Translate this page into:
21st International Conference of Indian Association of Palliative Care,14th to 16th February 2014, Acharya Harihar Regional Cancer Centre, Cuttack, Odisha, India: ORAL PAPERS
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
ESTABLISHING PALLIATIVE CARE SERVICES AT RURAL HOSPITALS OF THE EMMANUEL HOSPITAL ASSOCIATION
Dr. Ann Thyle
E-mail: ann@eha-health.org
Introduction: EHA's 20 hospitals, located in 14 north Indian states, has a vision to provide high quality, affordable medical care to the rural poor at remote locations. Cultural attitudes, low literacy rates, inability to access care, lack of knowledge, and crushing poverty results in unimaginable suffering.
Objectives: Palliative care was recognized as a gap in EHA's existing medical services, a huge need as cure is usually impossible because of late presentation and limited treatment options. Our objective was to establish palliative home-based, outpatient and inpatient care, accessibility to opioids, extensive training, income generation, and bereavement support.
Methodology: Since 2010, palliative care services have been established at three rural hospitals in Uttar Pradesh (UP); and one each in Assam, Bihar, Maharashtra, and Delhi. Most care is provided at home in villages located 25-50 km around the hospital. Awareness was raised among healthcare providers, village leaders, and communities. Inpatient units were established for acute care. Opioid licenses were obtained at two hospitals in UP. Care packages and support for children's education is provided when the main wage earner dies. Two income generation projects were started to support families.
Results: The rural poor in our locations have benefited immensely from focused palliative care, especially symptom control, and the varied support given to families. The concept of palliative care is spreading in an ever widening circle in areas with no knowledge of this type of care.
Conclusion: Providing holistic and palliative home care to neglected north Indian rural populations is critical to alleviate suffering and raise awareness.
PROSPECTIVE AUDIT FOR PAIN CONTROL
Sanghmitra Bora
E-mail: sanghamitrabk@gmail.com
Background: For a country like India where 80% of cancer patients report to the cancer hospital at an advanced stage and the concept of Palliative Care is synonymous with terminal care, it is necessary to propagate the right concept of pain management and palliative care amongst those who are suffering from the disease and also those who are involved in treating.
Objectives: The objectives of the audit are to stress the importance of treating pain at the onset, improve the knowledge about pain, its management, and impart scientific skills of measuring pain and its intensity which is limited amongst doctors and nurses.
Materials and Methods: A standard of 100% was set. A pain screening questionnaire was designed to be filled up by the attending physicians/oncologists at the outpatient clinics. The responses were compared with the outpatient department (OPD) record list in the palliative care unit (PCU) on a day-to-day basis. As such, the number of patients referred for pain management was then compared against the standard. Conscious patients of all ages with a sound state of mind were included.
Results: 66.37% of patients (231/348) were referred to the pain clinic in the first round of the audit as compared to 90.93% in the second round.
Conclusions: The audit reflected scope of improving practice in many areas for getting referral for pain management early on presentation. In this audit, patients from the OPD were included. It is now anticipated that if those in the inpatient and home care were also taken, the results may have further declined.
STUDENT'S PALLIATIVE CLUB - A NEW HUB FOR THE PALLIATIVE MEDICINE
Mr. Tigi Thomas M A
E-mail: tigipurayil@gmail.com
Introduction: Palliative care is a multidisciplinary team work aimed at mitigating the pain and suffering of the people. Despite the efforts made by this multidisciplinary team, only less than 10% of the deserving gets the holistic service and aid. The main reason is the lack of awareness about palliative medicine. So a new hub is needed to provide palliative care to all the needy.
Objectives: (1) To make the students become a member of palliative multidisciplinary team. (2) To develop in the students a compassionate and empathetic attitude towards the ailing and suffering.
Methods: Awareness program Special training program Patient's identification program World Palliative Day program
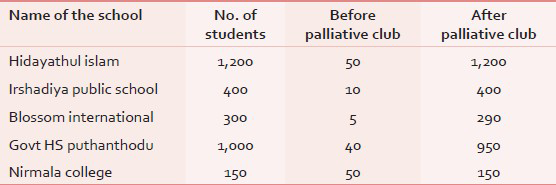
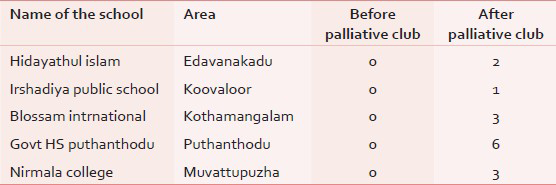
Results: Clear knowledge about the palliative care for the next generation [Table 1]. As per the data given above shows, through the palliative club our next generation can get a clear knowledge about the palliative medicine. A large improvement in patients’ rRegistration: A large improvement in patients’ registration [Table 2]. As per the data, within a period of just a month, 15 patients have already registered in Alpha Palliative Care through the palliative club. Through special training programs, students are empowered as a medium and through them the ailing and deserving persons will gain due benefit.
Conclusion: The palliative medicine is a new and emerging medical field. So the awareness about the same is limited. My firm belief is that more awareness and can generate more generous individuals. Through students palliative club we can enlighten our young generation to lighten the pain and suffering and also can generate better generosity and acceptance to the palliative medicine.
ORAL MORPHINE UTILIZATION DURING ADJUVANT RAPIDARC IMRT IN ORAL CANCERS: NEED FOR ROUTINE PALLIATIVE CARE INTEGRATION
Dr. Biji MS, Ms. Sindhu NR, Dr. Santam Chakraborty, Dr. Geetha M, Ms. Suja CA, Ms. Liji Bineesh
E-mail: bijims@gmail.com
Introduction: Use of adjuvant radiotherapy in oral cancer patients can be associated with severe mucositis.
Objectives: To report the patterns and efficacy of morphine use for pain control in this population.
Methods: Data regarding morphine use during adjuvant RapidArc intensity-modulated radiation therapy (IMRT) for oral cancer patients was abstracted. Toxicities, treatment compliance, and duration were compared across patients who did or did not receive morphine.
Results: Seventy patients with oral cavity cancers were treated between February 2012 and July 2013. Sixty percent of the patients were males and the median age was 60 years. Commonest sites were oral tongue (39%) and buccal mucosa (28%). Stage IV disease was seen in 62% patients. Oral morphine was required in 34 patients (48%) during the course of radiotherapy. Morphine was started at a median duration of 3.7 weeks after the start of radiotherapy and the median duration of use was 37 days. Patients receiving morphine had higher incidence of Grade III mucositis (77 vs 37%, P < 0.001). However, there was no increase in treatment time (mean increase 1.03 vs 1.9 days, P = 0.52), or difference in treatment completion rate in patients receiving morphine or not (90 vs 88%).
Conclusion: Although patients had more severe mucositis, use of oral morphine ensured that there was no increase in treatment time or incompliance rates. Integration of palliative care services and pain assessment is therefore useful for timely delivery of curative radiotherapy in this setting.
WHAT CAUSES STRESS AMONG PALLIATIVE CARE WORKERS? AND HOW THE WORKERS LOOK AFTER THEMSELVES?
Ravinder Mohan
E-mail: ravindermohan@cansupport.org
Introduction: Some stress is a part of life, however, palliative care workers face death and dying on a regular basis. The workers often connect the work situations to their own personal life and carry the burden of helplessness home. Many cases are tragic and leave deep scars like death of a young lone bread winner, an only child, or a newlywed spouse.
Objectives: To find what causes stress among the palliative care workers on a regular basis. Evaluate the personal experiences of these workers to learn how to manage these stressful situations and prevent burnout.
Methods: Used included structured questionnaire. This questionnaire was tested on five persons. Fifty-four palliative care workers (doctors, nurses, and counselors) participated in this study.
Results: Common stressors found were travelling long distances, too much of documentation, multiple issues of the families at the end of life and inadequate symptoms management. Common destressors were music, prayers, and regular physical exercise.
Conclusions: The sooner we identify the stressors and the effective destressors, the less the anguish to the palliative care workers. Lowering the level of stress in the workers translates into more effective work. This means better quality of life for the palliative care providers and their patients.
A STUDY TO EVALUATE THE ADVANTAGE OF MUSIC THERAPY IN PAIN AND PALLIATIVE THERAPY
Santha Swarupa
E-mail: ravindermohan@cansupport.org
Introduction: Pain is an unpleasant sensation felt only by the individual, but it causes agony to the patient as well as her/his caregivers due to the sight of suffering.
Objectives: To evaluate the effect of music therapy on drug resistant cancer pain.
Methods: Thirty-five patients suffering with different types of carcinomas, who were already receiving appropriate pain medications, were selected for this observational 12 week study. Initially through a pretest questionnaire we assessed the patient's emotional and psychological condition and recorded patient preference regarding music. Accordingly, music therapy was administered.
Results: After our intervention, Edmonton's symptom scale was used on patients to assess symptom relief. More than 50% of cases showed improvement in pain and anxiety. Well-being, sleep, and diet intake also showed marked improvement.
Conclusion: Appropriate use of music therapy can provide additional symptom relief beyond that achieved by the pharmacological measures and may have the added benefit of achieving relaxation and mood elevation. Further studies are needed.
REHABILITATION OF PALLIATIVE CARE PATIENTS AND THEIR FAMILIES
Charanjeet
E-mail: ravindermohan@cansupprt.org
Introduction: When we visit patients at their homes, we come across families whose earning member is very sick or he/she is jobless because he/she has to take care of their loved one. As we visit patients regularly, it is easy to assess the need for economic rehabilitation by seeing their living conditions, no food and medicines in the house, rented house, and many dependents. The home care team makes an assessment and talks to the family about what kind of work they can do so that a source of earning can be started.
Objective: To assist the families to start earning again, after a serious illness or bereavement.
Method: Counseling for the motivation to carry on in life, economic assessment, assessment of education, job options, and seed grants. Few were supported by giving them a cart with materials to sell, or buy a rickshaw, a sewing machine, etc.
Result: Most of the families were able to fend for themselves and would lead their lives normally.
Conclusion: The families had great satisfaction and could take care of the patient and the families in a much better way. Even after the death of the patient the family members had a source of livelihood. Therefore, all organizations that are providing palliative care should have funds or resources for rehabilitation to provide holistic care to the patient and their families.
TO STUDY THE EFFECT OF MULTIMODAL MANAGEMENT OF LYMPHEDEMA ON POST-MASTECTOMY PATIENTS
Shashi Chandra
E-mail: ravindermohan@CanSupport.org
Introduction: Lymphedema is a common complication following mastectomy in breast cancer patients. It causes discomfort, disability, and disfigurement and affects the patient's quality of life. Multimodal treatment consisting of skin care, exercise, massage, and compression, helps in the management of this problem.
Method: Fifteen post-mastectomy patients with upper limb lymphedema, who were being followed-up by our palliative homecare team were taught skin care, exercise, massage, and advised compression garments. The patients were followed-up weekly for 2 months. The lymph edematous limbs were measured on each visit (measurement according to Australasian Lymphology Association technique).
Result: Majority of patients benefitted from this treatment.
Conclusion: Multimodal management of lymphedema is helpful in majority of patients. However, intensive education of patients is required and they have to follow these principles of care throughout their life.
A COMPARATIVE STUDY OF FATIGUE AMONG CANCER PATIENTS WITHOUT DIABETES AND CANCER PATIENTS WITH DIABETES IN A PALLIATIVE CARE SETUP
Prakash S
E-mail: onelifeprakash@gmail.com
Introduction: Fatigue is the most common and disgusting symptom among patients with cancer as well as diabetes. To patients and their families, fatigue can be an overwhelming symptom impairing quality of life. When a patient has diabetes and receives palliative care for some other disease, fatigue is almost present among them and its nightmare for the patient, family as well as to the treating doctor.
