Translate this page into:
The Prevalence of Chronic Pain among Adults in India
Address for correspondence: Dr. Parmanand N Jain, Department of Anaesthesiology, Critical Care and Pain, 2nd Floor, Main Building, Tata Memorial Hospital, Parel, Mumbai, Maharashtra, India. E-mail: pnj5@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The prevalence of chronic pain (CP) is well described in Europe, America, and Australia. However, little knowledge is available of the prevalence of CP within Asia or Southeast Asia. Given the cultural and genetic variation in pain causation, manifestation, and reporting, the findings of previous western studies cannot be extrapolated to Asian countries. A prevalence study was needed to be carried out to quantify the magnitude and impact of CP in the adult population in India.
Methods:
Two sets of questionnaires were designed. The first, a screening questionnaire was used telephonically to identify the prevalence of CP, and should there be CP; the second, a detailed questionnaire was administered, to characterize the features and impact of pain. The interviews were carried out face-to-face.
Results:
A total of 4326 Indian patients were screened, and 836 completed a detailed pain questionnaire during 2006. The prevalence of CP was found to be 19.3% (n = 836). There was a higher prevalence in females (25.2%). Pain prevalence increased steeply beyond the age of 65 years old. There was a significant impact of CP on work and daily function.
Conclusion:
This Indian adults' population survey about CP found a higher prevalence of CP as compared to other Asian pain prevalence studies; however, the impact of pain was just as significant. In a rapidly aging population, CP is emerging as a significant healthcare problem which may likely to exert an increasing toll on the existing social infrastructure within the next two decades.
Keywords
Chronic pain
India
prevalence
questionnaires
surveys
INTRODUCTION
Chronic pain (CP) is a major healthcare problem. Although acute pain may reasonably be considered a symptom of a disease or trauma which may successfully be treated. However, CP may be considered a disease in its own right as described by European Federation of International Association for the Study of Pain (IASP) Chapters Declaration on Pain.[1] Pain is just not a symptom of a disease but a disease state in itself. The IASP provides a widely used definition of CP that takes into account duration, severity, and “appropriateness”. IASP defines CP as pain without apparent biological value that has persisted beyond the normal tissue healing time (usually taken to be 3 months).
