Translate this page into:
Symptoms In Bangladeshi Patients with Incurable Cancers: Implications for Interventions
Address for correspondence: Dr. Richard R Love, 2708 Columbia Road, Madison, WI 53705 USA. E-mail: richardibcrf@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims:
The poor state of palliative care in low- and middle-income countries has been termed a global crisis by the Lancet Commission on Palliative Care. The investigators previously reported on a cross-sectional study of symptoms in 640 Bangladeshi adults with incurable cancers. Usual levels of pain were high. The not-reported details of pain and other symptoms offered an opportunity to consider explanations and implications for interventions to lessen these symptoms.
Methods:
At one visit, 640 Bangladeshi patients completed a symptom questionnaire. The distributions of 12 symptom level scores and the correlations between pain and different symptom scores were determined.
Results:
The population had significantly high and functionally compromising average usual pain scores, but low percentages of patients with very high and low pain scores. The distributions of scores for multiple symptoms were all skewed to higher mid-scale levels and modestly high (≥0.6) correlations of pain with nausea, anxiety, lack of appetite, constipation, and sleep quality were seen.
Conclusions:
While the types and direct effects of the cancers, the young age distribution, and the true symptomatic status of this Bangladeshi population studied may explain the described characteristics, the observations deserve exploration of other causes with specific therapeutic implications. These patients appear to have been partially treated for pain, and in particular, environmental factors such as extreme heat and its consequences appear more likely causes of moderate levels of multiple symptoms, which collectively magnified patients' suffering. Greater attention to gastrointestinal symptoms and sleep disturbance, in particular, seems indicated.
Keywords
Nondisease causes of symptoms
palliation
symptoms
INTRODUCTION
The poor state of palliative care in low- and middle-income countries has been termed a global crisis by the Lancet Commission on Palliative Care.[1] Bangladesh has been ranked 79th out of 80 countries on the recent Economist Quality of Death Index.[2] In practice in Bangladesh currently, there are very, very few palliative care health professionals (physicians, nurses, other caregivers, or volunteers) or hospices, and no population-wide significant palliative care efforts at all. Affordability of care, training, access to opioids, and psychological support (at a basic level addressing abandonment) were identified critical issues in the Economist analysis.[2] Additional barriers to successful management include (i) the desires of seriously ill patients to be at home, and not to travel to doctors' offices or clinics; (ii) absence of “real” time (that is, current) symptom type and intensity information by doctors because symptom questionnaires are not much used at all or repeatedly used; (iii) absence of information on practical, affordable, and effective interventions among treating physicians; and efficient systems and processes to facilitate physicians' giving successful palliative care and to lead to greater engagement of physicians overall in this kind of care.[2]
While these considerations are all valid, successful management has to begin with some understanding and the implications of the numbers, levels, and types of symptoms which patients with limited life expectancy have. In the current authors' reported work, among 640 patients with incurable cancers regularly seen in tertiary care outpatient clinics in Bangladesh (and thus one of the optimal circumstances of patients needing palliative care in the country), on 10-point Likert scales, two-thirds reported usual pain scores of ≥5 (or moderate).[3] Our initial report focused on this finding and the obtaining of this information using a 15-item cell phone questionnaire.[3] The detailed information on all of 12 symptoms and their implications for management are the subject of the current communication.
METHODS
The details of the acquisition of the data reported here have been published.[3] Briefly, after approval by the Scientific and Ethical Review Boards in Bangladesh and the United States, we approached 642 patients with incurable malignancies presenting for care in oncology clinics at two tertiary care institutions in Dhaka, Bangladesh. Six hundred and forty patients provided written informed consent and agreed to provide information about their symptoms using a validated cell phone questionnaire. The 15-item questionnaire covered nausea, tiredness, depression, anxiety, drowsiness, appetite, well-being, shortness of breath, and current worst, least, and usual levels of pain in last 24 h, constipation, quantity of sleep, and quality of sleep. Patients answered the questions by moving a cursor along visual analog scale bars (0–10) to indicate intensities of each of these symptoms. The data were collected over an 18-month period that included two summers.
