, they considered a logjam around the health system in developing countries. In Iran, palliative care is a brand-new concept with no written plan of specialized services in accordance with the proportionate share of the overall demand.[18] Sporadically delivered, PC does not enjoy adequate support to the extent that patients usually do not receive essential care such as nursing as well as those associated with social, psychological, physical, and spiritual needs.[19] Although government's noncommittal approach to the philosophy of PC is said to be the greatest stumbling block to gaining access to and running the PC programs in the developing countries, and that the majority of problems to the implementation of PC services arise from absence of government strategies, consistent national policies, and broad negotiations with countries involved, it seems that structural hurdles to be the main concern of the health system structure of such countries, thereby considering the hindrance to establishing a palliative care system (PCS).[92021] Based on the researcher's systematic surveys, it seems that the existing knowledge in the field of palliative care is not well expounded, with limited studies delving into the stakeholders’ perceptions about palliative care as well as the obstacles and challenges to its being established.[22232425] Therefore, proper planning in relation to palliative care for cancer patients is a perceived need in the Iranian health system.[21] As models and theories can help researchers with identifying, describing, explaining, or predicting,[26] Donabedian model, as a conceptual framework, was used in this research.[27] In regards to the fact that identifying the matrix as well as the views of stakeholders are sine qua non and indispensable conditions of planning, the current study was conducted in response to the question “what is the stakeholders’ understanding and views about the existing structural challenges to providing palliative care in Iran?” It is the perceived barriers to supportive and palliative care and to help the development of this type of service.
MATERIALS AND METHODS
This qualitative study used semi-structured in-depth interviews with purposeful sampling conducted in Tehran, Iran, from January 2015 to June 2015. Under this model, the quality of care provided in the health system is defined in three measurable dimensions: Structures of care, processes of care, and outcomes. In this model, structure is meant to be the context or the environment in which patients receive services, such as equipment, facilities, personnel, healthcare policies, and cultural, social, and political characteristics of society.
Participants consisted of twenty health practitioners and women with breast cancer referring to the outpatient palliative care clinic in the Cancer Research Center of Shohadaye Tajrish Hospital (SBMU CRC) and Medical Oncology ward at Taleghani Hospital affiliated to Shahid Beheshti University of Medical Sciences as second referral center in the field of cancer in Iran.
Inclusion criteria for the admission of patients are: Definitive diagnosis of cancer made by a specialist, being aware of the diagnosis, lapse of at least 6 months from the time of diagnosis and treatment or completion of treatment cycle, and ability to speak in Farsi language. The criteria for admitting care providers included working in the area of care and treatment of cancer patients and having at least 1 year of hands-on experience in the field of cancer. Since in qualitative research there is no set criterion to determine the number of participants prior to the study, sampling continues as long as other participants do not add new information to the findings and thus, it goes uninterrupted till we reach data saturation.[26] In this study, data saturation was reached right after conducting twenty interviews. The researcher, before the start of the interview, explained to the participants the purpose of the study, confidentiality of information, and recording of interviews. They were asked to complete the consent form if they wished to participate in the study. Each participant agreed to have her views used while opting to remain anonymous.
The Ethics approval was obtained from the Shahid Beheshti University of Medical Sciences with code no.: SBMU2.REC.1394.51. The researcher, using pivotal questions, including: “During the treatment, what services were most needed by you/client?”… “What is your experience of receiving/offering care?”…. “For what reason you were unable to access the services you needed (patients)?”… “For what reason you could not offer services to your patients?” (healthcare providers). The interviewer, using follow-up questions, encouraged the patients to express their deeper experiences. Questions like “what do you mean by that?” “What did you feel then?”… “What happened next?”… “Could you possibly make yourself more clear by setting an example?” and so on. All the interviews were recorded by digital audio recording. The interviews were immediately transcribed after having been carefully listened several times, citing modes of expression such as laughter, sighs, tears, and silence were written. The interview process lasted for 30–90 min.