Objectives: To assess the prevalence of fatigue among patients who has diabetes and receive palliative care for other disease. To assess the severity by using Functional Assessment of Chronic Illness Therapy (FACIT)-fatigue scale. To measure the outcome of palliative fatigue management among these patients.
Methods: Definition and criteria for fatigue ware identified. Qualitative difference between fatigue in cancer patients and healthy controls have been proposed. Then 25 cancer patients without diabetes and 25 cancer patients with diabetes in a palliative care setup have been identified. FACIT-fatigue scale version 4 has been adopted for the study with assessment of physical, social, emotional, and functional well-being and additional concerns. Then thisopen, qualitative and prospective study is conducted among both in- and outpatients of RMD Pain and Palliative Care Center.
Results: Fatigue among cancer palliative care patients without diabetes is about 89%. Fatigue among cancer palliative care patients with diabetes is about 100%. Seventy percent of cancer palliative care patients with diabetes have more severe fatigue symptoms than patients without diabetes.
Conclusion: Fatigue is very common in cancer palliative care patients and most of the time it is due to physical and psychological symptoms. Fatigue is also a common disabling symptom in patients with diabetes. This can be due to because of disease, diabetes treatment, other comorbid conditions, and complication of diabetes. When a patient has both diabetes and cancer this symptoms of fatigue is very severe. Fatigue has strong impact in patient's daily performance, sense of well-being, and relationship with family and friends. Since fatigue among palliative care patients are multifactorial and the symptoms are not constant, intervention results are not encouraging. Single approach cannot manage fatigue in this group of patient. The fundamental principle of holistic management must remain foremost in fatigue management. The effects and side effects of all interventions must be weighed before proceeding, and their various impacts require regular and frequent review.
Fatigue Questionnaire:
International Classification of Diseases (ICD) 10 fatigue criteria:
Following symptoms have been present every day or nearly every day during the same two weeks period.
Do you have generalized weakness or limb heaviness?
Do you have diminished concentration or attention?
Do you have decreased motivation or interest to engage in usual activities?
Do you have insomnia or hypersomnia?
Do you experience sleep as unrefreshing or non-restorative?
Do you suffer from perceived need to struggle to overcome inactivity?
Do you have marked emotional reactivity (sadness, frustration, or irritability) to feeling fatigued?
Do you have difficulty in completing daily task attributed to feeling fatigued?
Do you perceive problems with short-term memory?
Do you have post-exertional fatigue lasting several hours?
The symptom cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
There is evidence from history, physical examination, or lab findings that symptoms are consequences of cancer or cancer therapy.
The symptoms are not primarily a consequence of comorbid psychiatric disorders such as major depression, somatization disorder, somatoform disorder, or delirium.
Physical symptoms: Loss of physical performance/inability to complete tasks/decreased strength/tachycardia with exertion and anemia/increase shortness of breath.
Psychological and affective symptoms: Lack of energy/loss of motivation/depression/sadness/anxiety/feeling of “there is no energy left”.
Cognitive Symptoms: Difficulty in making decision/inability to think clearly.
Causes of Fatigue:
Stress and central nervous system (CNS)
Disease and treatment related factors
Individual differences.
Management: Whole person approach
Communication and education
Balancing activity and rest
Pharmacological
Management of stress
Managing disease and treatment-related factors
Sample size: 200
Duration of study: 2 months
Protocol: Background
Define fatigue and study criteria
Aims, objective, and questionnaire
Participants
Method
Statistics
Result
Discussion
Conclusion
References and footnotes
PERSPECTIVES OF ORTHOPEDICIANS ON PAIN MANAGEMENT IN OSTEOARTHRITIS - A QUALITATIVE STUDY
Jose Austine, Shoba Nair
E-mail: joseaustin3@hotmail.com
Introduction: Osteoarthritis (OA) is the result of a degenerative process and is the most common form of arthritis and one of the leading causes of pain and disability worldwide, which in turn significantly impair the quality of life in patients. It would therefore be imperative to know the treating doctor's perception about pain relief in this group of patients.
Objective: To assess orthopedician's perspectives on pain management in osteoarthritis pain.
Methodology: In this qualitative study, a semistructured interview was conducted on 15 orthopedic surgeons from a tertiary care hospital and audio recorded simultaneously. The audio recording was transcribed verbatim and a grounded theory approach was used to code the data. An inductive approach using thematic analysis was used to manually analyze the data.
Results: Five themes emerged.
(1) Participants said that osteoarthritis produces significant disease burden and impaired quality of life in patients. (2) Pain management usually comprised of a multipronged method of treatment with more emphasis on physiotherapy and surgery and less on analgesics. The doctors felt that patients usually demand immediate pain relief. (3) Doctors usually preferred a practice of individual discretion as against any guideline or protocol; however, a few felt that there was a need to systematize pain management. (4) The participants all agreed that counseling would help in the improvement of the quality of life of patients. (5) All participants put forward several barriers for optimal pain management.
Conclusions: There is a need for a patient-centered approach to pain management in osteoarthritis. Comprehensive osteoarthritis pain management involving a multidisciplinary team will help in providing better pain relief and in turn improve the quality of life in osteoarthritis patients. There is also a need to correlate the doctor's perspectives with those of the patient.
ROLE OF PHYSIOTHERAPY ON IMPROVING PHYSICAL AND PSYCHOLOGICAL SYMPTOM DISTRESS IN PALLIATIVE CARE
Mugdha Vaidya, Priyadarshini Kulkarni, Nandini Thatte, Vrushali Anavkar
E-mail: mugdha.vaidya@ciplacare.com
Introduction: Physiotherapy is known to promote, maintain, and restore physical well-being of patients; it prevents and compensates for deformities already set in due to disease. Physiotherapy improves and enhances the physical abilities of patients, thus improving the quality of life, in a number of diseases, including life-limiting ones.
Objectives: The present study was aimed at assessing the effect of physiotherapy on the quality of life of cancer patients undergoing palliative therapy.
Methods: The study was conducted on consenting inpatients who were rated to have a performance between 30 and 60 on Karnofsky's Performance Scale, a very wide ranging scale assessing physical ability. The study was an open, randomized, parallel comparison of physiotherapy with concomitant control. Intervention consisted of a battery of exercises customized to suit individual patients, administered 6 days a week for a period of 3 weeks. Quality of life was measured weekly using the Rotterdam Symptom Checklist, a comprehensive instrument that is reliable and robust and has psychometric properties too.
Results: Physiotherapy was found to cause an improvement in the quality of life of patients. There was a significant enhancement of physical abilities and a marked improvement of the patients. Patients receiving physiotherapy had a lower physical symptom distress, lower psychological distress, increased activity level, and overall valuation of life.
Conclusions: It is concluded that physiotherapy is an important complement of conventional palliative care and should be incorporated for all patients who are able to participate in the exercise sessions
MOBILIZING COMMUNITY POTENTIAL FOR PALLIATIVE CARE
Hamza KV, Suresh Thaliyaril
E-mail: dnipcare@gmail.com
Introduction: The people in the metropolitan city of Delhi are in the mad rush for livelihood, shelter, and comfort. Extremities of weather added with the commuting issues, the stressed Delhiites seldom find time or convenience to think beyond their own complex issues. Mishaps, tragedies, and sufferings of prolonged diseases aggravate the already isolated stressful lives. Stakeholders are many for human immunodeficiency virus (HIV), AIDS, cancer. etc., on the curative scene, but prolonged medical conditions of bedbound or wheelchair bound lives consequent on tragedies, accidents, eruption of genetic, or incurable chronic diseases mar the prospect of even living, forget about quality living. On the realization of bad prognosis or incurability of the disease, the initial crowd of relatives, friends, and well-wishers also vanishes in the thin air. Deserted by even own family members, the solitary state and the plight of such patients in the big cities pose a big question mark before the society as a whole. In addition, the woes of neglect and humiliation met by our ageing population craving for a drop of care and support from the near and dear is yet another tipoff the iceberg in this capital city.
Objective: Inculcate empathy and fellow feeling to translate into care and concern for long term, bedridden, terminally ill patients including cancer and geriatric patients among the common people through community mobilization initiative under DNipCare. Sensitization and propagation of importance of community participation in palliative care to ensure availability, quality, and consistency of service delivery at the doorsteps of the patients. Emancipation from the taboo of unethical and superstitious beliefs, attitudes, and practices associated with any or every disease.
Methods: Conducting sensitization and propagation programs with no cost involvement; targeting people from all walks of life by focusing on specific institutions, groups, and congregations.
Area of operation chosen for sensitization and propagation are:
Churches, temples, gurudwaras, and other religious congregations
Educational and professional Institutions (schools, colleges, universities, and Indian Institute of Technology (IIT))
Sociocultural organizations
Resident welfare associations
Professional groups (nurse groups, police group)
Fairs and festivals including health exhibitions and India International Trade Fairs
Results: The pockets we focused remain sensitized to the plights of the patients. Participation of different communities including students in palliative home care. Resource mobilization and sensitized groups of audio visual and print media.
Conclusion: A paradigm shift from I, me, myself to we, us, ourselves is possible especially in the interest of the suffering patients through inexorable efforts.
A COMPARATIVE STUDY BETWEEN DEXMEDETOMIDINE VS CLONIDINE AS ADJUVANTS TO ROPIVACAINE 0.75% IN EPIDURAL ANESTHESIA
Nirlipta Ku Behera, Patel PK, Panda P
E-mail: daya8310@gmail.com
Introduction: In an effort to find better adjuvant in regional anesthesia (RA) with sedation, stable hemodynamics and ability to provide smooth, prolonged, postoperative analgesia; many drugs have been studied. With opioids producing many side effects, α2 agonists having analgesia, sedation, and better hemodynamic stability may be preferable. Decreased anesthetic, analgesic requirements, and augmentation of local anesthetics by α2 agonists is due to hyperpolarization of nerve tissue by altering transmembrane potential and ion conductance at locus ceruleus in brainstem.
Objectives: To study and compare analgesic, sedative, and hemodynamic properties of dexmedetomidine with clonidine as adjuvant in epidural anesthesia.
Methods: After approval from ethics committee, 50 patients, American Society of Anesthesiologists (ASA) Grade I and II aged 20–60 years undergoing surgery below the umbilicus were enrolled. Patients with contraindications for neuraxial block are excluded. Patients randomly allocated into two groups, Group-RD (ropivacaine + dexmedetomidine), Group-RC (ropivacaine + clonidine). Group-RD received 17 ml 0.75% ropivacaine + dexmedetomidine 1.5 μg/kg and Group-RC 17 ml ropivacaine 0.75% + clonidine 2 μg/kg.
Block characteristics recorded: Onset of analgesia, highest dermatomal level, complete motor blockade, two-segment regression, regression to S1 level, and time to complete recovery. Sedation and motor blockade assessed by five-point scale and modified Bromage scale, respectively. Hemodynamic parameters recorded every 5 min.
Results: Group-RD resulted in early onset analgesia and higher dermatomal level compared to Group-RC (P < 0.05). Higher sedation score, time to 2 segment regression and return of motor power to Bromage 1 are more significant in Group-RD than in Group-RC (P < 0.05).
Conclusion: We conclude that dexmedetomidine is a better adjuvant than clonidine in epidural anesthesia in terms of better cardiovascular system (CVS) stability, sedation, and analgesic properties.
