Translate this page into:
Utility and Potential of Bedside Ultrasound in Palliative Care
Address for correspondence: Dr. Sanjay Thulkar; E-mail: sanjaythulkar@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Bedside ultrasound is an important tool in modern palliative care practice. It can be utilized for rapid diagnostic evaluation or as an image guidance to perform invasive therapeutic procedures. With advent of portable ultrasound machines, it can also be used in community or home care settings, apart from palliative care wards. Major applications of bedside ultrasound include drainage of malignant pleural effusions and ascites, nerve blocks, venous access, evaluation of urinary obstruction, deep vein thrombosis and abscesses. Bedside ultrasound leads to better clinical decision-making as well as more accurate and faster invasive therapeutic procedures. It also enhances patient comfort and reduces cost burden. However, use of bedside ultrasound is still not widespread among palliative care givers, owing to initial cost, lack of basic training in ultrasound and apprehensions about its use. A team approach involving radiologists is important to develop integration of bedside ultrasound in palliative care.
Keywords
Bedside ultrasound
Neurolysis
Palliative care
Ultrasonography
INTRODUCTION
Ultrasound (USG) is a simple yet versatile cross-sectional imaging modality with added advantages over other imaging modalities including lack of ionizing radiation, real time visualization, and easy availability. Moreover, USG examinations yield rapid results and are affordable as compared with computed tomography (CT) and magnetic resonance imaging (MRI). However, it is highly operator-dependent and has small but definite learning curve. The images are also not exactly reproducible and hence interpretation of USG images obtained by someone else may be difficult. It is limited by its small field of view and hence, large organ or area cannot be included in a single image. USG waves cannot travel through bone or air and hence, it is not suitable for body parts like head, lungs and bowel. These limitations of USG however do not make it a less-powerful imaging modality. Recent technological developments have improved the resolution and have added additional functional capabilities like Doppler studies for vascular evaluation, tissue harmonic imaging, contrast enhanced ultrasonography and elastography. Several of these can still be considered as investigational as there is insufficient evidence to support their routine clinical use.
Simplicity and cost-effectiveness of USG has liberated it from confines of radiology departments. Clinician performed USG is often referred to as clinical ultrasonography. Cardiologists and gynecologists are traditional non-radiology users of USG. With the advent of miniaturized portable USG machines, the modality has now found place in varied clinical specialities such as surgery, anesthesiology, gastroenterology, urology, and emergency medicine. These machines practically have most of the capabilities of traditional stand-alone USG machine.
Palliative care is intended not to cure the disease but to provide relief of distressing symptoms and promote comfort. Clinical ultrasonography has long been used in palliative care for basic diagnostic evaluation and for guiding therapeutic invasive procedures in patients with advanced cancer.[12] User-friendly portable USG machines are boon for palliative care of debilitated or non-ambulatory patients, as these can be effectively used not only in palliative care wards but also in hospice and home care settings.[34] However, it is not a widespread or standard practice.[1] Cost of USG machine when compared to other non-imaging equipment, lack of basic training, and consequent apprehension are still main hurdles in utilizing full potential of USG among palliative care practitioners.
There is new interest among interventional radiologists in palliative care.[5] Full potential of bedside USG in palliative care can be utilized if a good team is formed with radiology department. Active participation of radiologist is mandatory, at least during initial phase implementation. Availability and support of a skilled radiologist will always be needed in difficult situations that may be encountered. Team work is the key for successful integration of USG in palliative care.
Use of USG not only leads to better accuracy, success, and patient comfort; it also decreases procedure time and cost of the treatment.[1] Important areas where USG is useful in palliative care practice are enumerated in this review.