Data analysis
Directed content analysis (guided) was used for data analysis in which initial coding starts with a theory or similar research findings. This kind of analysis is useful in predicting variables of interest and/or the relationship between variables, as well as in determining initial codings and the relationships between codes.[28] The interviews were transcribed by the researcher in parallel. Texts were perused a couple of times to gain an in-depth and correct understanding, and then broken down into the smallest meaningful units.[29] The codes were grouped into two main categories using Donabedian model. The entire coding processes of all the interviews were managed using qualitative data analysis software MAXQDA 10 (VERBI software, GmbH, Berlin/Germany). To ensure validity and reliability of data in this study, Lincoln and Guba's four criteria including credibility, dependability, conformability, and transferability were used.[26]
RESULTS
In this study, twenty participants comprising nine women with breast cancer and 11 care providers were interviewed. Patients’ age ranged from 35 to 61, with the average age of 43 years. They were all married. An interval of 8–80 months has passed since the initial diagnosis. Of these, seven patients underwent total mastectomy, one breast-conserving, and one partial mastectomy surgery. Health-care providers included nine clinical nurse specialists (seven females and two males) and two physicians. The median years as a palliative care provider were 10 years (range 3–21(. In analyzing the interviews, 685 codes emerged once all duplicate codes were removed and similar cases merged, which were characterized in two main categories and eight subcategories [Table 1].
Palliative care services in the health system not defined
According to the health professionals, the PC services still remain ill-defined in the health sector|, including home-based care services, rehabilitation services, specialized palliative care services, insurance coverage and out-of-pocket costs, and lack of patient referral system.
Home care
According to the participants, ill-defined care at the end of disease and unawareness of families about the benefits of these services gave rise to unnecessary and recurrent hospitalization of patients, thus unnecessarily occupying hospital beds and incurring financial burden:
“The family insists on hospitalizing the patients with cancer who are at the final stage, and have already received extensive metastasis. If home care services are launched, hoteling costs and unnecessary occupation of the beds will be dramatically decreased” (physician).
“Many patients are hospitalized in ICU before the end of their life because we do not provide any kind of palliative care services at home, especially in the presence of families” (physician).
Specialized palliative care
The participants stated that patients with advanced cancer are often hospitalized in general wards. More coherent healthcare will be provided once palliative care services are known and determined:
“Currently we visit caseloads of patients casually as acting consultants in the hospital wards, and if otherwise the patient requires more advanced measures, we will not be able to provide special palliative care” (physician).
Lack of rehabilitative services
Participants, while emphasizing the need to provide palliative care soon after diagnosis of cancer, said that due to the structural problems, the grounds for providing rehabilitative services were not laid right from the beginning.
“The situation goes like this that the patient on her initial visit followed by diagnosis goes through treatment stages, and returns home after surgery; afterward, in case she observes any symptom of the disease again, she will have to repeat the same cycle of treatment…. Unfortunately, there is no post-treatment comprehensive and systematic program for a back-to-normal life pattern to return to normal life, and most patients are released like that… Rehabilitation is a very important part of cancer treatment” (physician).
Insurance inefficiency and out-of-pocket payments
Skyrocketing costs are incurred on families, owing to the chronic causes of cancer, which are out of their means. Most of the patients believed that health-care insurance does not meet their needs. One of the patients, a 55-year-old patient, being in the follow-up phase, said:
“My doctor told me that I had to buy foreign-made medicine if I wished to quickly get better. Foreign-made drugs are too expensive and not covered by insurance policy, and we cannot afford to pay 200 $ monthly off a retirement pension” (patient)
Another patient is quoted as saying:
“I cannot use the benefits of my supplementary insurance as some medicines are not duly covered and I have no choice but to use medicines available in the public hospitals” (patient).
In line with the patients’ comments, the health-care providers also reiterated the inadequacy of insurance service coverage:
“With regard to the long waiting queues that the cancer patients face in an attempt to secure an empty bed for outpatient or hospitalization services…. one more problem is that insurance companies do not cover palliative services, or the high costs of treatment that villagers have to bear” (Nurse).
A GP with 5 years of experience in cancer care, said:
“It is not specified whatsoever in the health system that what type of service we provide exactly… even no funding source or budget row is defined for palliative care services” (physician).