HOLISTIC CARE OF RURAL ELDERLY - AN INTERVENTION-BASED SURVEY
Priya Khanna, Abhijit Dam
E-mail: priya40@gmail.com
Introduction: Rural elderly are cared for by their families, but it does not put them in any more of an advantageous position than their urban counterparts. Greater life expectancy, changing attitudes, and rising costs are few of the factors that play a role in making the position of elderly more vulnerable.
Objectives: This voluntary, intervention-based survey was designed to address the ‘holistic’ needs of the rural elderly and to address the potentially ‘treatable’ and ‘correctable’ issues during the interview.
Methods: A simple questionnaire was designed which attempted to incorporate all aspects of “holistic care”–physical, environmental, emotional, and spiritual. Amongst identified clients, 13 agreed to participate in the survey. Clients needing interventions were followed-up regularly. Interventions such as using analgesics to reduce pain, supplements of vitamins, discussing sleep hygiene, treatment of hypertension, and others were carried out.
Results: Patients were between 60 and 104 years of age. All of them followed Hinduism. Son and daughter-in-law were primary caregivers in almost all cases. Eight clients acknowledged that they had physical problems interfering with activities of daily living. Most of them had no further expectations. All believed that religion provided some satisfaction. Following interventions, the quality of life (QOL) was measured; the results of which will be discussed in further detail.
Conclusions: Physical and emotional difficulties are often ignored in rural elderly. However, interventions that alleviate physical symptoms improve outcomes and QOL inventory (QOLI).
EFFICACY AND SAFETY OF SCRAMBLER THERAPY IN THE MANAGEMENT OF ONCOLOGICAL PAIN
Komal Kashyap, Sushma Bhatnagar
E-mail: komalkashyap009@gmail.com
Introduction: Scrambler therapy (ST) is a noninvasive approach to pain control that interferes with pain signal transmission by providing 16 nonlinear waveforms that change continuously.
Objective: The main objective of the study is to assess the effect of ST upon pain perception, quality of life (QOL), therapy toxicities, and impact on medicine dosages.
Method: ST consists of 10 treatment sessions for 40 min followed by weekly follow-ups for 2 weeks. Pain intensity was assessed daily with a visual analog scale (VAS) pre- and post-therapy. QOL was assessed with a World Health Organization (WHO) QOL score form which was filled by the patient on four occasions, that is, first session, tenth session, and both follow-ups.
Result: According to a case report of a patient who was admitted for left lower alveolus cancer and was being administered with nonsteroidal anti-inflammatory drugs (NSAIDS), opioids for pain control further, left mandibular nerve block was given but no major relief was observed; thus ST was planned. During treatment, visual analog score (VAS) score decreased on the very 1st day from 8 to 5 out of 10, which is nearly 50%; it further decreased to 1 after three to four sessions and was nearly stagnant at 1 even after 10 sessions and two follow-ups, that is, 90% of reduction in pain with 0% side effects was observed. Patients with visceral, bony, and mixed pain were also observed showing 50–60% reduction in pain.
Conclusion: In conclusion, ST can be a good option for the oncological pain patients, who responded poorly to conventional treatments with a reduction of an average of 70% in all kinds of oncological pains.
MANAGEMENT OF FUNGATING WOUNDS IN CANCER PATIENTS WITH HONEY DRESSINGS
Sr. Shindu Raj
E-mail: ravindermohan@cansupport.org
Introduction: Fungating wounds often foul smell, have exudates and may bleed excessively. Because of these factors the patients face isolation and have poor self-image. Honey dressing is a novel way of taking care of these difficult problems.
Objective: To study the efficacy of honey dressings on fungating wounds.
Method: Ten patients with fungating wounds had the wounds dressed with honey. Good quality honey is easily available in market and neem honey is available with a chemist. The care givers were taught to do dressing with honey. The patients were followed-up for 2 weeks and wounds were examined every alternate day.
Result: Honey dressings help to take care of the major problems associated with fungating wounds like foul smell, exudates, and excessive bleeding. Both patients and caregiver were satisfied with honey dressing, as assessed by an objective checklist.
Conclusion: Honey dressings are effective in care of the problems associated with fungating wounds. This is a culturally acceptable form of wound care.
EVALUATING THE NEEDS OF ADOLESCENT CHILDREN AND THEIR CAREGIVERS: TO IMPROVE THEIR QUALITY OF LIFE
Pradnya Talawadekar, Melba Cardoz, Sushil Nikam
E-mail: childrenspalliativecare@gmail.com
Introduction: The life limiting conditions bring with them pain, discomfort, hospitalizations, and emotional, psychological, and social challenges for children and also for their families as they cope with taking care of the sick child and coming to terms with their own feelings like sadness, helplessness, and anxiety. Children in adolescent age group have various issues. Assessment of these issues helps in providing ‘quality care’ to these children and their caregivers.
Objectives: To evaluate the needs and concerns of adolescent children and caregivers to provide quality care.
Methods: The focus group discussions and interviews are held with the caregivers and children with different life limiting conditions to evaluate their concerns and needs. The voices of the participants are documented and a plan of ‘Quality Care’ is decided in collaboration with a multidisciplinary team to provide need-based services.
Results: The focus group discussions with the children and their caregivers have been helpful in building rapport and that has helped to assess the behavior, needs, and concerns of adolescent children.
Conclusions: Adolescent children have varied needs ranging from information about the disease to sexuality. The needs differ as per the disease trajectory. Need assessment help the team to plan the ‘quality care’. Different models of care may be necessary for different needs.
GAPS IN DOCTORS’ PERCEPTIONS REGARDING VARIOUS ASPECTS OF CARE FOR FALLS IN THE ELDERLY
Ravi Prasad P Varma
E-mail: dr.rpvarma@gmail.com
Introduction: Falls among the elderly and resultant injuries can affect quality of life, chronic pain, or loss of independence; and eventually alter the course of all aspects of aging.
Objective: To study the perceptions of care providers regarding various aspects of palliative care requirement as a result of falls and compare those with patients’ perceptions and experiences.
Methods: The study was based on findings of formative investigation of a doctoral research on falls in the elderly. The findings of in depth interviews with 10 doctors of Orthopedics, Neurosurgery, and Surgery department and seven patients (four men and three women). One focus group discussion (FGD) with six elderly men in the community was also conducted. Interview and discussion transcripts were reviewed for identifying perceptions on various aspects of care requirement as a result of falls.
Results: Doctors identified physical aspects of elderly patients who had sustained falls in detail ranging from common presentations, complications, and death as an outcome. Mention of psychological and social aspects were limited to “degree of motivation”, “social support”, “psychological problems”, and “element of depression”. Patients’ responses ranged from concerns of treatment costs, being bedridden, having difficulties in daily activities, and needing support from others. Most patients and participants of FGD attributed falls and consequences to fate and one responded that it was “all over” due to the fall.
Conclusion: Doctors’ perceptions are largely limited to physical aspects of falls in the elderly and their consequences. Spiritual aspects were the most neglected in doctors’ responses.
COMPARATIVE STUDY BETWEEN TRAMADOL AND DEXAMETHASONE AS AN ADJUNCTIVE TO ROPIVACAINE IN SUPRACLAVICULAR BRACHIAL PLEXUS BLOCK
Alok Kumar Panigrahy, Bimal Krushna Panda, Laxmidhar Dash
E-mail: alokpanigrahy86@gmail.com
Aim: This is a prospective, randomized, double-blind study to evaluate the postoperative analgesia following supraclavicular brachial plexus block with tramadol or dexamethasone as an admixture to ropivacaine (0.5%) in upper extremity surgeries.
Materials and Methods: Total 60 patients of American Society of Anesthesiologists (ASA) I and II aged between 18 and 65 years undergoing upper extremity surgery under brachial plexus block with ropivacaine were randomly divided into two groups. One group received tramadol (1 mg/kg body weight) and the other group received dexamethasone (4 mg) as an adjunctive to ropivacaine (0.5%). The duration of postoperative analgesia was recorded in both groups using pain visual analog score (VAS) score which was determined by maximum VAS score of 8–10 and when patients demand for additional analgesics.
Results: The mean duration of postoperative analgesia in the dexamethasone group was 540 min, while in the tramadol group it was 370 min.
Conclusion: We conclude that dexamethasone with local anesthetics prolongs postoperative analgesia significantly than tramadol (P < 0.05) when used as an adjunctive to local anesthetic in brachial plexus block in upper extremity surgery.
COMPARATIVE STUDY OF INTRAVENOUS TRAMADOL VS NALBUPHINE FOR POSTOPERATIVE ANALGESIA OF LOWER ABDOMINAL SURGERIES UNDER SPINAL ANESTHESIA
Sanjay Ku Roy, Patel PK
E-mail: dr_roysanjay@yahoo.com
Introduction : Tramadol is a weak opioid μ agonist and weaker at delta and κ receptor. Nalbuphine is an opioid with antagonism at μ and agonism at κ receptor.
Aim and Objectives: The aim of this study was to compare the analgesic efficacy, sedation, and side effects of these two drugs.
Methods: Fifty patients undergoing lower abdominal surgeries under subarachnoid block were randomized into two equal groups of 25 each. They received either intravenous (IV) tramadol 1 mg/kg or IV nalbuphine 0.1 mg/kg when VAS score is 2. Half the dosage of same analgesic was repeated for breakthrough pain. Pain and sedation assessment done at 30 min, 3 h, and 6 h after each dose of the study drugs. Adverse effects and time of its occurrence was noted. Vital parameters were monitored 4 hourly for 24 h.
Observation/Results: VAS was low for nalbuphine compared to tramadol at 30 and 540 min (P < 0.05). Out of 240 observations of VCS in tramadol ‘no pain’ was 37 in number in contrast to 60 out of 250 in nalbuphine (P < 0.05). Sixty-five percent of observations in nalbuphine group were in three levels of sedation (mild-30%, moderate-22%, and asleep-13%) compared to tramadol group where 64% of observation were awake (P =0.0001). Requirement of additional dose was similar in both groups (P =0.93). Adverse effects: Four patients complained nausea and eight patients vomited in tramadol group, in comparison, two patients complained nausea and one vomited in nalbuphine group. Vital parameters were stable and comparable in both groups.
Conclusion : Nalbuphine at the dose of 0.1 mg/kg IV had marginally superior analgesic action than tramadol 1 mg/kg IV. Incidence of nausea and vomiting was seen more in tramadol. Nalbuphine had more sedative action which is beneficial in stressful postoperative period and it can be used for postoperative analgesia in patients undergoing abdominal surgeries.
A STRUCTURED PALLIATIVE CARE TRAINING PROGRAM FOR ASHA
Geetha M, Ligesh KT, Remya P
E-mail: nio.palliative.india@gmail.com
Background: Though ASHA is seen as a key group for the effective delivery of many healthcare packages at grassroots level there is a lack of clarity regarding their roles and knowledge, skills, and attitudes needed in many areas of healthcare. The potential for ASHA to intervene in health problems effectively can be realized only if certain aspects of ASHA program including capacity building are modified as per the requirement of the state. National Rural Health Mission Kerala has started a new course in Palliative Care for ASHA.
Aim of the Course: The 1-month course aims to train ASHA to handle community level monitoring and supportive care activities for the chronically ill, incurably ill, bedridden, and dying patients. This “Basic Course in Community Based Interventions in Palliative Care and Long Term Care”, is a structured 1-month course.
Course Structure:
One week of theory
Three weeks of practical hands on training and
a final evaluation
Topic covered includes:
Assessment of patients
Nursing procedure
Result: A total of 137 Asha workers have successfully completed training in 2012–2013. They are now involved in the delivery of palliative care in community. They were trained through 14 centers in Kerala and the program was monitored by Pain and Palliative Care Society, Calicut. Feedback was collected from ASHA workers who have successfully completed the training and the program was found useful and effective to train ASHA in palliative care.