CP is one of the most disabling problems with significant health, social, and economic repercussions. Efforts to determine the prevalence of CP in the general population are faced with various challenges such as variations according to the population sampled (general population vs. primary care), the methods used to collect the data, demographics (age, sex, income, and urban-rural divide,) and the criteria used to define “CP.” Pain perceptions and behavior are heavily influenced by culture and by the sociocultural context of people.
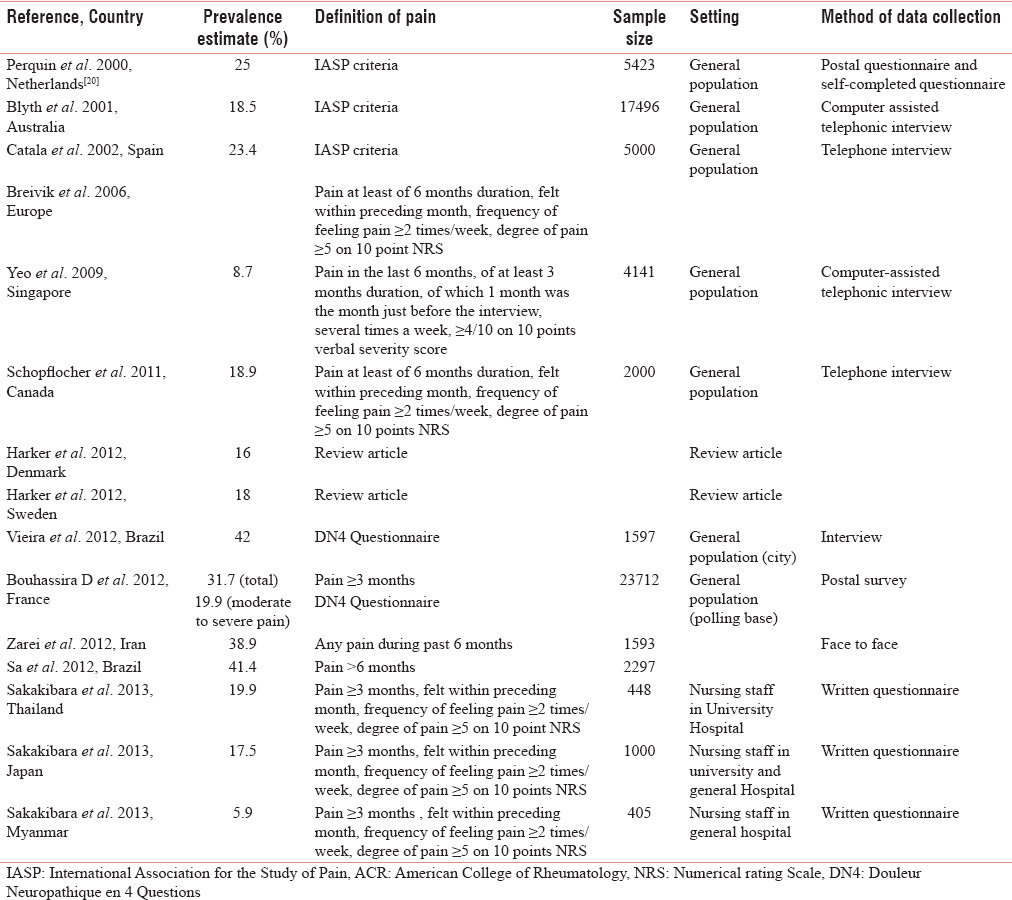
Approximately 30% of the world's population suffers from pain. Various regional pain surveys' reliable estimates indicate that the CP prevalence is somewhat closer to 30%–40%.[234567] A big CP prevalence survey “Pain in Europe” reported it as 12%–30% in the European countries.[7] However, in a four countries Asian pain survey, Singapore reported a lower prevalence of CP as 8.7%.[8] In Japan, Thailand and Myanmar CP prevalence has been reported to be 17.5, 19.9%, and 5.9% respectively.[9] This pain survey is the first-ever extensively conducted CP prevalence study in Indian population. We report the detailed findings of the prevalence, its impact on health, types of treatment used and its social impact on the adult population.
METHODS
This cross-sectional study for evaluating the prevalence of CP in Indian population was carried out between April and July 2006. Two sets of questionnaire were used. All subjects of either gender aged between 18 and 80 years of all socioeconomic classes were included for listing (i.e., screening) listing questionnaire (LQ). The subjects who were suffering from CP for a duration of more than 3 months, presence of pain in last month, and pain several times a week were then subjected to detailed questionnaire (DQ). The DQ interviews were carried out face-to-face. DQ was designed to uncover areas such as characteristics of pain, the impact of pain, attitudes to pain, beliefs, and cultural practices prevalent in the society. Questions were included about how the CP affected their quality of life. Details of treatment taken for pain by patients were also enquired; types of analgesics, over-the-counter (OTC) or prescribed by a doctor, type of doctor, and also the details of nonpharmacological treatment received by patients.
Sample selection
Urban-to compensate for heterogeneity arising due to difference percentage of people residing in different types of towns, the urban population stratum was split across a total of 5 classes as:
Class population
-
Mega metros 40,00,000+
-
Metros 1,000,000–3,999,999
-
Large towns 500,000–999,999
-
Small towns 100,000–499,999
-
Class I and below towns <100,000
-
Towns with a population >20,000 were included in this study. The houses surveyed were based on cluster sampling. The adult of the household selected was then asked the questions of LQ. If any of the households had CP, the sufferer was interviewed on a DQ. To avoid interviewer bias and ensure randomness, KISH grid was used if more than one person was eligible for DQ interview in a single household.