MALIGNANT PLEURAL EFFUSION
Malignant pleural effusions causing dsypnea are treated with thoracocentesis. Single-time needle aspirations are initially performed, however, recurrent fluid re-accumulations are common which require in dwelling catheters. Use of USG-guided percutaneous placement of small bore tubes, such as pigtail catheters, can be as effective as surgically placed chest tubes and also easier to maintain.[678] After adequate control of pleural drainage, these can also be used to perform chemical pleurodesis for lasting palliation of malignant pleural effusion.[9] Bedside USG, along with chest radiographs, is useful for initial evaluation and to select the patient for small bore catheter drainage of symptomatic malignant pleural effusion. Opacities diagnosed as pleural effusion on chest radiographs may actually contain large pleural deposits or primary tumor itself with little free effusion. This is easily detected on USG. Catheter drainage of such effusion is unlikely to help relieve dyspnea and hence, unnecessary drainage procedure can be avoided. USG can also demonstrate multiple loculations in pleural effusion, which is a relative contraindication for thoracocentesis [Figure 1].
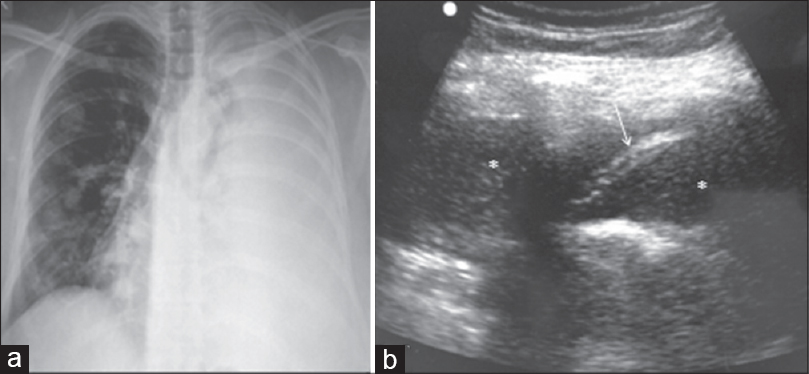
- Hemorrhagic pleural effusion: Chest X-ray (a) of a woman with breast cancer shows opaque left hemithorax with mediastinal shift to right. Multiple nodular metastases are also seen in right lung. Ultrasound of chest (b) confirms presence of pleural effusion. In addition, there are fine internal debris (asterisk) and septation (arrow) within
Once decided, USG is useful to determine the most appropriate site for drainage catheter insertion irrespective of traditional surface anatomy. This is especially important since malignant pleural effusions may not be free and largest component may be loculated anywhere in pleural cavity.
If the drainage has stopped but there is no resolution of dyspnea or radiographic evidence of pleural effusion, USG can be used to check the positon of catheter. Malignant pleural effusions often contain debris, blood clots, and tumor fragments and these can block catheters. Bedside USG is again useful to detect whether stopped drainage is because of complete evacuation or it is due to a blocked catheter. If USG shows presence of significant pleural fluid, the catheter can be flushed with saline or cleaned with soft guide wire. If drainage is stopped because of loculations or catheter malposition, bedside repositioning of the catheter or drainage of loculated fluid under USG guidance can also be attempted.[10]
MALIGNANT ASCITES
Tense, ascites-filled abdomen causes pain and distress which further debilitates patients condition. Drainage of tense malignant ascites or paracentesis is generally easy and does not require imaging guidance. It works in most patients and provides adequate symptomatic relief.[11] However, imaging is required if blind tapping fails. This may occur due to several reasons such as loculated ascites, ascites with large peritoneal, and omental deposits. USG can identify these conditions and also roughly quantify ascites. It also helps to determine most appropriate site of needle insertion and can further adds to the confidence if needle tip can be visualized in largest fluid pocket. At times, just gaseous or fluid distention of bowel due to obstruction or ileus may simulate ascites clinically. USG can confirm absence of significant ascites in these situations and helps avoid unnecessary blind taps. If significant ascites co-exists with bowel obstruction, USG guidance helps to avoid inadvertent puncture of distended bowel loops.