Conclusion: “Basic Course in Community Based Interventions in Palliative Care and Long Term Care” is an effective training program to train ASHA in palliative care.
INTEGRATING ULTRASONOGRAPHY TO PALLIATIVE CARE ONCOLOGY CONSULTATION - CACHAR CANCER HOSPITAL AND RESEARCH CENTRE, SILCHAR, INDIA EXPERIENCE
Iqbal HM Bahar, Folaju O Oyebola
E-mail: iqbal.bahar@cacharcancerhospital.org
Introduction: Palliative care consultation besides pain and symptom control involves impeccable assessment for accurate diagnosis and prognostication of life limiting disease conditions. History taking and physical examination during clinic consultations may not be adequate and often times there are need for further investigations. Ultrasonography (USG) is a very common and a reliable tool for patient evaluation, but often requires booking and scheduling appointments with long delays in developing countries. Palliative care clinic of Cachar Cancer Hospital, has USG facility. This integration is a very rare opportunity. The palliative care physician is versatile in following-up the patients by evaluating; prognosticating and also offer needed interventions.
Methodology: A retrospective study of all patients’ consultations at the palliative care clinic and admissions over a 4-week period May–June 2013 were evaluated.
Results and Data: There were more males (54.9%) than females (45.10%). Three commonest oncological conditions were lung (27.4%), gallbladder (19.4%), and breast cancers (10.1%). Not all the patients presented at the palliative clinic needed USG evaluation (61.1%), but the usual pain and symptom control. However, 38.9% of the patients had the USG in their follow-up either for prognostication or interventional issues. Majority of the USG active intervention were for fine needle aspiration cytology (FNAC) or biopsy (93.75%).USG-guided therapeutic procedures were abdominal paracentesis (54%), intercostal drainage (35%), thoracotomy for pneumothorax (7%), celiac plexus block (3%), superior hypogastric block (1%).
Conclusion: In a limited manpower and resource poor settings, the responsibility of a palliative care physician may go beyond symptom control. Possession and integration of interventional USG skills and knowledge into palliative care consultation could be an invaluable asset.
PRACTICES OF USING NARCOTICS IN INPATIENT AREA AT TERTIARY CANCER HOSPITAL
Shweta J Ghag
E-mail: ghagshweta@yahoo.co.in
Healthcare safety is a thought provoking and a challenging global issue both for developed and developing countries. “First, do no harm” has always been the pillar of medicine. However, unintentional harm does occur at all levels of the health system. A well-established narcotics system is means of monitoring and improving the quality of care and services safer and more effective when continuously monitored and systematically reviewed to improve standards.
Tata Memorial Hospital is pioneer in safe handling of narcotics in India. Approximately, 250 new cases of palliative patients are registered and 42 admissions are registered every month. Inhouse system is developed to standardize procedures and protocols for dispensing and administering medication in safe and effective manner. All narcotic medications are stored in narcotic vault at ward level, the key of which is maintained with sister in-charge. Narcotic medications for external use should be stored in a separate container in the narcotic cupboard. All narcotic medications should be checked carefully for the expiry date. Narcotic medication is prescribed in the official doctor's order sheet. Clinician informs nurses on duty. Nurse on duty administer the narcotic medicine from stock and preserves the broken ampules, documentation is done in the narcotic register and patients file. Replacement is done, from dispensary by the senior nurse on duty from pharmacy. Staff education on drug handling and medication errors was done on regular basis. No incidence of misuse of narcotics either by healthcare workers or patients are seen because of awareness regarding the regulatory norms and procedures.
References Internal resource document if any: Nursing Manual, Pharmacy Manual, External resource document if any: The D and C act, 1940, and Rules 1945.
Web based references: Directorate of Nursing Affair – Drug Administration: Policy and Procedure on Narcotics.
FIVE YEARS OF NATIONAL RURAL HEALTH MISSION PROJECT IN PALLIATIVE CARE IN KERALA
Sanoj AK, Biju PC, Suresh Kumar
E-mail: nio.palliative.india@gmail.com
Statement of the Problem: The total number of people in need of palliative care in India can be estimated to be 60% of all deaths, or 5.4 million people a year. A study on ‘quality of death’ carried out by Economist Intelligence Unit of “The Economist” in 2010 covering 40 countries, ranks India the last, even below Mexico, Brazil, Uganda, etc. The estimated average coverage of palliative care services in the whole of the country is less than 2%. The south Indian state of Kerala is estimated to have more than 125,000 incurably ill, bedridden, and dying patients in need of palliative care.
Description of the Project: National Rural Health Mission (NRHM) Palliative Care Project was initiated in 2008 with the aim of facilitation of development of a public health model in palliative care in Kerala in line with the Pain and Palliative Care policy of Government of Kerala. The policy had happened in the background of widespread civil society involvement in palliative care in the state. The project aimed to establish the primary, secondary and tertiary care facilities for all the bedridden incurably ill and dying patients in Kerala with community participation. The strategy was to facilitate the development of palliative care programs through Local Self Government Institutions, while taking care to maintain the spirit of community participation in the program. Focus of the program was on sensitization and capacity building among various strata of the society and also healthcare professionals at the primary, secondary, and tertiary level healthcare system. Since NRHM projects are for 1 year, the whole program was divided to ‘standalone’ annual projects and each year's project has been getting submitted to NRHM. Institute of Palliative Medicine, World Health Organization (WHO) Collaborating Center for Community Participation in Palliative Care and Long Term Care has been entrusted with the task of preparation of yearly projects with the overall project in mind.
Impact of the Project: In a project of this kind which essentially reduces physical and mental suffering, which induces a sense of belonging among the terminally ill, the impact in the community is more than what can be quantified by measurable indicators. The effective network of palliative care services extending in more than 850 of the local governments along with 150 palliative care units from the non-government sector covering more than 60% of the needy has given a different quality of life to beneficiaries and their families. Kerala, with 3% of the national population now has more than 90% of palliative care units in the country. The project also provided a common platform for likeminded compassionate individuals and various organizations to effectively orient their complete potential for the well-being of the society.
Scalability: An innovative project by NRHM acted as the facilitator for local government to establish palliative care projects in Kerala. Since the model works through existing institutions and processes within the public system, it is easily replicable. The processes, procedures, and systems can be explained in detail to provide an adaptable model to any agency or government. The experience in Kerala has been that once the scale of the problem is brought out into the open, social, and political support is almost naturally assured. The universal nature of the problem of incurable illness, debility, dying, and death makes sensitization and advocacy easier than other health issues.
Conclusion: Palliative care services are poorly developed in India, the second most populous country in the World. NRHM has facilitated the development of a unique public health model in Kerala which can be replicated in other states of the country.
FEAR OF DEATH
Sinimol KV Auxillary, Lissy Rajan
E-mail: nio.palliative.india@gmail.com
Introduction: Death is the ultimate reality of human life. It is a truth from which no one can escape. The response to the idea of one's death depends on a large number of factors and it varies across cultures and age groups. But one of the most common emotion related to his or her death is that of fear. The fear of death is something each palliative care worker would have seen sometime during their experience with the patients. It would be an interesting venture to enquire regarding the influence of such an experience on the thoughts about and emotional response to their death.
Aim: To assess issues related to fear of death among the palliative care workers.
Materials and Methods: A total of 250 palliative care workers will be assessed using the Lester Fear of Death Scale version 3.0 which is translated to native language.
Results: This is an ongoing study. The results will be analyzed and reported after completion of the study.
A WORLDVIEW OF PALLIATIVE CARE
Stuart Malloy
E-mail: mailto: pcfp@mac.com
The world consists of people of varying cultures with varying views of how life is to be lived and what constitutes a good life. What is the basis for those views? Are they socioeconomic, spiritual, or health-related?
What about death? Does a good life always precede a good death? What does a good death look like?
What kind of conversations should be a part of a culture that desires to care for their sick and dying in a way that allows the patient and loved ones to be involved in what they would like their end-of-life care to consist of?
I have been involved in end-of-life care for 40 years and directly involved with hospice/palliative care full-time for 7 years. I have been a part of care in Mexico and Haiti along with the United States. There is a better way to help with the sick and dying of our world.
Our presentation is about the need for end of care and end-of-life conversations for everyone, but more specifically, to the sick and dying. It is a reminder that end-of-life care consists of more than just miracle cures and treatments, but assisting the sick to face their mortality supported by family and medical community. We hope to create open dialogue and active responses to the need for alternative ways to care for our terminally ill patients.
A trained hospice/palliative care team is equipped to do the same what we can do at home.
TRIAGE SYSTEM IN HOME CARE
Sunil Dhiliwal, Supriya Salunkhe
E-mail: Supriyasalunkhe06@gmail.com
Introduction: Patients with advanced cancer experience multiple areas of suffering which interact to create a complex need of help. Specialist palliative care services have been developed to meet these needs. There is a dearth of literature in palliative care, on the amount of time people wait for palliative care treatment, and the management of patient's. There is limited information regarding the prioritization of patients, importance of uncontrolled symptoms, psychological distress, prognosis, and the management of competing needs. Based on this, a triage system was devised as a pilot study to provide a basis for decision-making to prioritize patient as per their needs and provide timely intervention.
Objectives: The objective of the current study was to understand if the triage system has helped to provide timely intervention to the patient and thus reduce their sufferings and unnecessary hospital admissions.
Methods: Homecare services will be coded as:
High priority 01 (urgent visit) - Home visit in 0−3 working days.
Medium priority 02 - Home visit in 0−10 working days
Low priority 03 - Home visit in 0−18 working days
The duration of home visit was decided based on our previous experience with triaging home care services.
Results: A total of 1,830 visits were done in 2012 based on the triage code. As per the triage criteria, 32 patients were categorized into ‘high priority’ code, 126 into ‘medium priority’, and 1,693 into ‘low priority’ code.
Conclusion: We pilot tested the triage coding system in this study based on which future studies could be directed towards standardized tools for triaging patients. Our results suggest that the triage coding system can help to direct resources to patients who are most likely to benefit from them, and help to decrease the demands on limited resources, thereby making available more resources towards ‘high to medium priority’ patients.
RELIABILITY OF THE CORK UNIVERSITY HOSPITAL GROUP ORAL CAVITY ASSESSMENT TOOL IN AN INDIAN PALLIATIVE CARE SETTING
Sreedevi Warrier, Rajagopal MR
E-mail: dr.sreewarrier@gmail.com
Introduction: Assessment and recording of oral hygiene is an important but incompletely addressed element of palliative care.
Objective: To evaluate oral cavity assessment tool of Cork University working group, Ireland for assessment of oral hygiene status of persons seeking palliative care from Pallium India, Kerala.
Methods: Oral hygiene status of 64 persons seeking care at various link centers of Pallium India was assessed by physical examination and recorded using the 17-item oral cavity assessment tool. The tool underwent assessment of face validity and internal consistency. Principal component analysis (PCA) was undertaken to identify possible components (small sets of variables that contain most of the information in the large set).
Results: The distribution of males and females was equal. There were 18 persons with cancer of oral cavity/adnexa, 32 with cancer of other sites, and 14 with non-cancer conditions. None had teeth that were free of debris, 26 (40.6%) persons reported mouth pain of varying severity, and 16 (25%) persons had severe manifestations indicative of poor oral hygiene. The tool had moderate internal consistency (Cronbach's alpha 0.75), but poor additivity (analysis of variance (ANOVA) with Tukey's test for non-additivity, P < 0.001). Only one component comprising of four variables–lips, gingiva, mucous membrane, and mouth pain–could be extracted in PCA.
