Translate this page into:
Trocar Catheter: A New Alternative for Point of Care for Management of Pleural Effusion by Palliative Care Physicians
*Corresponding author: Nishkarsh Gupta, Department of Onco-Anaesthesia and Palliative Medicine, DRBRAIRCH, All India Institute of Medical Sciences, New Delhi, India. drnishkarsh@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Varshney H, Maurya P, Bharati SJ, Gupta N. Trocar Catheter: A New Alternative for Point of Care for Management of Pleural Effusion by Palliative Care Physicians. Indian J Palliat Care. 2025;31:88-9. doi: 10.25259/IJPC_303_2024
Dear Editor,
We would like to highlight the use of trocar catheters as a minimally invasive alternative for managing malignant pleural effusion (MPE) in palliative care, based on our experience with a critically ill cancer patient. MPE affects up to 20% of cancer patients, contributing to significant morbidity, including severe dyspnoea, pain and reduced mobility.[1] Traditional management with large-bore intercostal chest drains (ICDs) requires surgical incisions and muscle dissection, often resulting in complications such as hemothorax, pneumothorax, organ perforation and infections.[2] These risks can be especially burdensome for palliative care patients. While the use of pigtail catheters has been explored, there is limited research on the efficacy of trocar catheters compared to ICDs.[3] Studies, such as by Abusedera and Alkady, demonstrate that trocar catheters achieve high technical success rates (96%) with low complication rates, making them a viable alternative for MPE management in palliative care.[4]
We recently managed a 70-year-old female with advanced ovarian carcinoma and peritoneal metastases presenting with massive MPE, characterised by severe dyspnoea (Modified Medical Research Council scale grade 4) and intense chest pain (8/10 on the Numeric Rating Scale) [Figure 1]. Her pre-procedure Eastern Cooperative Oncology Group Performance Status (ECOG PS) was 3, reflecting significant functional impairment and limited tolerance for invasive procedures. Considering her frailty, recurrent MPE and preference for early discharge, a trocar catheter was chosen over an ICD.

- (a) is the baseline chest X-ray showing a complete whiteout lung with mediastinal deviation to the right side, (b) is a post-procedural chest X-ray showing the expansion of the left lung with trocar catheter in situ at the base of the left lung and (c) is chest X-ray after 7 days showing full expansion of left lung with trocar catheter in situ.
The procedure was performed using the Seldinger technique, with a 24-gauge trocar catheter inserted under sterile conditions [Figure 2]. Immediate drainage of 2 L of haemorrhagic fluid provided significant symptomatic relief, with her dyspnoea and chest pain reducing to 2/10. Her performance status improved from ECOG PS 3–2, allowing for greater independence. The total procedure time was 14 min, shorter than the approximately 15–30 min required for ICD placement, due to the streamlined nature of trocar catheter insertion, which avoids extensive muscle dissection [Table 1].[5]
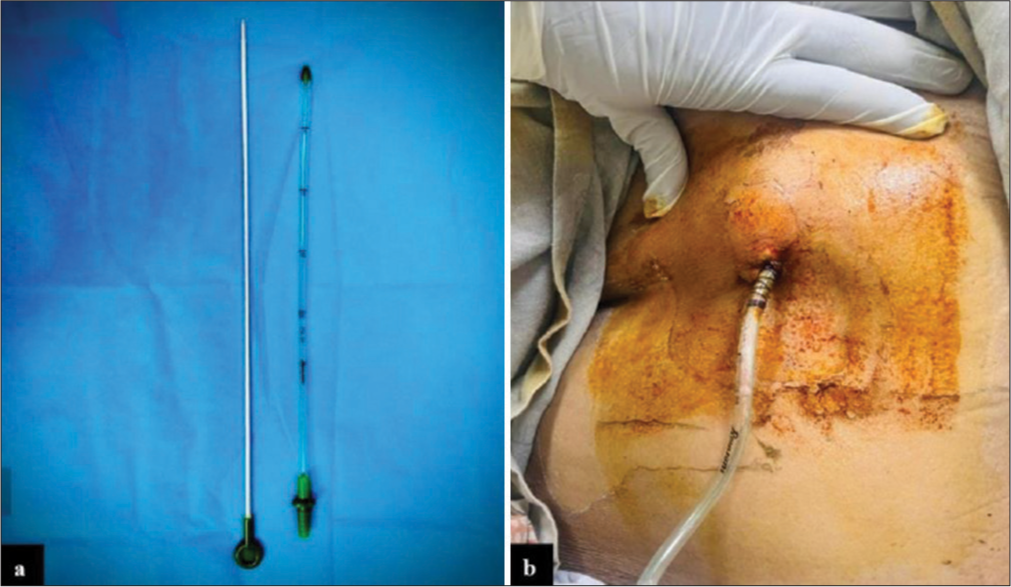
- (a) Shows the Trocar catheter with pointed tip encircled and (b) shows the patient having a 24 G trocar catheter in situ.