Rural
Sampling in rural India was done using sociocultural regions (SCRs). To cover all the states, total sample was allocated to SCRs. One district was taken as representative of that SCR. Within this district, 10 villages were then selected using Probability Proportional to Size method. To select households within a village, the interviewer drew a map of the village in consultation with an opinion leader. The map indicated clusters of households and 10 such homogenous clusters were selected systematically. In each cluster, 7–8 listings were carried out with a gap of five households between every two contacted ones, to yield 75 interviews. Subsequently, interviews were carried in same way as in urban clusters, through the face to face interview method.
Measures
The LQ included questions on demographic parameters such as age, gender, urban/rural as well as questions to detect the prevalence of CP. IASP definition of CP was considered as benchmark for identifying a CP sufferer.
CP-sufferer should have:
-
Suffered from more than 3 months
-
Suffered pain during last month
-
Suffered pain several times a week
-
Intensity of pain more than 4/10.
The second set of questionnaire, DQ, was designed for respondents with moderate-to-severe CP. It included questions related to pain characteristics, the impact of pain on quality of life, doctor visits, and treatment obtained by the sufferers.
To test the robustness of the definition of CP and to test the accuracy, relevance, comprehensibility, and user-friendliness of LQ and DQ, a pilot study was carried out in December 2005. In addition, validation interviews were carried out with specialist pain physician to ensure the quality of field work and steps were undertaken in line with TNS quality control systems.
Statistical methods
The data were analyzed using SPSS (IBM SPSS Statistics for Windows, Version 15.0. Armonk, NY: IBM Corp). Two sets of data were generated from the survey; the LQ data and DQ data. Standard error (SE) was derived based on simple random sampling at the 95% level of confidence.
Where P = Percentage estimate from the survey
n = Sample size.
RESULTS
A total of 6549 households were contacted telephonically, of which 4326 (66%) screened individuals completed the LQ. Of these, a total of 2176 (50.3%) respondents had rural background, and 2150 (49.7%) respondents were from the urban area. Eight hundred and thirty-six (19.3%) respondents (415 rural and 421 urban) were found to have chronic persistent pain and were subjected to DQ. Thus, an overall prevalence rate of 19.3% was found for CP in the Indian population.
Gender
Nearly 70.6% of respondents suffering from CP were females. The prevalence rate in females was 25.2% (n = 591/2345), significantly higher compared to the rate of 12.3% (n = 245/1981) in males [Figure 1 and Table 1].

- Gender Distribution of chronic pain patients with different grades of severity

Age
Those above 60 years of age appeared to experience more CP as compared to <60 years of age [Table 1]. The mean (standard deviation) age of the respondents was 45.7 (19.8) years. The average duration of pain was 4.2 years (males-5.06; females-3.59) [Table 2].

Site of pain
The most prevalent location of pain was knee (23.6%), followed by lower back and head. Joint and muscle pains were the most common causes of pain [Figure 2].

- Prevalence of chronic pain according to anatomical sites
Impact of pain on life
Thirty-six percent of respondents were not able to do their routine work due to pain. 25.5% had accepted pain as part of their lives. 14.1% of respondents had anxiety and depression due to CP [Figure 3].

- Morbidities associated with chronic pain
Type of pain consultation
Nearly 71.2% of CP sufferers were currently visiting a doctor (allopathic/alternative medicine doctors) for their pain. Only 4.8% patients of the total respondents were visiting a specialist pain physician [Table 3].

Choice of treatment
Overall, 72% patients used analgesics. Fifteen percent patients did not use any medications. Sixteen percent of respondents were not aware of any analgesics. Thirty-five percent and thirty-seven percent patients were using either OTC drugs or prescription drugs, respectively. Ayurvedic and homeopathic medications were used by 16 and 22% of respondents, respectively. In addition, 35% of patients opted for massages and physical therapy, 34% opted for yoga and meditation, and 5% opted for acupuncture [Table 4].