Conclusion: Manifestations of poor oral hygiene were very common, but the scale had limited reliability for scoring this in our set up. The individual items of the scale may however be used to document oral hygiene status in clinical records.
IMPOSSIBLE IS NOTHING
Viv James
E-mail: tim.viv.james@xtra.co.nz
The Opening Doors Program (ODP)-An Innovative Day Hospice Program.
The basic principle of a Hospice is to cater for the needs of patients at all levels of living and to optimize their quality of life. The ODP, (ODP), running at Mercy Hospice Auckland (MHA) has made a significant difference to palliative care patients, improving both their sense of worth and their quality of life.
At Mercy Hospice we have over 290 patients on our books. We are situated in Ponsonby, central Auckland, where we have a 13 bed inpatient unit, and the facility to run a day program for patients living in the community.
Patients have the opportunity to enjoy a relaxed atmosphere, meet new people in beautiful surrounds, and have a range of complementary therapies available to them. Volunteers are relied on for all aspects of the program, providing the many therapies available to patients including hairdressing, nail and foot therapy, massage, music, and art. The introduction of a Ukulele group has been hugely successful, creating a sense of belonging and of community, with staff, volunteers, and patients alike all taking part and enjoying the ambiance. This combination of factors enables patients to look beyond the confines of their illness and as Andrew Moore stated,[1] it frequently leads to a search for deeper meaning and an addressing of spiritual issues.
At OD, it became apparent that patients had an overwhelming desire to share their lives and their profound concerns about their dying. The team at OD endeavored to cater for this “ELEPHANT IN THE ROOM”. What has developed over time, is the Self Care and Education Program. In a safe environment, where confidentiality and respect are paramount, skilled facilitators tackle the tough issues of; death and dying, grief and loss, advanced care planning, and most importantly how patients might approach their families to talk about their impending death. The response has been very significant and has led to a formal evaluation of the relevancies and benefits of this program. Patients were interviewed and recorded and a survey was formulated. Thirty patients took part in the survey and the findings were;
-
100% of the patients, completing the survey, were comfortable with the program
-
Patients made suggestions of how to enhance and improve the program
-
Patients felt valued and respected having been a part of the evaluation process
-
All of patients surveyed, found it helpful to share how they felt in a group, with others, who were in similar circumstances.
Denis, one of the patients who took part in the survey commented:
“The connection with others in similar circumstances makes you feel you are not alone. People here understand and don’t want to fix it, they just accept you as you are. We understand each other and connect at a deeper level.”
The ODP is essentially in harmony with the MHA philosophy, LIVING EVERY MOMENT. This is portrayed especially well in two other significant elements in the make-up of the program. The first is a very big event staged each year at Hampton Downs Raceway, called Race for Life. This extraordinary event has been running for 6 years now. The most outstanding feature might be almost looked upon as a mathematical formula:
COMMUNITY + PATIENTS = WIN/WIN
Dame Cecily Saunders (1978)[2] stated:
“Hospice is indeed a place of meeting, physical and spiritual, doing and accepting, giving and receiving, all have to be brought together. The dying need the community, its help and fellowship. The community needs the dying, to think about eternal issues and to make it listen”. How true!!
It is both stirring and heart-warming when 50 patients merge on the facility at Hampton Downs Raceway to be given a choice to ride in racing cars, a helicopter, trucks, luxury cars, and on a Harley Davidson Motorbike. All is provided freely by the local community who have remained faithful to this event since its inception. A committee of dedicated enthusiasts work on the organization of the day for months prior. Volunteers on the day offer all services to patients for free. They find the day astounding, and then ask if they can return the following year!! Needless to say the patients have the time of their lives!!
The second of the two significant elements of the ODP is the wish list. This provides the avenue by which patients are encouraged to live every moment. As with Race for Life, it is an honor to be privy to the generosity of our community. The OD team is in awe of the kindness, generosity, and heart-warming hospitality of so many businesses, big or small, throughout New Zealand. People want to help out and make a difference, knowing that they themselves could well be among the patients in the future.
As a facilitator, it is crucial, not to be a gatekeeper. Tenacity is an indispensable characteristic as is the ability to tell a good story that will reach the hearts of the community. The sky is the limit. Impossible is nothing!! Mix all that with an intrinsic belief and faith in humanity and you have a wonderful recipe for success.
Conclusion: The ODP is making a huge difference to the quality of lives of our patients. To achieve this excellence, such a program needs to be driven by passion, a passion shared by the Hospice Trust Board and shown by their endorsement of paid positions. To maintain a team of dedicated, dynamic, and committed personnel; staff need to feel valued. MHA have witnessed many magical moments, by investing in a program that meets the needs of its patients and optimizes their quality of life.
DEVELOPMENT OF PRO FORMA TO ASSESS “TOTAL CANCER PAIN”
Anchal Satija, Sushma Bhatnagar
E-mail: anchal.satija@gmail.com
Introduction: The multidimensional nature of cancer pain has been accurately described by Dame Cicely Saunders as ‘total pain’; which comprises of not just the physical component but emotional, psychosocial, and spiritual components also. There is growing awareness amongst professionals to treat ‘total cancer pain’. In order to address this need, this study was conducted to develop a pro forma to assess all components of cancer pain.
Objectives: To develop a pro forma to assess all components of cancer pain, that is, physical, emotional, psychosocial, and spiritual.
Methods: This was a prospective study conducted at Pain and Palliative care Unit of Department of Anesthesiology, Dr BRA Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi. The information regarding demographic, socioeconomic, psychological, and spiritual profile was noted. The patients’ physical pain was treated according to WHO analgesic ladder and interventional pain management and other components influencing the cancer pain were identified and treated accordingly.
Results: Results from 48 patients were obtained. The data from the patients showed the occurrence of psychosocial and spiritual issues among the cancer patients. The patients seemed to be burdened by not only the physical aspects of disease, but were simultaneously affected with above mentioned concerns.
Conclusion: Cancer pain is multidimensional. The psychosocial and spiritual components add to patients concerns regarding the disease. Hence, for effective management of cancer pain, all the components of cancer pain need to be addressed. However, small sample size is a limitation of this study. It is recommended to perform the study on a larger population and validate the pro forma.
THE FEASIBILITY OF USING GOAL ATTAINMENT SCALING ON AN ACUTE ONCOLOGY WARD IN PATIENTS WITH ADVANCED METASTATIC DISEASE
Nimisha Panchmatia
E-mail: nimisha.panchmatia@imperial.nhs.uk
Background: Goal setting is the central part of the interdisciplinary rehabilitation process and is a cornerstone for therapies. Holistic, patient-centered goal setting is noted to yield effective rehabilitation outcomes resulting in goal attainment, patient satisfaction, and shorter length of hospital stay. The practice guidelines emphasize patient involvement in goal setting which appears to happen in rehabilitation settings and seems to be elusive in acute care.
In an acute care setting, the focus is on medical treatment and rapid discharge. Therefore, therapy intervention and goal setting methods often lack a patient-centered approach.
Aim: To assess the feasibility of using the Goal Attainment Scaling (GAS) on acute oncology wards with patients diagnosed with advanced metastatic disease and explore patients’ experience of participation in the process.
Study Design: Feasibility study.
Setting and Participants: Inpatients on acute oncology wards referred to Occupational Therapy (OT) services between February and April 2012, were assessed for study inclusion. Out of 100 referrals, 26 were eligible and 12 recruited. Goal setting and the outcome and patient experience were documented via GAS-light (GAS-l) and Patient Opinion Survey, respectively.
Results: Pre- and postintervention GAS-l scores demonstrated a clinically significant change (mean change 12.77, ± standard deviation (SD) 9.03; with respect to a composite GAS-T score of 50). The goal setting process was perceived to be beneficial and satisfactory.
Conclusion: The GAS-l was a useful outcome measure for few selected patients of this population, that is, patients’ with rehabilitation potential. In addition it helps to define ongoing (community) rehabilitation requirements.
STARTING PALLIATIVE CARE SERVICES - AN EVIDENCE-BASED APPROACH
Savita Butola
E-mail: savitabutola@yahoo.com
Introduction: A public health strategy offers the best approach for translating new knowledge and skills into evidence-based, cost-effective interventions.
Objectives: Evidence-based establishment of palliative care services in the Border Security Force (BSF).
Methods: A preliminary study showed that 75% BSF doctors were unaware of the concept and scope of palliative care. A presentation at the annual training conference led to the policy decision that palliative care should be a part of the regular medicare. Data was collected from all BSF units to assess the number and profile of patients. An awareness campaign was started and a series of presentations held at Kolkata; Delhi; Siliguri; Jalandhar; Bangalore; the training academy (Gwalior), for doctors undergoing basic as well as senior training courses, annual medical conference; the BSF schools; women's welfare centers; and at the Headquarter of Narcotics Control Bureau aimed at not only healthcare workers but personnel of all ranks. The second phase of the campaign is planned for Srinagar, Jodhpur, Ahmedabad, Agartala, Shillong, and Aizawl. Training for staff was organized; study material mailed, peer support group started, advocacy/independent ethics committee (IEC) activities included articles in the mainstream and vernacular media, BSF magazines, and e-hospice. ‘Pahal’ (NGO) helped in awareness campaign targeting the youth, citizens, and local hospitals at Jalandhar.
Results: In-hospital services were successfully started at Delhi in 2010 (’Cansupport’ provided counseling/homecare) and Jalandhar in 2012.
Conclusions: Evidence-based practice (EBP) helps put research results into practice and when used for groups, can help develop an organization.
EFFECT OF TASK-ORIENTED TRAINING ON GAIT PERFORMANCE IN MCA STROKE PATIENTS
Sakthi K. B. Prasad
E-mail: sakthiprasad03@gmail.com
Stroke is the major cause of chronic disability and the largest consumer of rehabilitation services in the elderly. The ability to perform the basic activities of daily living is reduced initially in three out of four patients in stroke. The activity most affected is walking/gait with as many as 80% of patients initially losing the ability, and walking impairments are present in more than half of the patients who survive the acute phase.
Task oriented training is a form of exercise training in which gait and gait related activities are practiced using a functional approach. It is a form of exercise, where movement emerges as an interaction between many systems in the brain and is organized around a goal and constrained by the environment.
Objective: To investigate the effect of task-oriented training to improve the gait performance in middle cerebral artery (MCA) territory stroke patients, Brunnstrom stages 4 and 5.
Design: Experimental study.
Setting: Alpha Palliative Care Hospital. Subjects: Thirty patients with MCA territory stroke were recruited at 3 month after stroke onset.
Interventions: The participants were divided into two groups, group A (n = 15) and group B, (n = 15). The group A received conventional physiotherapy, while the group B received task-oriented training along with the conventional physiotherapy. Treatment was given for 6 weeks.
Outcome measures: Walking distance assessed with 6-min walk test and gait speed assessed with 10-m walk test.
Result: Significant improvements in all main outcomes parameters were observed in response to the intervention. Between group analysis showed a statistically significant difference in favor of task oriented training in performance of the 10-m walk test (t =5.555, P = 0.005) and the 6-min walk test (t =3.642, P 0.002).
Conclusion: The task-oriented training seemed to be beneficial in improving gait performance in MCA territory stroke patients.
PERSPECTIVES OF ORTHOPEDICIANS ON PAIN MANAGEMENT IN OSTEOARTHRITIS - A QUALITATIVE STUDY
Austine J, Nair S
E-mail: drjosebabu@gmail.com
Introduction: Osteoarthritis (OA) is the result of a degenerative process and is the most common form of arthritis and one of the leading causes of pain and disability worldwide, which in turn significantly impair the quality of life in patients. It would therefore be imperative to know the treating doctor's perception about pain relief in this group of patients.