Lack of patient referral system
The health providers mentioned that there is no specified directory meant for referral when dealing with patients with breast cancer, which per se leads to the patients’ ending up in confusion and fatigue in the course of treatment process.
“Once a diagnosis of cancer is confirmed, we should begin treatment. We do encounter a whole lot of problems though. In addition to being under the stress of cancer diagnosis, patients are involved with financial and many other problems as well… first we need to know where to make the referral to…” (Physician).
Participants expressed that the establishment of a referral system based on stratification of health services is one of the essential objectives in the treatment of patients with breast cancer:
“Taking appropriate action for early diagnosis based on the guidelines available, referral and follow-up requirements is almost absent… and that the health system should provide all the three types of prevention, treatment, and rehabilitation” (physician).
Inadequacy of health-care providers
Participants in the study believed, that the care providers’ lack of adequate knowledge and awareness of PC, nonexistence of clinical guidelines and protocols in primary care and education, fuzzy and vague job descriptions, and weak teamwork skills are among those structural barriers to providing effective palliative care.
The health sector responsible to provide quality care requires skilled, knowledgeable, and experienced staff in the field of palliative care. This sphere of activity, however, is suffering due to the shortage of experts and insufficient knowledge and know-how on the part of the providers. One of the doctors said:
“There is a critical shortage of palliative care specialists and only oncologists bear the brunt of treating patients” (physician).
Of other structural problems plugging up the flow of providing favorable PC, as participants enumerated, are: Pioneer and trainers not designated, unclear job description for palliative care team, and inadequacy of in-service training in the field of PC:
“The main problem we face is lack of access to education and that there is no designated tutelage. Instructional materials are perhaps available casually either online or in print, but we must sum it all up and get to know who is going to present this (instructional materials)” (Physicians).
On the need to educate nurses specializing in this area, one of the participants says:
“During the four-year degree program in nursing, I did not receive professional training in the area of providing care to patients who are in the final and bereavement stages, or facing complex problems. I believe it is highly essential to have a cancer nursing track introduced in the graduate program” (Nurse).
In addition, participants expressed their dissatisfaction with the inadequacy of the in-service training programs in relation to palliative care:
“To provide better care for patients, we need training on how to manage complications because patients with chronic diseases have complex needs and it is of great importance to manage the situation” (Nurse).
Health-care education guidelines/protocols are nonexistent
To the participants, education is the integral part of healthcare, and one of the challenges in providing palliative care is the lack of standard and formal educational curriculum:
“There should be a system to educate people from the beginning on how to behave in society. The main problem is lack of education. Instructional materials are available on the internet and in books sporadically, but we have to have a good rundown of these sources, and make it clear whose duty is to present it (material), not just a pile of manuals and brochures to be used at times when the patient feels like interested to read” (physician).
In other words, lack of formally written protocols for educating patients is one of the other challenges in the area of cancer care provision:
“Developing standard curriculum specific to patient education ranks one of the main concerns in the field of the cancer, and the treatment team often face challenges in this area. For instance, the patient sometimes asks questions about the type of diet whereas the doctor or dietitian may not be aligned with nursing education” (Nurse).
Lesser-quality teamwork
The participants hold that teamwork is an essential element in the effectiveness of cancer treatment, yet being neglected in the medical community. Participants believe that the care of patients suffering from advanced cancer should be provided by an expert team fully conversant with clinical situations such that the initial base of PC provision is the existence of teamwork culture within health-care providers.
One of the participants touched on the need for a multiteam system for patient care, but, however, absence of teamwork culture is evident across the health system:
“A patient has already undergone surgery, and the idea of surgeon/physiotherapist working in tandem, thus far, has not gone down very well… A surgical patient, bedridden, yet not able to easily move her hand up, muscles weakened caused by decreased mobility or post-surgery pain and some swelling in the area of surgical site and shoulders…” (physician).
DISCUSSION
The findings of this study, aimed to explain the perception of stakeholders around the structural challenges to palliative care provision for women with breast cancer, showed that structural challenges are classified into two categories: Not-yet-elaborated palliative care services and inadequacy of healthcare providers.