DISCUSSION
This global CP prevalence survey found that 19.3% Indian adult population suffers from CP. CP is a hugely growing problem. It becomes complex due to underreport, undertreatment, and low priority in developing countries. Half of the survey population belonged to the rural population who are suffering in silence probably due to nonavailability of effective and safe analgesic drugs. Pain is the most common reason for patients to seek medical advice globally. The World Health Organization estimates that 80% patients with severe pain never receive any adequate treatment. Shakespeare had said that “when sorrow comes, they not come as single spies but in battalions.” CP is often associated with depression, anxiety, anorexia, insomnia, fatigue, and accompanied by social challenges related to family, work, costs, finances. Various levels of understanding about the prevalence rate of CP exists. Using different definitions, the prevalence rate of CP has been found to vary from 8.7% to 42% in previous studies.[234567] India is a country with a large population of 1.2 billion. The results show that age-standardized prevalence of CP condition was 37.3% in developed countries and 41.1% in developing countries.[10] They found no obvious association between economic disparities and prevalence of CP.
This study shows a huge chronic burden in India by the prevalence rate of 19.3%, which translates into 180–200 million adults having CP. The exact figure cannot be calculated as this does not include patients admitted in hospital settings and the small sample of the total population. A later Indian survey reported a modest prevalence of CP as 13% in 2013.[11] There are many reasons for the underreporting of pain. Giving more emphasis on the disease management rather than pain, tolerating pain in silence, thinking that reporting about pain to busy physician is waste of their precious time or patients' coy predisposition. Some patients do not believe that analgesics can really relieve pain or some feel that it is easier to put up with pain rather than their side effects.
In United Kingdom, only backache has an economic burden of 1 billion pounds per annum. It is difficult to estimate the financial burden of CP in low- and middle-income countries like India. A meta-analysis found that prevalence of unspecified persistent pain may be about 34% in general population in these countries Table 5.[2] Since low- and middle-income countries population largely depends on government healthcare system for low-cost treatment, this prevalence study shall play an important role to emphasize on government and administrative agencies about the unmet need for the proper budget allocation, and organizing management plan for pain management at different healthcare levels.
Gender
There is a stronger gender predisposition observed in global CP survey, which found that the women suffer from CP almost double that of males. Evidence shows that women are more prepared to acknowledge pain than men (the stereotypical sexual roles).[121314] When men and women suffer the same painful state, women report greater frequency, intensity, and duration of pain. This finding corroborates the majority of other studies which compared prevalence of CP between sexes.[121314]
Age
A strong relationship was noted between increasing age and CP prevalence. The prevalence rate of CP was higher in patients aged over 60 years (23.5%) as compared to younger group (15.5%). The most frequent site of pain was knee (23.6%), followed by lower back indicating degenerative diseases due to wear and tear in elderly population Figure 4.

- Underlying etiology of chronic pain
Impact of pain
To study the impact of CP on the lives of respondents, they were asked a variety of life-related questions. Thirty-three percent respondents said that due to the pain they were not able to do their routine work. 25.5% had accepted pain as part of their lives. Nearly 14.1% of respondents were diagnosed with depression because of their pain. CP often is the leading reason that forced the patient to consult their primary care physician, and the burden of pain and depression in those with medical illness is particularly severe. Treating depression can decrease physical symptoms in many patients, but these patients may require a different pain strategy than those with depression alone.[151617]
Pain specialist consultation
71.2% CP sufferers were often visiting a general practitioner, but only 4.8% patients consulted a specialist pain physician. This shows a lack of awareness about “pain medicine” as a separate specialty among the population, and more so about the scarcity of pain physicians in the country. With the promotion of Department of Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy AYUSH by the Government of India (in terms of educational standards, quality control, and awareness) and opening up of Ayurvedic and Homeopathic centers in the private practice as well government healthcare system, more, and more people are increasingly favoring alternative therapies.[18]
Nonpharmacological or alternative methods
Thirty-five percent of pain sufferers were being treated with nondrug treatments such as massage and physical therapy. Yoga and meditation were being used by 34% respondents. Multidisciplinary and cognitive-behavioral approaches to the management of CP conditions are well documented in the literature to have significant and lasting effects. However, these approaches were used by very few patients may be due to nonavailability or inefficacy. Acupuncture is not much preferred as a modality for CP management in India. Only 5% respondents have ever used it.