Objective: To assess orthopedician's perspectives on pain management in osteoarthritis pain.
Methodology: In this qualitative study, a semistructured interview was conducted on 15 orthopedic surgeons from a tertiary care hospital and audio recorded simultaneously. The audio recording was transcribed verbatim and a grounded theory approach was used to code the data. An inductive approach using thematic analysis was used to manually analyze the data.
Results: Five themes emerged. (1) Participants said that osteoarthritis produces significant disease burden and impaired quality of life in patients. (2) Pain management usually comprised of a multipronged method of treatment with more emphasis on physiotherapy and surgery and less on analgesics. The doctors felt that patients usually demand immediate pain relief. (3) Doctors usually preferred a practice of individual discretion as against any guideline or protocol; however, a few felt that there was a need to systematize pain management. (4) The participants all agreed that counseling would help in the improvement of the quality of life of patients. (5) All participants put forward several barriers for optimal pain management.
Conclusions: There is a need for a patient-centered approach to pain management in osteoarthritis. Comprehensive osteoarthritis pain management involving a multidisciplinary team will help in providing better pain relief and in turn improve the quality of life in osteoarthritis patients. There is also a need to correlate the doctor's perspectives with those of the patient.
EFFECTIVENESS OF REFLEXOLOGY IN REDUCING CHRONIC PAIN AMONG PATIENTS WHO RECEIVE PALLIATIVE CARE
Anu Savio Thelly
E-mail: anu.savio@gmail.com
As a form of complementary and alternative medicine (CAM), reflexology has gained popularity in the treatment of various conditions, including those relating to pain. A small scientific study on reflexology as a treatment for pain finds that it may be as effective as painkillers. Reflexology is a complementary medical approach, which works alongside orthodox medicine, in which pressure may be applied to any body area, but is commonly used on either the feet or hands.
The sample consists of 40 patients with cancer, between the age group of 30–60 years with receiving palliative care were allocated to either reflexology (n = 20) or routine nursing care only (n = 20). The treatment group received 20 min of reflexology twice a day for 3 days. Pain was recorded before and 5 min after the intervention by using numerical pain intensity scale. Paired t-test was used to assess the effect of music on pain both the group. In the music group, t-value is significantly higher than the tabulated value at 5%, z-test was used to assess the difference between experimental and control group, this shows significantly higher than the tabulated value at 5%. Reflexology is a beneficial nursing intervention that promotes relaxation and alleviates the perception of pain among the patients. Reflexology could be used as an intervention along with other modalities of pain management as it has no adverse effect.
EFFECTIVENESS OF EPEC-6 STEP PROTOCOL ON COPING AFTER BREAKING THE BAD NEWS AMONG PATIENTS WITH LIFE LIMITING ILLNESS
Sivaprakash S, Ilangovan G
E-mail: siivaprakash@gmail.com
Introduction: No one likes breaking bad news. Although doctors and other professionals have always broken bad news, the increase in chronic illness and the issues related to quality of life, heighten the importance of understanding how the delivery of bad news affects patients and their family.
Objectives: To assess coping among patients who already knew their prognosis. To assess coping among patients for whom Education for Physicians on End-of-life Care (EPEC)-6 step protocol was used for breaking the bad news. Study design: Sixty patients of which 30 already known about the prognosis and 30 patients to whom the researcher conveyed the bad news with selected intervention. COPE Inventory was used to assess the coping.
Results: Patients who already knew the prognosis conveyed that a direct approach was most common, without much prior warning for the patients. EPEC-6 step protocol includes: Getting started, what does the patient know? How much does the patient want to know? Sharing the information, responding to patients’ family feelings, and planning and follow-up. Descriptive and inferential statistics was used for the analysis. Results suggested that patients had a better coping with EPEC-6 step protocol. This approach was perceived as appropriate and sensitive.
Conclusions: Bad news is not always broken in a sensitive way, despite considerable efforts to address this issue. Relatively minor changes to practice could improve the patient experience: Greater preparation, provision of sufficient time in consultations, and cautious disclosure for new patients.
“STUDENTS FOR PALLIATIVE CARE - A PILOT PROJECT”: AN INITIATIVE OF ALPHA PALLIATIVE CARE
Neeraja Keeran, Rashida Abdulla, Rekha Rajeev
E-mail: neeraja.keeran@alphapalliativecare.org
Introduction: Lack of proper awareness and support from the public is one of the major challenges in delivering adequate palliative care services for the needy. Alpha Palliative Care believes that involvement of students in palliative care can be a solution for the problem.
Objectives: To sensitize and develop social responsibility among the students in palliative care.
-
To empower the students with knowledge and skill in palliative care.
Methods: The methods used in the study are qualitative and quantitative approaches.
Results: Other programs initiated by the students under students’ initiative for palliative care [Table 1].
-
Walkathon and a seminar in connection with World Hospice and Palliative Care Day.
-
Voluntary activities for palliative care activities: Mime presentation, resource mobilization, home care, designing of patient's need-based wheelchair.
Publication of newsletters3.
Conclusion: “Students for Palliative Care” is an experimental initiative of Alpha Palliative Care to ensure the delivery of palliative care services through the students. Such initiatives resulted in more patient registrations and other support (like fund raising and participation in other palliative care programs) building measures among the community for the cause of palliative care. Thus, Alpha Palliative Care envisages a new generation of civil society committed to deliver total palliative care, sensitized and supported by the students’ power.
SOCIAL NEEDS ASSESSMENT AND INTERVENTIONS IN A TERTIARY PALLIATIVE CARE CENTER
Shyni M, Likesh
E-mail: nio.palliative.india@gmail.com
Introduction: Palliative care offers whole person care for patients with chronic and incurable conditions. This includes physical, psychological, spiritual, and social care. There is limited data on characterization of the social interventions offered in palliative care locally. This study was undertaken to determine the range of social interventions offered and implementation of social needs assessment and interventions in routine clinical practice.
Method: The study will be carried out at the Institute of Palliative Medicine, Kerala. Structured questionnaires were designed to survey the range of interventions provided at the center. The survey sample included clinical and administrative staff as well as patients. An audit pro forma was designed to determine practice of social needs assessment and interventions. Case notes were randomly sampled and audited using the pro forma to determine social needs assessment and interventions in actual practice.
Results: The range of social interventions offered will be characterized across domains of finances, food, education, housing, and employment. Audit results will demonstrate and benchmark current practice of social needs assessment and interventions. Association between disease status (cancer vs non-cancer) and sociodemographic variables and social needs assessment and intervention will be analyzed using chi-square tests.
Conclusion: Recommendations will be made for continuing quality improvement of social domain in palliative care.
THE USE OF ANTIDIABETIC, ANTIHYPERTENSIVE, AND LIPID-LOWERING MEDICATIONS IN THE ELDERLY DYING WITH ADVANCED CANCER
Al-Shahri M, Sroor M, Ghareeb W, Aboulela E, Edesa W
E-mail: malshahri@kfshrc.edu.sa
Introduction: The prescription of medications unrelated to symptom control may be difficult to justify in terminally ill cancer patients, especially in the dying phase.
Objectives: To determine the prevalence of prescribing antidiabetic, antihypertensive, and lipid-lowering medications to elderly patients dying with cancer.
Methods: We reviewed the medical records of patients above 60 years of age who died with cancer at our palliative care unit, over a period of 23 months. The collected data included the use of antidiabetic, antihypertensive, and lipid-lowering medications during the last week of life.
Results: Of the 103 patients included, 51.5% were females and the median age was 69 years. The most common cancer categories included gastrointestinal (40.8%), gynecological (13.6%), and head and neck (12.6%). All patients had either metastatic (92.2%) or locally extensive (7.8%) disease. Hypertension (59.2%), diabetes mellitus (52.4%), and dyslipidemia (19.4%) were common. During the last week of life, 38.8% of patients received antidiabetic, 23.3% received antihypertensive, and 3.9% received lipid-lowering drugs. More than one half of patients (51.5%) had received at least one of the medications under study. No association could be detected between patients’ characteristics and the prescription patterns.
Conclusion: This study has shown that a significant proportion of old patients dying with cancer are maintained on medications for chronic conditions until the very late stages of their lives. For these frail and actively dying patients, the benefits of such medications are unlikely and the various drug-related burdens are possible. Further research is needed to explore physicians’ perceived rationale of such practice.
QUALITY OF LIFE IN TERMINALLY ILL CANCER PATIENTS RECEIVING HOME-BASED PALLIATIVE CARE UNDER PRPCS
Anuradha S, Kamalakar V, Vidya K, Palat G
E-mail: vujjinikamal@gmail.com
Aim: A study on the symptom management, physical and psychological health, perceived control of the effects of cancer, and quality of life of terminally ill cancer patients receiving home-based palliative care, and the factors that predict quality of life.
Introduction: Quality of life is a major goal in the care of patients with terminal cancer. In addition to symptom management, psychological care and provision of support, being cared for at home is considered an important determinant of patient well-being. A more comprehensive understanding of the impact of cancer on patients and their families will inform the delivery of palliative care services.
Methods: Twenty-five patients with terminal cancer from MNJ Institute of Oncology and Regional Cancer Centre (MNJIO and RCC) were recruited for home-based palliative care of Pain Relief and Palliative Care Society (PRPCS). A structured questionnaire was administered by personal interviews to obtain quality of life details.
Results: The most prevalent symptoms usually seen are pain, sleep disturbance, weakness, fatigue, and constipation. Patients receiving home-based services had significantly less symptom severity and distress, lower depression scores, and better physical health and quality of life.
Conclusions: The main issues arising are the early detection and management of both physical and psychological symptoms and the need to use strategies that will empower patients to have a greater sense of control over their illness and treatment. Studies are needed to identify other factors that may impact on quality of life, and to establish the extent to which home-based palliative care meets the needs of both the patient with terminal cancer and their family.
ONCOLOGY NURSES’ KNOWLEDGE, PRACTICE, AND EDUCATION ABOUT ORAL CARE OF CANCER PATIENTS UNDERGOING CHEMOTHERAPY AND RADIATION THERAPY
Radhika R Pai, Ravikiran Ongole
E-mail: radhika.r@manipal.edu
Introduction: Oral health and oral care are crucial aspect of oncology nursing. Most of the published studies have been conducted in western and European countries, whereas there is not much literature in Indian setting related to oral care of cancer patients.
Aims: This study aimed to determine the nurses’ knowledge and practice about oral care in cancer patient undergoing chemotherapy and radiation therapy.
Materials and Methods: A cross-sectional descriptive survey was conducted among 158 staff nurses working in oncology related areas from four different hospitals of Dakshina Kannada district and Udupi district of Karnataka state, India by using purposive sampling technique.
Results: Majority (81, 51.3%) of the staff nurses had poor knowledge on oral care of cancer patients. More than half of the subjects did not perform oral care in their usual duties. Lots of writing tasks, staff shortage, and different practices were the major barriers to oral care. 80.63% (87) of the staff nurse reported that knowledge acquired through basic education in oral care is not sufficient. Documentation audit reveals that nurses recorded oral care in the chart, but oral problem assessment was not recorded at all. Most of the staff nurses did not receive basic and continuing education in oral care of cancer patients. In all four hospitals surveyed, there was no protocol specific for oral care of cancer patients
Conclusion: Nurses expressed that oral care in the cancer wards was one of the most neglected care aspect in oncology nursing. This result highlights the need to develop evidence-based oral care intervention protocol and continue education programs on oral care for improving knowledge and practice of staff nurses in order to render comprehensive care to the patients.