| Steps of procedure | Time taken in trocar catheter insertion | Time taken in ICD insertion |
|---|---|---|
| Painting and draping | 5 min | 5 min |
| Local Anaesthesia | 2 min | 2 min |
| Catheter Insertion | 1–2 min | 7–10 min |
| Suturing and dressing | 5 min | 5 min |
| Total | 13–14 min | 19–22 min |
ICD: Intercostal chest drain
The patient was monitored for 6 h post-procedure, remained stable and was discharged with instructions for catheter care and outpatient follow-up. On day 7, follow-up revealed full lung expansion, and the catheter was successfully removed [Figure 1]. The minimally invasive approach facilitated early discharge and reduced the overall burden of care, aligning with palliative care objectives.
Trocar catheters offer several advantages over traditional ICDs. They minimise procedural pain and scarring, providing rapid symptomatic relief and significant improvement in respiratory function and mobility as well as a reduction in psychosocial distress, including relief from anxiety and fear of suffocation. Compared to pigtail catheters, which may clog in haemorrhagic effusions, trocar catheters offer reliable drainage and are less invasive than ICDs, making them a compassionate choice for MPE management.[6]
The ease of use in non-surgical settings, coupled with reduced post-procedural care requirements, makes them practical for palliative care physicians. Post-procedural care was minimal, involving routine flushing with heparinised saline, incentive spirometry and chest physiotherapy. Furthermore, trocar catheters are cost-effective, priced at 500–600 Indian rupees (INR), significantly lower than pigtail catheters (~1500 INR) and comparable to ICDs (300–500 INR), making them a viable option in resource-constrained settings.
Despite these advantages, trocar catheters carry risks such as re-expansion pulmonary oedema, infections and catheter dislodgement. Challenges include loculated pleural effusions, coagulopathies and hemodynamic instability. Further comparative studies are needed to substantiate their efficacy and establish trocar catheters as a standard option for MPE management.
This case demonstrates that trocar catheters are a patient-centred, minimally invasive and cost-effective alternative for MPE management, particularly in palliative care settings. They align well with the goals of reducing procedural distress, enabling rapid recovery and improving quality of life. We advocate for further research into trocar catheters to validate their broader adoption and long-term outcomes in similar settings.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Guidelines of the European Respiratory Society and the European Society of Thoracic Surgeons for the Management of Malignant Pleural Mesothelioma. Eur Respir J. 2010;35:479-95.
- [CrossRef] [PubMed] [Google Scholar]
- Chest Tubes: Indications, Technique, Management and Complications. Chest. 1987;91:258-64.
- [CrossRef] [PubMed] [Google Scholar]
- Pigtail Tube Drainage in the Treatment of Spontaneous Pneumothorax. Am J Emerg Med. 2003;21:241-4.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-guided Pleural Effusion Drainage with a Small Catheter Using the Single-step Trocar or Modified Seldinger Technique. J Bronchol Intervent Pulmonol. 2016;23:138-45.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of Surgical Outcome of Trocar versus Blunt Dissection Technique for Intercostal Drainage Insertion: A Prospective Interventional Study. Int J Anat Radiol Surg. 2024;13:SO13-7.
- [Google Scholar]
- Pigtail Catheters vs Large-bore Chest Tubes for Management of Secondary Spontaneous Pneumothoraces in Adults. Am J Emerg Med. 2006;24:795-800.
- [CrossRef] [PubMed] [Google Scholar]