Following dry taps, patients are generally referred to interventional radiology departments for USG-guided paracentesis which take significant time of the interventional radiology facility and is also more expensive. Bedside USG-guided paracentesis is as effective or even better in terms of clinical outcomes and cost.[12] Long-term indwelling peritoneal catheters, tunnelled or non-tunnelled are good options to treat recurrent malignant ascites. It is beneficial symptomatically, avoids hazards of multiple repeated procedures, and reduces treatment cost.[13] These catheters can be safely placed using trocar-cannula or Seldinger techniques under USG guidance.[14]
USG-GUIDED NERVE BLOCKS
Majority of peripheral nerve blocks or joint injections for pain management can now be performed under USG guidance. These are more accurate than conventional blind, surface marking-based needle insertions, or those performed under c-arm fluoroscopy guidance as there is direct visualization of the nerves on USG. Real-time monitoring of needle insertion also make it faster and more accurate. Doing these procedures at bedside under USG guidance also obviate the need to shift the patient to minor OT, thereby saving precious OT time. This also enables more procedures to be performed in limited time. Overall, this translates into cost-effectiveness.[15]
From patients’ point of view, there is psychological benefit as being taken into OT leads to fear and anxiety in many. C-arm-guided procedures also require patients to maintain specific position during entire procedure and may also involve manoeuvers. This is difficult and uncomfortable to patients with painful bone metastases, pathological fractures, or advanced disease involving joints and nerves. USG-guided procedures generally do not need special positioning as there are no fixed needle entry points or directions. Hence, these are more comfortable to patients.[16]
Truncal blocks such as coeliac [Figure 2], superior hypogastric, ganglion impar neurolysis can be performed under USG guidance, although it is not as common as USG-guided peripheral nerve blocks. These blocks are not as simple and require a learning curve. There is also apprehension of needle injury to bowel, solid organs or vessels and possible complications. However, there is evidence that these procedures are safe even when performed at bedside under USG guidance.[17]
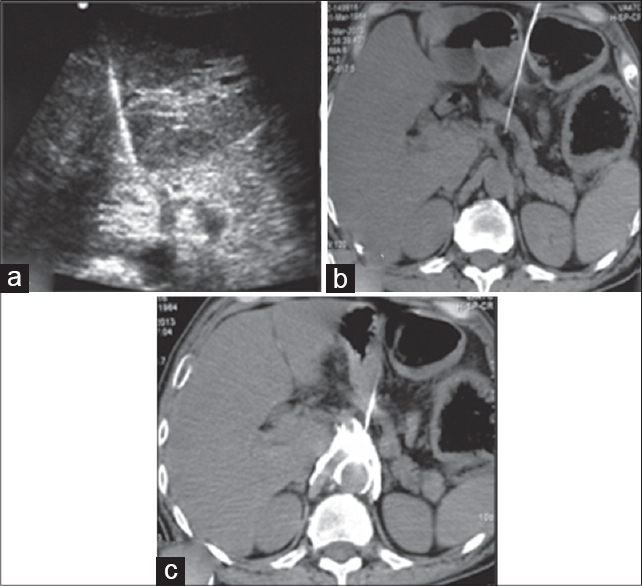
- Ultrasound (USG)-guided celiac plexus neurolysis: USG demonstrates needle tip on the right side of celiac trunk (labeled in a) which was confirmed on subsequently performed unenhanced computed tomography (CT) scan (b). Drug spread was seen as echogenic cloud on USG (a) which was verified on CT (c)
There are other advantages of doing these blocks under USG guidance. Unlike fluoroscopy which relies on bony landmarks, there is direct visualization of target area on USG. If there is complete infiltrations of target area with no space for spread of neurolytic agent (e.g. encasement of coeliac trunk by tumor or nodes), the procedure may not be clinically successful and hence can be avoided. This information is obviously not available on fluoroscopy and if performed, will result in failure. Ease of USG-guided neurolysis has also encouraged many to perform diagnostic blocks before definitive neurolysis. Long-acting local anesthetic such as bupivacaine is used onfirst attempt. If it results in temporary but satisfactory pain relief, neurolytic block with alcohol or phenol is performed next day.[17] If desired pain relief is not achieved with diagnostic block, neurolysis with alcohol or phenol is not done. This reduces number of unsuccessful blocks as well as complications related to alcohol or phenol injections.