EVIDENCE-BASED ADVANTAGES OF HOME CARE IN PALLIATIVE THERAPY
Santosh Chaudhari, Priyadarshini Kulkarni, Vivek S Nirabhawane
E-mail: santosh.chaudhari@ciplacare.com
Introduction: Homecare is the preferred mode of care by patients, care givers, and doctors. Hitherto this was based on preference of patients and perception of doctors. We studied the outcome of our home care program to confirm the impact of our services in terms of the outcome.
Objectives: The present study was aimed at analyzing home care data to confirm the rising demands of homecare in certain patient populations.
Methods: Using our indigenous software, data specific to homecare was collected for the years 2011–2013. It was analyzed to confirm the hypothesis that the need for home care services is rising, along with demands for more frequent visits and better end-of-life management at home.
Results: Home care is preferred by a small family that has few caregivers to accompany the patient to an inpatient center. Most patients in our study had no insurance; hence, there was a need to free the earning member from caregiving responsibilities. Most patients had multiple symptoms, including pain that could be managed at home. The data shows that more patients are opting for homecare, and that this leads to more deaths in home setting. A greater number of patients are alive at the end of the year, probably due to early intervention. However, this needs confirmation.
Conclusions: The advantage of managing a terminally ill patient at home cannot be overestimated. Frequent visits, quality services, and prompt interventions can lead to a drop in hospital deaths, reducing the load on inpatient facilities.
PATIENT DATABASE IN PALLIATIVE MEDICINE - AN ATTEMPT TO ENHANCE QUALITY OF CARE
Vivek Nirabhawane, Santosh Chaudhari, Priyadarshini Kulkarni
E-mail: vrushali.anavkar@ciplacare.com
Introduction: Palliative care involves a multimodal approach including medication, nursing, counseling, and social support. In order to increase the benefits that patients may accrue, it is necessary to standardize treatments, record, and evaluate outcome measures.
Objective: Highlighting the need to maintain indigenous database in palliative care.
Methods: For enhancing palliative care services, we have used customized software. The software was used to record the demographics, disease details and treatments, palliative care rendered, symptom, and survival data.
Results: Data from a total of 9,130 admissions from 1997 to 2013 was analyzed using the software. Data was sorted on the basis of a diagnosis of breast cancer, patients who totaled 953. The mean age of patients was 54.15 (14-91). The patients survived for an average of 98.57 days after first admission at the center. Of the total 779 patient died at the center, while 139 were discharged. The most common symptom was pain suffered by 70.07% followed by breathlessness in 42% of the patients. Based on this information we could develop protocols to treat these patients.
Conclusions: It is axiomatic that whatever is not measured cannot be improved. Metrics is thus at the basics of any innovation. With the use of the software we found it easy to analyze patient data faster and more accurately. Such a database leads to quick and focused patient management. It might lay the foundation for helping in future research activities, which will help to establish evidence-based palliative service.
EFFECTIVENESS OF LAVENDER OIL IN REDUCING INSOMNIA AMONG INPATIENTS RECEIVING PALLIATIVE CARE
Grace B
E-mail: pinkybenne@gmail.com
Lavender oil, which is distilled from lavender flowers, is often used in aromatherapy and massage. Since lavender oil has no potential for drug abuse and no sedating side-effects, it appeared to be an effective and well-tolerated alternative to benzodiazepine drugs for amelioration of insomnia among hospice patients. In this study effects of aromatherapy were measured using Insomnia Severity Scale (ISS) and Pittsburg Sleep Scale (PSS). A total of 40 patients, female (25%) and male (75%) subjects, 18–65 years of age were randomized into two groups. Participants were eligible for the study if they met the inclusion criteria of a ISS and PSS-total score of greater than 18. In order for a participant to qualify as having a significant response to treatment they were required to have a reduction of at least 50% in the ISS and PSS-total score during the 6-week trial. Remission was defined as a ISS and PSS-total score of less than 10 points at the end of the 6-week study. The results demonstrated that lavender oil was comparable to the conventional approach in its ability to promote relaxation. The ISS and PSS-total score decreased by 45% in the Lavender oil group and decreased by 46% in the conventional group. At the conclusion of the 6-week intervention, 40% of the lavender oil group and 27% of the conventional treatment group were determined to be in remission. Lavender aroma significantly decreased the mean scores of ISS and PSS, suggesting an effective, noninvasive means for the treatment of insomnia in patients receiving palliative care.
NEED OF CANCER PAIN TREATMENT IN INDIA - PILOT STUDY
Suraj Pal Singh, Sushma Bhatnagar
E-mail: surajpal26@gmail.com
Introduction: The frequency of pain is about 30% in patients with newly diagnosed cancer, 50-70% in patients receiving active anticancer therapy, and 60-80% in patients with far advanced disease. 85-90% of cancer pain can be controlled by using the guidelines of the World Health Organization. Though a wide range of pain management therapies are available in India, yet many barriers interfere with adequate cancer pain management.
Objectives: To determine delay (time lag) and factors contributing to delay in cancer pain treatment, thereby determining the need of cancer pain treatment in India.
Methods: This was a prospective study conducted at Pain and Palliative Care Unit of Department of Anesthesiology, Dr. BRA Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi. Specific questions were asked to 84 patients to identify barriers to cancer pain treatment.
Results: Data from 84 patients were obtained. The data from the patients showed that majority are unaware of availability of specific cancer pain treatment and their pain is not addressed by the physician. Patients also suffer because of nonavailability of such treatment at their native places which contributes to the delay in pain management.
Conclusion: The barriers to cancer pain treatment contribute to worsen the quality of life of patients. Hence, there is a need to resolve these barriers. However, this study is limited by a small sample size. It is recommended to perform the study on a larger group of patients and explore their concerns to pain treatment.
NONPHARMACOLOGICAL INTERVENTIONS FOR MANAGEMENT OF FATIGUE AMONG CHILDREN WITH CANCER: SYSTEMATIC REVIEW OF EXISTING PRACTICES AND THEIR EFFECTIVENESS
Tushti Bhardwaj
E-mail: bhardwajtushti@yahoo.co.in
Background: Cancer-related fatigue is one of the most commonly experienced symptoms but little is known about its nonpharmacological management especially among the children. The present review synthesized the already existing nonpharmacological interventions used with children for management of fatigue in order to understand their effectiveness and explore future areas of research.
Objectives: The specific objectives of this review were: (1) To identify the commonly used nonpharmacological interventions to manage fatigue among children with cancer and to examine the appropriate setting for its administration, and (2) to examine the effectiveness of identified interventions in management of fatigue among children with cancer.
Methods: Six major electronic data base namely PsycINFO, Medline, EMBASE, CINAHL, Scopus, and Cochrane library were systematically searched for obtaining literature on fatigue and cancer limited to children and English language. From a total of 1,187 articles, six were reviewed.
Results: Three types of interventions namely complementary and alternative medicine (healing touch/massage therapy), exercise based, and nursing interventions were identified for managing fatigue. In majority of the reviewed studies, intervention was applied during the active treatment phase suggesting that the nonpharmacological interventions has more scope during active treatment phase as compared to the follow-up phase. Hospital-based settings and involvement of parents maximized the participation of children. Though, fatigue score were lower in the post-intervention phase, but none of the study could present statistical significant difference for the same, which may be attributed to short length of the intervention.
Conclusion: Hospital-based settings are more appropriate as it yields better retention rate. In absence of any strong evidence, professionals need to be cautious using already existing nonpharmacological interventions and further long-term interventions should be designed and tested in future studies in order to examine their effectiveness.
EVALUATING THE IMPACT OF PALLIATIVE CARE PROGRAMS; USING MOST SIGNIFICANT CHANGE METHODOLOGY
Grace Kivumbi, Leng M, Kivumbi G, Thyle A Collins, Venkateswaran C
E-mail: gkivumbi@gmail.com
Introduction: A significant challenge in evaluating innovative programs is methodology. Many tools focus on activity and quantitative data using predetermined groups or clinical care standards. The impact on people and values can be overlooked and key opinions missed. In addition, tools developed in other areas of social development are not assessed for their value in the palliative care (PC) setting. Most significant change (MSC) asks participants to collect narrative records that illustrate the changes sought by the project being evaluated. These are then collected, reviewed, and feedback given to identify the stories that best reflect the project outcomes. MSC has a role where a combination of deductive and inductive information is sought.
Methods: We present an evaluation of the use of MSC as an evaluation tool for PC models in Tanga, Tanzania, and Emmanuel Hospital Association (EHA), India. Examples will be shared of narrative outcomes.
Results: Training is essential and many clinicians struggle to differentiate between clinical case histories and narrative accounts. The stories collected are a rich record of changes in the three areas of project impact requested; MSC in yourself and clinical practice, the experience of patients and their families, and the experience of your colleagues and the wider community.
Conclusions: Evaluations should consider tools that allow for the voice of those involved to be heard. MSC is useful as a monitoring and evaluation tool in PC which allows for narrative voices to be heard. It is being used in projects in India and Africa.
IMPACT OF A PALLIATIVE CARE LINK NURSE PROGRAM AT MULAGO HOSPITAL, KAMPALA, UGANDA
Mwazi Batuli, Kivumbi G, Kabahweza J, Downing L, Grant L, Murray SA, Leng M
E-mail: mbatuli@yahoo.com
Introduction: A needs assessment in 2010 revealed that 40% of patients in Mulago hospital had palliative care (PC) needs. The hospital specialist palliative care team (Mulago Palliative Care Unit (MPCU)) developed and implemented a link nurse model of palliative care with empowerment of hospital staff as a key component. Twenty-seven link nurses from different clinical areas have been trained and mentored over the past 2 years and 11 clinical management protocols and an essential medicines list developed.
Objectives: To evaluate this link nurse program as a method of empowering link nurses to practice PC.
Methods: A mixed methods approach (quantitative and qualitative) was used to collect data; pre and post-course assessment confidence ratings; course evaluation forms; audit the availability of clinical guidelines; review of link-nurse activity sheets and action plans; review of MPCU patient documentation; most significant change (MSC); individual and focus group interviews.
Results: Link nurses have been directly managing 80% of patients at ward level. They report an improved attitude towards patient care and use of PC drugs, development of new skills, knowledge transfer, and improved nurse patient relationship. Challenges included heavy workload and a need to work through the ward doctors for referral and prescriptions. Overall the link nurses felt that they were able to provide better PC and had a stronger relationship with the MPCU. Complexity of patients referred to the MPCU increased.
Conclusions: Integration of PC throughout hospitals is possible, and the link-nurse program is a practical model. Generalist PC service provision can be developed and supported with referral pathways for specialist support. Patient outcomes will now be assessed.
INTEGRATING VOLUNTEERS IN A HOSPITAL-BASED SETTING: EXPERIENCE OF MULAGO NATIONAL REFERRAL HOSPITAL
Onapit I, Kivumbi G, Mwazi B, Onapit I, Toko F, Mackintosh J, Leng M
E-mail: onadit@gmail.com
Introduction: While developing the Makerere Palliative Care Unit (MPCU) strategic plan (2011-2016), a needs assessment was conducted, indicating that more than half of patients in Mulago Hospital have unmet psychological, spiritual, and social needs. Volunteers are key to palliative care (PC) models and service delivery. We developed a model volunteer network to aid in the provision of patient social and pastoral care in a government hospital setting.
Objectives: To improve the provision of practical, social, and spiritual support to patients with PC needs in Mulago National Referral Hospital.
Methods : A total of 15 volunteers were recruited. Volunteers initially undertake 20 h training followed by regular in-service training. Supervision and mentorship is provided by the volunteer coordinator who also has mentorship support and attends clinical rounds. Volunteers are linked to specific ward areas and encouraged to work closely with MPCU and ward staff. Activity data has been collected and analyzed.