Lack of specialized palliative services, referral system, and inefficient insurance services are cited as structural impediments to providing palliative care by the participants so much so that even with a change of policy of providing specialized palliative care toward primary care provided by general practitioners and community health nurses,[930] and awareness of the benefits of palliative care of the interdisciplinary counseling teams, the cancer patients in Iran still receive their needed care in hospitals while centers that provide home care are few and far between, and there is no such thing as hospices.[23] One of the important aspects of care provided to patients with cancer is the availability and possibility of utilizing medical resources and financial support by both the government and insurance organization to the extent that issues such as patients’ insurance coverage (amount of out of pocket payments),[23] and failure to provide health services based on leveling, and consequently increases in health care costs, seem to be the ostensible barriers to palliative care provision in this area.[18]
Service tariffs seem to be among the main challenges to palliative care services provision, which practically renders impossible manpower recruitment (doctors, nurses, and all service providers). Obviously, without service tariffs, home-care services will be out of question.[313233] One of the measures taken to address this problem is the “Health Reform Plan.”[23] and now after 1 year into the implementation of the plan, 95% of the population is covered by supplementary health insurance and people's out-of-pocket payment in the area of health scaled down from 55% in 2009 to 10% in 2014.[34] Therefore, cooperation between organizations and insurance organizations on a large scale is regarded one of the constructive approaches toward promoting care based on the clients’ individual needs and life quality revolving around the development of cooperation across individuals, groups, and organizations.[1035]
Despite the need for specialized training and basic knowledge and skills in providing PC for all health professionals,[36] participants in our study were cited as holding that lack of knowledge/awareness of the palliative care treatment team and the weakness of teamwork are the core causes of the care providers’ inefficiency. Tahmasebi stated that more than half of the Iranian physicians possess scant knowledge in the area of palliative care and its philosophy, symptoms management, and how to go about the palliative care,[37] with more than half of them agreeing to their having little knowledge in pain control management and end-of-life and palliative care principles.[38]
Different studies acknowledge that the main problem with the health system in Iran, in the area of palliative car, is lack of definition of palliative care in the health system, lack of PC job title for nurses,[24] limited number of palliative medical specialists,[5] inefficiency of nurses in providing palliative care,[25] and shortage of in-service training programs to empower professional staff.[39] Furthermore, consistent with the rest of the world (except for a few European countries) incorporating a palliative care module to be integrated into medical curriculum was not compulsory,[36] and there is no such thing as syllabus content as far as PC is concerned.[15243840]
Among other factors affecting the quality of care is team collaboration.[4142] The results emerging from numerous studies showed that teamwork failure, interprofessional conflicts and the concomitant tensions,[43] lack of coordination between services, heterogeneous palliative care coverage,[44] unclear job descriptions,[45] lack of awareness, and transparency of duties between health workers[46] can contribute to challenges in palliative care provision.
Palliative care, being a dynamic discipline and considered a specialty in medical science, requires collaborative teamwork reinforced by its being multidisciplinary by nature[47] thus, important step can be taken toward resolving the structural problems within the PCS via promoting a culture of teamwork among other health team members through formal education, heightening professional awareness around palliative care and concerted measures of the PC support groups, health administrators, and policy makers.[4849] In short, under the health policy instrument for promoting primary care, enacted by the health policy and reform secretariat in 2007, the flaws in the healthcare structure of Iran include lack of insurance coverage, centralized structure, failure to establish the position of nongovernmental sector, inefficacy of the existing structure against new needs such as cancer, physical resources taking precedence over human resources, lack of balance in the staffing, financing, payment system, and the lack of rules.[18]
It is noteworthy that the current study is qualitative and has been conducted on a small number of participants, thus being of narrow generalizability.