Urinary obstruction
In patients with renal impairment or decreased urinary output, a quick bedside USG examination can determine if it is due to parenchymal renal failure or due to urinary tract obstruction resulting in hydronephrosis.[1819] In later situation, bedside USG-guided percutaneous nephrostomy can be performed to relieve obstruction [Figure 3]. In cases of lower urinary tract obstruction, USG can confirm massively distended urinary bladder as a cause for patient's discomfort or agitation. Suprapubic cystostomy can be performed under USG guidance.[18]
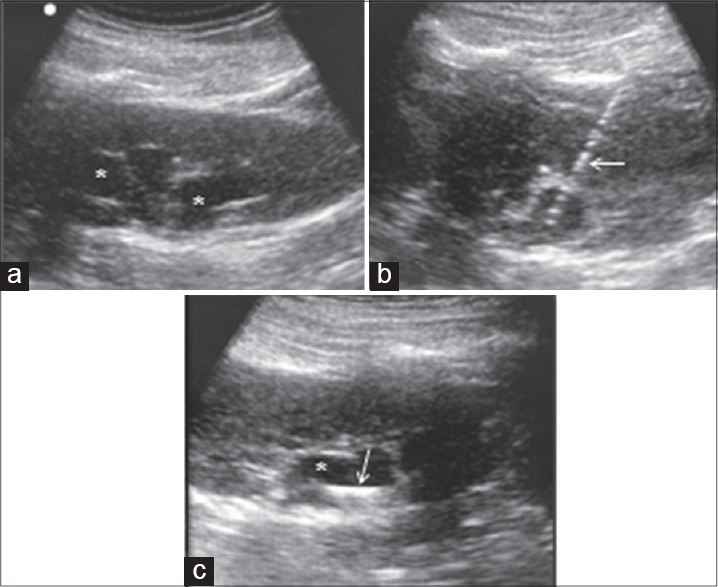
- Bedside ultrasound-guided percutaneous nephrostomy to relieve urinary obstruction in a woman with Ca cervix: Baseline USG demonstrates hydronephrosis (asterisk in a and c). Needle (arrow in b) was inserted into the pelvicalyceal system, followed by serial tract dilatation. After completion of procedure, loop of pigtail catheter is visualized within the pelvicalyceal system
Swollen painful limbs
Diffuse painful unilateral or bilateral limb swelling is a common situation in advanced cancers. It may be secondary to deep vein thrombosis, lymphatic obstruction due to metastatic lymph nodes, cellulitis, or generalized edema due nutritional or renal impairment. In case of uncertainty, bedside USG with color Doppler examination can diagnose deep vein thrombosis or any other local cause for limb swelling. This has important implication in choosing appropriate management.[1820] Edema of limbs may hamper insertion of venous lines as superficial veins cannot be well appreciated in edematous limbs. USG-guided venous catheterizations are obviously the choice in these situations.[21]
Miscellaneous conditions
Infective collections in abdomen or thorax can be detected and localized with USG. Depending on the size and location of such collection, one time aspiration or catheter drainage of thoracic or abdominopelvic collections can be performed under USG guidance.