Since drugs OTC are easily available, 35% of patients were using paracetamol, nonsteroidal anti-inflammatory drugs, or Cox-2 inhibitors. Prescription drugs including opioids, antidepressants, etc., were used by 37% respondents only. There is a general sense of opiophobia among the respondents. Opioids are not easily available in India due to various barriers at administrative, healthcare professional, and patient levels. Opioids can be accessed through the hospital dispensaries only after a physician consultation on a printed opioid prescription form issued in triplicate after furnishing the doctor's medical registration number and name legibly. Patient compliance with prescribed drugs (opioids) is another crucial issue which needs attention.[19]
CP is a neglected and undertreated issue, and although an important disease in itself with socioeconomic repercussions, is not given its due in budgetary and administrative setups. Various efforts at governmental, administrative, healthcare, and at public and patient levels are required through the advocacy groups to enhance the public awareness. A robust longitudinal study is required to estimate the exact current prevalence of CP in India. Unless governmental agencies need to put pain as a top public health priority, pain shall remain shall remain in the society as a demon unconquered.[19]
An important strength of this study is its sampling method and a uniform questionnaire. Face-to-face interviews helped in the accuracy of the study. The weakness lies in the fact that a sample of 4326 is too small to be representative of the entire country. The increased cost of these huge exercise without any government funding is also a limiting factor. More systematic and uniform methodical method covering the entire country (all states and union territories) and designed on multicentric study to determine the prevalence of CP is warranted. Quality of life should be assessed in more detail in future studies.
CONCLUSION
This study shows a CP prevalence of 19.3% in India. Rural population preferentially females suffer more unrelieved and untreated pain. The prevalence may increase significantly during next two decades, negatively impacting the global health status, man-hours, and overall economy of the nation. This prevalence study may serve as a benchmark of CP needs of the society and may help to initiate governmental efforts to mitigate the CP epidemic in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest. 20
Acknowledgments
This study was funded and supported by Mundi Pharma International. All the authors express deep gratitude and wish heart full thanks to Modi-Mundi Pharma India for their kind cooperation and support.
REFERENCES
- Pain as a human right: The 2004 global day against pain. J Pain Palliat Care Pharmacother. 2005;19:85-100.
- [Google Scholar]
- Asystematic review and meta-analysis of the global burden of chronic pain without clear etiology in low- and middle-income countries: Trends in heterogeneous data and a proposal for new assessment methods. Anesth Analg. 2016;123:739-48.
- [Google Scholar]
- Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16:769-80.
- [Google Scholar]
- Prevalence of chronic pain with neuropathic characteristics in the general population. Pain. 2008;136:380-7.
- [Google Scholar]
- Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287-333.
- [Google Scholar]
- Acomparison of chronic pain prevalence in Japan, Thailand, and Myanmar. Pain Physician. 2013;16:603-8.
- [Google Scholar]
- Common chronic pain conditions in developed and developing countries: Gender and age differences and comorbidity with depression-anxiety disorders. J Pain. 2008;9:883-91.
- [Google Scholar]
- Prevalence of chronic pain, impact on daily life, and treatment practices in India. Pain Pract. 2014;14:E51-62.
- [Google Scholar]
- Gender differences in chronic pain – Findings from a population-based study of Norwegian adults. Pain Manag Nurs. 2004;5:105-17.
- [Google Scholar]
- Chronic pain, associated factors, and impact on daily life: Are there differences between the sexes? Cad Saude Publica. 2012;28:1459-67.
- [Google Scholar]
- Chronic pain in South Australia – Population levels that interfere extremely with activities of daily living. Aust N Z J Public Health. 2010;34:232-9.
- [Google Scholar]
- Resilience does matter: Evidence from a10-year cohort record linkage study. BMJ Open. 2014;4:1-8.
- [Google Scholar]
- Factors associated with chronic pain in patients with bipolar depression: A cross-sectional study. BMC Psychiatry. 2013;13:112.
- [Google Scholar]
- Medication compliance in patients with chronic pain. Pain Physician. 2014;17:81-94.
- [Google Scholar]
- Chronic pain among children and adolescents: Physician consultation and medication use. Clin J Pain. 2000;16:229-35.
- [Google Scholar]