RESULTS
Sixty-one percent of patients (392/640) were aged 50 or younger. Only 3% reported having no usual pain, while no patients reported having usual severe pain levels (8 or greater). About 90% had mild to moderate usual pain scores (3–6). Only three patients ever had pain levels of 7 or greater. Sixty-one percent had minimal pain scores of 4 or 5 or moderate.
Majorities of patient had moderate (scores of 4–7) levels of the following symptoms: Tiredness, nausea [Figure 1], depression, anxiety, drowsiness [Figure 2], poor appetite, constipation [Figure 3], sleep quality, and sleep quantity. The specific provided figures are representative of those found for the other symptoms listed.
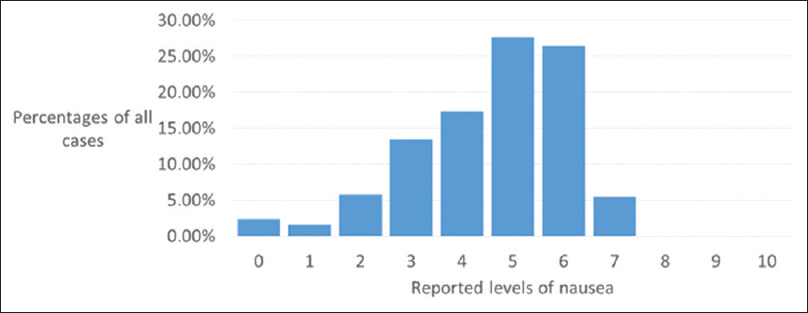
- Distribution of nausea levels among 640 Bangladeshi adults with incurable cancers
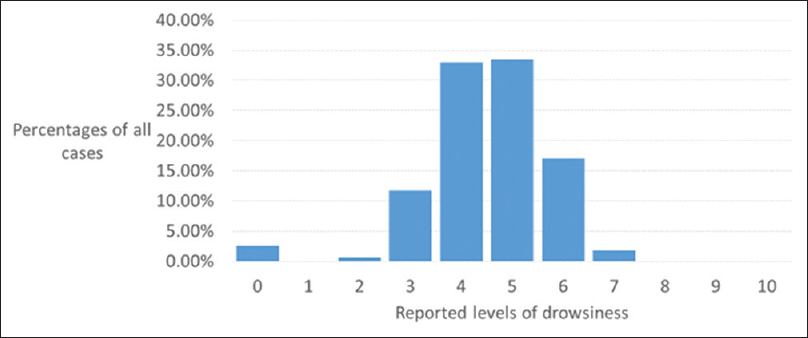
- Distribution of drowsiness levels among 640 Bangladeshi adults with incurable cancers
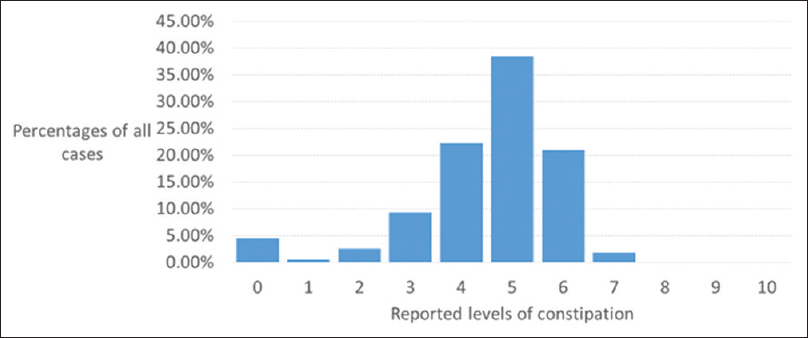
- Distribution of constipation levels among 640 Bangladeshi adults with incurable cancers
Moderately high correlations of pain levels with nausea (0.75), anxiety (0.76), poor appetite (0.75), sleep quality (0.74), and constipation (0.59) were seen.