Today one of the challenges of the health system is the provision of palliative care services to chronically-ill patients. Participants believed the PCS in Iran is at the mercy of structural impediments such as improper definition of palliative care services, including home care, palliative care and specialized rehabilitation programs, inadequate training and lack of awareness and expertise of palliative care staff, lack of educational guidelines and protocols on healthcare, lack of transparency of duties, poor teamwork, and inefficacy of Insurance. In Iran, Palliative care is a new discipline and its objectives are not yet fully achieved. It is hoped that in near future, the system will be all-set by improving staffs’ professional awareness in the health system and removing the existing structural barriers. Although the aim of this study was to evaluate the structure, there was no significant distinction between structure, process, and outcomes. In addition, the components which are included in the current study as structure coincide with proposed structural components in the study of Farjah and Detterbeck 2015.[50] With respect to the gravity of services tariffing, authorities in the health system may endeavor to determine relative value of services and health services tariffing, taking into account the existing structural barriers to establishing PC system.
Financial support and sponsorship
This study is part of a doctoral nursing dissertation of Shahid Beheshti University of Medical Sciences. The full title of dissertation is: “Design a service package palliative care for women with breast cancer.” The study sponsors had no role in the study design, data collection and analysis, data interpretation, report writing, and submitting or publishing the article.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Executive Guideline for Registering and Reporting Cancer Cases. Tehran: Cancer Office and the Research Fellowship of Cancer Research Center of Cancer Institute; 2007. p. :122.
- Trends in epidemiology, clinical and histopathological characteristics of breast cancer in Iran: Results of a 17 year study. Asian Pac J Cancer Prev. 2013;14:6905-11.
- [Google Scholar]
- Cost analysis for cancer subgroups in Kerman, IRAN. Iran J Epidemiol. 2012;8:62-70.
- [Google Scholar]
- Examination of medical and non-medical direct costs of outpatients and hospitalized cancer patients in Shiraz, Iran. Payesh. 2015;6:629-37.
- [Google Scholar]
- Palliative care in the Islamic republic of Iran. In: Silbermann M, ed. Palliative Care to the Cancer Patient: The Middle East as a Model for Emerging Countries. New York: Nova Scientific Publisher; 2014.
- [Google Scholar]
- The direct medical costs of breast cancer in Iran: Analyzing the patient's level data from a cancer specific Hospital in Isfahan. Int J Prev Med. 2013;4:748-54.
- [Google Scholar]
- Educating for healthcare quality improvement in an interprofessional learning environment: A New Zealand initiative. J Interprof Care. 2006;20:555-7.
- [Google Scholar]
- Developing targets for public health initiatives to improve palliative care. BMC Public Health. 2010;10:222.
- [Google Scholar]
- Clinical priorities, barriers and solutions in end-of-life cancer care research across Europe. Report from a workshop. Eur J Cancer. 2010;46:1815-22.
- [Google Scholar]
- Int [Homepage on Internet] WHO Definition of Palliative Care. Available from: http://www.who.int/cancer/palliative/definition/en/
- [Google Scholar]
- Trajectories of symptom occurrence and severity from before through five months after lung cancer surgery. J Pain Symptom Manage. 2015;49:995-1015.
- [Google Scholar]
- Mapping levels of palliative care development: A global update. J Pain Symptom Manage. 2013;45:1094-106.
- [Google Scholar]
- Integrating palliative care into comprehensive cancer care. J Natl Compr Canc Netw. 2012;10:1192-8.
- [Google Scholar]
- Early specialty palliative care – Translating data in oncology into practice. N Engl J Med. 2013;369:2347-51.
- [Google Scholar]
- Cost savings associated with US Hospital palliative care consultation programs. Arch Intern Med. 2008;168:1783-90.
- [Google Scholar]
- Selfevaluation of hospitals and medical education centers performance under Isfahan University of medical sciences using EFQM in 2007. Med Res. 2008;3:227-31.
- [Google Scholar]
- Cancer care in countries in transition: The Islamic republic of Iran. In: Silbermann M, ed. Palliative Care in Countries & Societies in Transition. 2016. p. :317-36.
- [Google Scholar]
- Palliative care in Iran: Moving toward the development of palliative care for cancer. Am J Hosp Palliat Care. 2016;33:240-4.