Results: This program has offered an opportunity to make a holistic contribution to the patient care. Volunteers made 495 visits over the year to 94 patients. Eighty-three percent of the patients received social support, 49% spiritual support, while the rest received practical support including access to food, collecting drugs, facilitation of investigations, and physical exercise.
Conclusions: Volunteers in our experience have brought energy, personal commitment, ideas, and joy to the hospital. Many have found the experiences they have encountered, challenging yet have spoken of their own personal growth and some took this experience back into the workplace and further study.
DEVELOPING AND IMPLEMENTING PALLIATIVE CARE CURRICULUM INTO A POSTGRADUATE PROGRAM IN MULAGO NATIONAL REFERRAL HOSPITAL
Elizabeth Namukwaya, Namukwaya E, Downing J, Leng M
E-mail: liznam2002@yahoo.co.uk
Introduction: Educating healthcare workers in basic palliative care, especially those in positions of authority, is central to integrating palliative care services into clinical practice. This can be done through the introduction of an educational curriculum with clinical modeling which facilitates attitude change, embraces palliative care values while improving knowledge and skills.
Objectives: To train postgraduate doctors in palliative care.
Methods: A competency-based curriculum was implemented in the 2nd year of a 3-year postgraduate Masters in Internal Medicine. The curriculum included tutorials on: Symptom control, communication, and spiritual care and a 1 week placement in MPCU with clinical modeling of multidisciplinary palliative care values. The training is supported by the use of 11 clinical management protocols. Students’ learning was assessed through formative and summative assessment and the impact of the training assessed through a qualitative study and analysis of hospital palliative care activity.
Results: There has been an increase in the practice of generalist palliative care on the wards reflected in: An increased prescription of morphine by non-palliative care doctors, an increase in number of referrals to the palliative care team; and an increased profile for palliative care in departmental activities. An expanded curriculum is now delivered in the 1st year with nine tutorials and a 2-week placement.
Conclusion: In order to integrate palliative care into practice it is important to target postgraduate doctors. The curriculum and clinical placements should be designed in such a way as to model and change values and provide knowledge and skills.
WHO NEEDS PALLIATIVE CARE? A CATEGORIZATION SYSTEM TO SUPPORT IDENTIFICATION AND REFERRAL
Mhoira Leng, Namukwaya L, Mwazi B, Grant L, Murray S, Downing J
E-mail: dr@mhoira.net
Objectives: To identify patients in need of palliative care (PC) throughout a hospital. To integrate PC into routine clinical practice and facilitate appropriate referrals.
Methods: We developed a link nurse program with 27 trained and mentored colleagues across 11 clinical areas in Mulago Hospital and introduced training for several additional health professional cadres and implementation of 11 clinical protocols. All patients being identified, managed and referred to the specialist team used a categorization system developed with four stages: (1) Generalist needs that can be met at ward level by all health and social care workers (needs curriculum integration), (2) generalist needs that require healthcare workers to have some additional training, and (3) and (4) specialist or complex needs requiring referral and input from one member (3) or more than one member(4) of the specialist PC team.
Results: Makerere Palliative Care Unit (MPCU) offers an integrated PC model and referral pathway for specialist care but also training and mentoring to empower generalist and intermediate PC. We present 1 year data. Link nurses identified and managed 1,348 (80 %) PC patients with their ward teams. A total of 336 (20%) were referred to MPCU, and a further 300 patients from other sources. The categorization system has facilitated improved referral pathways. Qualitative data shows empowerment and ownership within the diverse clinical areas.
Conclusions: A specialist PC team can support link nurses and other health professionals in different wards to identify and treat most patients who need PC. Further research will assess the quality of referrals and outcomes for patients.
DEVELOPING “INSPIRING HOPE: HELPING CHURCHES TO CARE FOR THE SICK” (A PALLIATIVE CARE HANDBOOK FROM AFRICA)
Bates J, Wells JM, Ratcliff C, Kapolyo J, Lavy V, Thomson S
E-mail: james.wells@emms.org
Introduction: The need for palliative care (PC) around the world is overwhelming and challenges us all to respond. With ever increasing disease burdens from communicable and noncommunicable diseases, traditional models of care are stretched. Spiritual care is a key domain of PC and faith based communities are uniquely placed to respond. Faith-based organizations already contribute 40% of health care delivery in sub-Saharan Africa and over 10% in India.
Objectives:
-
To engage the Christian faith-based communities in the development and support of palliative care services.
-
Develop a resource that demonstrates the importance of PC and mobilizes a response.
Method: Following a grant award from the Diana Princess of Wales Memorial Fund in 2012, EMMS International established a working group. Objectives and terms of reference were agreed with lead author and editorial group; publication reviewed followed by a launch at African Palliative Care Association (APCA) conference 2013. Ongoing publicity and promotion to relevant communities from September 2013.
Results: A handbook comprising the following: What is PC, role of the church, resources for inspiration, reflection, teaching, motivation and action, short stories, further reading, and useful contacts.
Conclusion: Faith-based communities are an essential and integral part of understanding and offering healthcare, and can offer a unique perspective and network for spiritual support and PC. The handbook provides an excellent tool for inspiring, informing, and challenging churches to respond that is applicable beyond Africa, and for adaptation by other faith groups.
WHAT MEDICATIONS ARE OUR PATIENTS TAKING? AN AUDIT OF PRESCRIBED MEDICATION AND ADHERENCE IN AN EAST AFRICAN NATIONAL REFERRAL CENTER
Beci Evans, Holmes C, Leng M
E-mail: becievans@gmail.com
Introduction: Effective communication between prescribers and patients and their families is an essential component of safe medication use. Errors in prescribing, administering or consuming medications can reduce effectiveness and could even cause harm. In Mulago National Referral Hospital patients or attendants administer oral medications, with minimal documentation to support them.
Objectives: To determine whether the patient prescription chart accurately describes the patients’ current medications.
Method: An audit of patients referred to Mulago Palliative Care Unit (MPCU) during September 2013. Prescribed medications were recorded and the patient and/or the attendant interviewed to determine which medications they were taking.
Results: Data was collected from 18 patients, with patients prescribed 2.6 medications but taking 4.1.
In two cases the medications prescribed matched those being taken (11%). 50.7% of drugs being taken were not prescribed and 21.3% of prescribed medications were not being taken. Of patients taking morphine, 77.6% was not prescribed and 14.3% of patients were noncompliant with their prescribed morphine.
Conclusion: In this setting it is not possible to determine which medications patients are taking from review of their prescription charts. Working with our pharmacy department we will be reporting on this review, continuing postgraduate training, using standard protocols and essential medicines lists, and initiating new processes for adherence support, pharmacoeconomics, and documentation.
EMERGING TREND IN PALLIATIVE CARE IN KUMUDINI DEVI PALLIATIVE CARE CENTER: AN INDIAN PERSPECTIVE
Manjula BV
E-mail: bvmanjula59@yahoo.co.in
Introduction: Pain Relief and Palliative Care Society of Hyderabad started a Palliative Care Center of 26 beds in July 2013. Other activities are Rural Outreach and Home Care.
Objectives: We realized that some patients managed in the outpatient department and the home care needed to be admitted in a center other than the Hospital for symptom control and end of life care.
Methods: We started admitting patients of cancer and other incurable diseases from early July. Until the end of September, we had admitted 100 patients.
Results: These figures show: (1) Deaths 27%, (2) Discharges 50%, (3) some discharged patients followed up by home care team if they lived within that radius. (4) Some patients readmitted whenever there is an emergency, which caregivers could not manage.
Conclusions: (1) In the Indian scenario a hospice is usually looked at as a place to die. (2) In our center we have seen a particular trend evolving. (3) Patients are coming for symptom management and prefer to go home to spend quality time with family or to end of their life. (4) End of life for less than 30% patients.
LEADERSHIP CHALLENGES IN CAPACITY BUILDING: IN A PALLIATIVE CARE SET UP
GANPATHY KV
E-mail: kvghrt@rediffmail.com
Introduction: Capacity building is a conceptual approach to development that focuses on understanding the obstacles that inhibit organizations from realizing their developmental goals while enhancing the abilities that will allow them to achieve measurable and sustainable results.
Fundraising, training centers, learning centers and networking are some forms of capacity building. However, the most important of all is the role of a leader in building organizational capacity. The leader ensures that: (1) At an individual level, the need is to create conditions that allow individuals to build and enhance existing knowledge and skills that in turn will facilitate the process of learning and adapting to change. (2) At an Institutional level - capacity building would require modernizing existing institutions and supporting them in forming sound policies, organizational structures and effective methods of management and revenue control. (3) And at a societal level - capacity building is used to develop public administrators that are responsive and accountable.
The leaders’ Capacity is then the “ways and means needed to do what has to be done.” And includes the following components: (1) How to get the involvement of people, (2) what kind of skills, knowledge and abilities need to be developed among people, (3) ability to identify and access opportunities, (4) how to motivate people to carry out initiatives, (5) design appropriate structures needed for effective participation, (6) develop a network for economic and financial resources, (7) to design enabling policies and systems.
These would require the leaders to demonstrate both cognitive and emotional intelligence. The paper however, restricts its focus on emotional intelligence.
There is growing evidence that the range of abilities that constitutes emotional intelligence plays a key role in determining the success of a leader. Research has uncovered links between specific elements of emotional intelligence and specific behaviors associated with effectiveness or ineffectiveness of a leader.
Constellation of abilities through which a leader deals with the emotion of self and others or the ability of the leader to perceive the emotions of others and use it to guide one's thoughts and actions. According to the psychologist, Daniel Coleman, the non-cognitive abilities that help an individual to adapt to all aspects of life. He focused on four basic competencies – self-awareness, social awareness, self-management and social skills – that influences the way people handle themselves and their relationship with others.
Higher levels of emotional intelligence are associated with better performance in the following areas: (1) participative management, (2) putting people at ease, (3) self-awareness, (4) balance between personal life and work, (5) straightforwardness and composure, (6) building and mending relationships, (7) doing whatever it takes, (8) decisiveness, (9) confronting problem employees, (10) change management.
The paper aims to study the leadership challenges in the palliative care set up, by focusing on the relationship between leadership role and emotional intelligence.
Benchmark studies indicate a strong correlation between participative management and emotional intelligence. Obtaining colleague's buy in for any new initiative by engaging, involving and listening to them is the essence of the strong relationship building skill.
The nature of palliative care services being highly interdependent, calls for a multidisciplinary approach. The success of such a multi-disciplinary approach rests on a capacity of the strong relationship between the service providers.
The correlation suggests that Leaders who are skilled in fostering a strong relationship are deeply satisfied on their job. Their strong sense of relationship helps them put people at ease and comfort. This ability is deeply connected to the leader's ability to control impulses or knee jerk responses. Thus a leader's disposition is a valid determinant of the level of comfort felt by others in his/her presence.
Leaders who have an accurate perception of their strengths and weakness, demonstrated steadfast and calm during crises and relying on facts and being able to recover from mistakes are directly connected to leaders ability to control impulses. Learders’ inability to cope with stress results in poor relationship with their teammates.
Another important aspect of Palliative service is the built in an element of stress. The ability to handle stress is related to a range of leadership skills. The most important being the ability to deal with conflict. In the workplace, there's always the risk that emerging conflicts can threaten or disrupt efficiency and productivity. However, leaders with emotional intelligence are equipped to handle conflicts and provide resolution. With this skill, leaders can quickly placate any disagreements that arise between the team members. In conjunction with the above skills, leaders can use their emotional intelligence to develop a more effective workplace.