DISCUSSION
As suggested in the introduction, our sample of patients is likely to be significantly less symptomatic than the majorities of patients who could not present to often distant oncology facilities because of the severities of their conditions, or who were less able seek such care because of socioeconomic deprivations. We should first ask whether there are cultural or language or educational factors which might explain or affect the responses these relatively more fortunate patients have given to these symptom questions. Our impressions are that patients understood the symptom terms and scaling issues and were not providing socially “correct,” or answers with understanding other than the commonly understood meanings. In Bangla, the terms “nausea”, “poor appetite”, and “anxiety”, for example, seem to connote the same meanings as these terms do in usual English parlance. The impressions of Bangladeshi clinicians are that unwellness is common among their countrymen, and the great extent of reported symptoms among patients with incurable cancers was not surprising to them. In sum, the authors believe that the data presented are truly representative of what the studied patients have.
In considering the data about pain, we might ask whether the younger age distribution of cases (than likely occurs in the population as a whole), and the types and direct effects of the cancers might best explain the generally high levels of pain. The distribution of cancer types was broad; no immediate explanations develop to support or refute age or type explanations.[3] The general conclusion would seem to be that this population was being partially treated (reflected by the absence of patients with high pain scores), but undertreated, as evidenced by the high fraction of patients with moderate pain scores, and high fraction with minimal pain scores that were moderate. This conclusion begs a solution which gives physicians more real-time patient pain data because it suggests that pain was being treated – treating physicians were aware – but not completely, perhaps in “real time,” informed.
The moderate reported levels of multiple symptoms are perhaps more provocative. Accepting them at face value as genuine requires then acknowledging that these likely contribute significantly to the extent of suffering and augment pain perceptions. Climate, particularly high heat levels, and air pollution levels, would appear to be significantly important to these Bangladeshi urban residents. Interventions addressing these symptoms might be expected to usefully improve functional status: the evidence is that lowering symptom scores like those for pain, by 1–2 units on such 10-point scales does achieve such goals.[4] In the studied populations, lowering symptom scores from moderate (4–6) ranges to <4 would thus be expected to have significant clinical benefits. For examples, environmental interventions-staying out of the heat-, and interventions directed at sleep and at gastrointestinal symptoms--optimal hydration, increased physical activity, and laxatives-, might be expected to have disproportionately great clinical benefit.
How then could we bring these observations more practically to bear on clinicians' work and facilitate more impactful palliative care? Specifically, how might we address the barriers noted in the introduction above? Based on the investigators' experience with the questionnaire, we have developed the Amader Gram Palliative Care System, first with a software tool for organizing successive reports with this questionnaire for physician review (ag-palliativecare. net). The reports can present longitudinal data by item and the system can automatically notify the specific physician identified by the patient, through E-mail or text messaging (widely used in Bangladesh), of new reports and of major changes in, or persistent high levels of symptom scores. Further, the investigators have created a website for the reports which also has succinct clinical practice guidelines for palliative care, and prescription writing capacity for immediate physician access and use (ag-palliativecare. net). Finally, this Amader Gram Palliative Care System doctors' team has developed an operational system use requirement that a served patient and/or a family member has/have to visit his/her physician at least once every 2 weeks to ensure regular care, and proper record-keeping. In summary, this system addresses palliative care patients' desire to stay at home, provision of real-time patient symptom data to physicians, and fingertip available practical interventions with an efficient, physician user-friendly system which is accessible to all.
CONCLUSIONS
In a Bangladeshi population with incurable malignancies likely to be less symptomatic and receiving care in tertiary care institutions, pain was found to be significantly undertreated. Moderate scores for multiple symptoms were also seen. Attention to these issues is likely to significantly improve patients' reported symptomatic status.
Financial support and sponsorship
This project was financially supported by The International Breast Cancer Research Foundation.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Lancet. Available from: http://www.thelancet.com/commissions/palliative-care
- Economist Intelligence Unit. In: The 2015 Quality of Death Index. London, United Kingdom: The Economist; 2015.
- [Google Scholar]
- Symptom levels in care-seeking Bangladeshi and Nepalese adults with advanced cancer. J Glob Oncol. 2017;3:257-60.
- [Google Scholar]
- When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain. 1995;61:277-84.
- [Google Scholar]