- [Google Scholar]
- Structuring a palliative care service in Brazil: Experience report. Braz J Anesthesiol. 2014;64:286-91.
- [Google Scholar]
- Mapping levels of palliative care development: A global view. J Pain Symptom Manage. 2008;35:469-85.
- [Google Scholar]
- Nurses’ attitudes toward palliative care in south-east Iran. Int J Palliat Nurs. 2013;19:403-10.
- [Google Scholar]
- Human relationships in palliative care of cancer patient: Lived experiences of Iranian nurses. Mater Sociomed. 2014;26:35-8.
- [Google Scholar]
- Perception of Iranian nurses regarding ethics-based palliative care in cancer patients. J Med Ethics Hist Med. 2013;5:141-64.
- [Google Scholar]
- Nurses’ knowledge about palliative care in Southeast Iran. Palliat Support Care. 2014;12:203-10.
- [Google Scholar]
- Qualitative Research in Nursing: Advancing the Humanistic Imperative (5th ed). Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
- Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277-88.
- [Google Scholar]
- Scoping Exercise on Generalist Services for adults at the End of Life: Research, Knowledge, Policy and Future Research Needs. Recommendations for Future Research in Generalist End of Life Care. In: Report to the NHS Service Delivery and Organisation Research and Development Programme. King's College. London: University of London; 2007.
- [Google Scholar]
- Unresolved issues in medical tariffs: Challenges and respective solutions to improve tariff system in Iranian health sectors. Hospital. 2012;10:21-30. [Persian]
- [Google Scholar]
- Economic evaluation of varicella vaccination in Swiss children and adolescents. Hum Vaccin. 2009;5:847-57.
- [Google Scholar]
- Determinants of resource utilization in four palliative care units. Palliat Med. 2006;20:95-106.
- [Google Scholar]
- Patient satisfaction before and after executing health sector evolution plan. Iran J Emerg Med. 2015;2:127-33.
- [Google Scholar]
- Cancer surveillance and control in adolescents – Similarities and contrasts between Canada and the United States. Pediatr Blood Cancer. 2006;46:273-7.
- [Google Scholar]
- Palliative care in geriatrics – Conceptual design and methods of a study to explore the viewpoints of different health care professionals and disciplines. Z Gerontol Geriatr. 2009;42:127-30.
- [Google Scholar]
- Palliative care for the end-of-life cancer patients in the emergency department in Iran. Iran J Cancer Prev. 2013;6:231-2.
- [Google Scholar]
- Switching methadone: A 10-year experience of 345 patients in an acute palliative care unit. Pain Med. 2012;13:399-404.
- [Google Scholar]
- Do multidisciplinary team meetings make a difference in the management of lung cancer? Cancer. 2011;117:5112-20.
- [Google Scholar]
- Interventional oncology in multidisciplinary cancer treatment in the 21 st century. Nat Rev Clin Oncol. 2015;12:105-13.
- [Google Scholar]
- Palliative care for older people – Exploring the views of doctors and nurses from different fields in Germany. BMC Palliat Care. 2009;8:7.
- [Google Scholar]
- Interpretation of palliative care concept, its barriers and facilitators using meta-synthesis. Mod Care J. 2014;11:316-29.
- [Google Scholar]
- Iran's multiple indicator demographic and health survey-2010: Study protocol. Int J Prev Med. 2014;5:632-42.
- [Google Scholar]
- Palliative care in Germany from a public health perspective: Qualitative expert interviews. BMC Res Notes. 2009;2:116.
- [Google Scholar]
- Current status of palliative care – Clinical implementation, education, and research. CA Cancer J Clin. 2009;59:327-35.
- [Google Scholar]
- Facilitating good process in primary palliative care: Does the gold standards framework enable quality performance? Fam Pract. 2007;24:486-94.
- [Google Scholar]
- Early specialty palliative care – Translating data in oncology into practice. N Englnd J Med. 2013;369:2347-2351.
- [Google Scholar]
- What is quality, and can we define it in lung cancer? The case for quality improvement. Transl Lung Cancer Res. 2015;4:365-72.
- [Google Scholar]