Painful, focal bone or soft tissue metastases are generally treated with opioids and palliative short-course radiotherapy. Metastases refractory to these can be treated with USG-guided radiofrequency ablation in selected patients.[22]
Occasionally, biopsy or fine-needle aspiration cytology (FNAC) of the tumor or lymph nodes may be required to initiate palliative chemotherapy, if it has not been performed before. If there is sudden deterioration of general condition of patients with abdominal or pelvic malignancy, bedside USG may also be required to assess extent of primary or metastatic disease or its complications.[18]
CONCLUSION
USG has important role in several diagnostic and therapeutic procedures in palliative care practice. Use of USG not only leads to better accuracy, success, and patient comfort but also decreases procedure time and cost of the treatment. Routine use of USG in palliative care with active participation of a skilled radiologist is highly desirable.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Hospice and palliative medicine ultrasound: A new horizon for emergency medicine? Acad Emerg Med. 2010;17:330-2.
- [Google Scholar]
- Ovarian cancer and ascites: A questionnaire on current management in the United kingdom. J Palliat Med. 2006;9:1264-70.
- [Google Scholar]
- The use of bedside ultrasound and community-based paracentesis in a palliative care service. J Prim Health Care. 2014;6:148-51.
- [Google Scholar]
- Palliative ultrasound for home care hospice patients. Acad Emerg Med. 2010;17:293-6.
- [Google Scholar]
- Palliative care: A frontier that should be explored by radiologists. Can Assoc Radiol J. 2014;65:289.
- [Google Scholar]
- Use of indwelling pleural catheter in the outpatient management of recurrent malignant pleural effusion. Arch Bronconeumol. 2009;45:591-6.
- [Google Scholar]
- An update in the management of malignant pleural effusion. Indian J Palliat Care. 2011;17:98-103.
- [Google Scholar]
- Use of small-bore vs large-bore chest tubes for treatment of malignant pleural effusions. Chest. 2001;120:19-25.
- [Google Scholar]
- Pleurodesis for effusions in pediatric oncology patients at end of life. Pediatr Radiol. 2007;37:269-73.
- [Google Scholar]
- Prospective randomized trial of intrapleural bleomycin versus interferon alfa-2b via ultrasound-guided small-bore chest tube in the palliative treatment of malignant pleural effusions. J Clin Oncol. 2004;22:1228-33.
- [Google Scholar]
- Medical and palliative management of malignant ascites. Cancer Treat Res. 2007;134:459-67.
- [Google Scholar]
- Clinical outcomes after bedside and interventional radiology paracentesis procedures. Am J Med. 2013;126:349-56.
- [Google Scholar]
- Peritoneal catheter for continuous drainage of ascites in advanced cancer patients. Support Care Cancer. 2008;16:975-8.
- [Google Scholar]
- Placement of a permanent tunneled peritoneal drainage catheter for palliation of malignant ascites: A simplified percutaneous approach. J Vasc Interv Radiol. 2002;13:379-83.
- [Google Scholar]
- Bedside ultrasound: A radiologic boon for placement of complex nerve blocks for abdominal malignancies. J Palliat Med. 2011;14:1198-9.
- [Google Scholar]
- Bedside ultrasound-guided celiac plexus neurolysis in upper abdominal cancer patients: A randomized, prospective study for comparison of percutaneous bilateral paramedian vs. unilateral paramedian needle-insertion technique. Pain Pract. 2014;14:E63-8.
- [Google Scholar]
- Early ultrasound-guided neurolysis for pain management in gastrointestinal and pelvic malignancies: An observational study in a tertiary care center of urban India. Pain Pract. 2012;12:23-32.
- [Google Scholar]
- Bedside ultrasound--experience in a palliative care unit. Eur J Cancer Care (Engl). 2009;18:642-4.
- [Google Scholar]
- Improvement of transurethral catheterization in male patients. Palliat Med. 1999;13:261-2.
- [Google Scholar]
- Venous thromboembolism: A common and preventable condition. Implications for the home care nurse. Home Healthc Nurse. 2007;25:94-100.
- [Google Scholar]
- Critical review and state of the art in interventional oncology: Benign and metastatic disease involving bone. Radiology. 2012;262:765-80.
- [Google Scholar]






