Translate this page into:
Distress Screening Using Distress Thermometer in Head and Neck Cancer Patients Undergoing Radiotherapy and Evaluation of Causal Factors Predicting Occurrence of Distress
Address for correspondence: Dr. Naveen Salins; E-mail: naveensalins@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Distress is commonly seen in head and neck cancer patients undergoing radiotherapy. Causal factors of distress are multifactorial; which encompasses physical, psychological, spiritual, and existential factors with complex interrelationship among the factors.
Materials and Methods:
Thirty patients undergoing head and neck radiotherapy were included in the study. Patients were screened for pain scores, distress scores, physical and psychological symptoms, and spiritual and emotional distress.
Results:
Significant increasing trend seen for pain score, distress score, and total number of symptoms during 2nd week, 4th week, and on completion of radiotherapy treatment (all P's < 0.001) compared to pretreatment. Those who had chemotherapy (CT) along with radiation had significantly greater pain score (t = 5.54, P = 0.03) and distress score (t = 3.9, P = 0.05) at 2 weeks into radiotherapy compared to those who did not receive CT. There was significantly higher grade of skin toxicity in those with spiritual distress (Somers’ d = 0.36, P = 0.02) and higher grade of mucositis in those with existential distress (d = 0.34, P = 0.02) at 4 weeks into radiotherapy.
Conclusion:
Positive correlation between distress score and pain score and occurrence of physical symptoms. Increasing trend seen for pain score, distress score, and total number of symptoms during 2nd week, 4th week, and completion of radiotherapy treatment compared to pretreatment. Increase in distress score in those with existential and spiritual distress.
Keywords
Distress
Head and neck cancer
Radiotherapy
INTRODUCTION
Distress is defined as a multifactorial unpleasant emotional experience of a physical, psychological (cognitive, behavioral, emotional), social, and/or spiritual nature that may interfere with the ability to cope with cancer, its physical symptoms, and its treatment. Distress in a cancer setting is explicitly linked with physical, psychosocial, spiritual, and existential issues related to cancer diagnosis, treatment, and aftermath.[1] Elevated levels of distress is associated with poor quality of life (QoL), reduced survival, decreased patient satisfaction, and poor compliance with treatment.[2] The American National Comprehensive Cancer Network (NCCN) practice guidelines for distress management introduced the distress thermometer (DT), an easily understood, self-report measure of distress using a visual analogue scale (VAS). Patients are asked to rate their overall distress on a VAS (a thermometer) from 0 (no distress) to 10 (extreme distress). Studies have indicated that the DT is highly valid and usable in various groups of cancer patients.[34]
Patients with head and neck cancer, have disproportionately high amounts of emotional distress owing to the possibility of physical disfigurement from disease progression and/or treatment, as well as from impairment of such basic human functions such as eating, speaking, and breathing. Large numbers of patients undergoing RT for head and neck cancer have symptoms suggestive of psychosocial distress even before the beginning of treatment. This proportion increases significantly during RT.[56] This study is about prospective screening for distress in patients undergoing radiotherapy for head and neck cancer and correlation of causal factors responsible for occurrence of distress.
MATERIALS AND METHODS
Aim
-
Document rates of overall distress in head and neck cancer patients undergoing radiotherapy (RT)
-
Evaluate the demographic, physical, psychological, spiritual, and existential predictors of overall distress.
Methods
Thirty patients undergoing head and neck radiotherapy at Department of Radiation Oncology Victoria Hospital, Bangalore Medical College and Research Institute, Bangalore were randomly chosen for the study.
Inclusion
Patients aged >18 years with a cancer diagnosis, aware of diagnosis and treatment plan, receiving radiotherapy with a curative intent, willingness to participate, and physically fit enough to fill in the questionnaire were included in the study.
Exclusion
Patients treated with palliative intent, previous history of radiotherapy, diagnosis of depression or mood disorder, and patients on antidepressants and anti-psychotics.
Concurrent chemoradiation is the standard of care for advanced stage III and IV head and neck cancer and in postoperative cases with high-risk features like positive margin, positive nodes, and T3 and T4 cases. Ten patients did not receive CT due to advanced age, poor performance status, early stage, and postoperative cases with low risk factors.
The screening tool used was distress thermometer (DT) a VAS used to screen distress in cancer patients, which is a validated screening tool for distress recommended by National Comprehensive Cancer Care Network (NCCN). Pain score was documented using numerical rating scale (NRS).
Patients included in the study were screened for presence of physical symptoms (pain, nausea, vomiting, oral ulcers, dysphagia etc.), psychological symptoms (low mood, anxiety), spiritual distress (loss of faith, God questions), existential distress (meaning questions), family support, financial support, and communication concerns.
Radiation toxicity was assessed using Radiotherapy Oncology Group (RTOG) toxicity grading.
Patients were screened on five occasions: a. Prior to commencing RT. b. Two weeks on RT. c. Four weeks on RT. d. On completion of RT. e. Four weeks after completion of RT. During each assessment, patients were screened for pain score, distress score, symptom checklist, RTOG toxicity screening for skin, and mucosal toxicity.
The entire questionnaire was completed by the radiotherapy trainee residents and results were tabulated in Microsoft excel and analyzed using SPSS 20.0. Patient's informed consent was obtained and approval from hospital ethics committee and other relevant institutional review board was sought prior to commencement of this study.
RESULTS
Thirty patients participated in the study of which 17 were male and 13 were female. Age of the participants ranged from 26 to 82 years and average age of the study population was 53.2 years.
Out of 30 patients, five had malignancy involving hypopharynx, eight involving oropharynx, 15 involving oral cavity, one involving larynx, and one involving neck nodal metastasis with unknown primary. Three had stage I diagnosis, one had stage II diagnosis, eight had stage III diagnosis, and 18 had stage IV diagnosis. Twenty patients received concurrent CT and 10 patients received radiotherapy alone. Eighteen patients received conventional radiotherapy 70 Gy in 35 fractions and other 12 received lesser doses.
Pain was the most common symptom before, during, and after radiotherapy with increase in pain scores during RT. Mean pain score peaked from 2.86 prior to RT to 4.90 and 5.36 at 4 weeks during RT and completion of RT, respectively [Table 1].
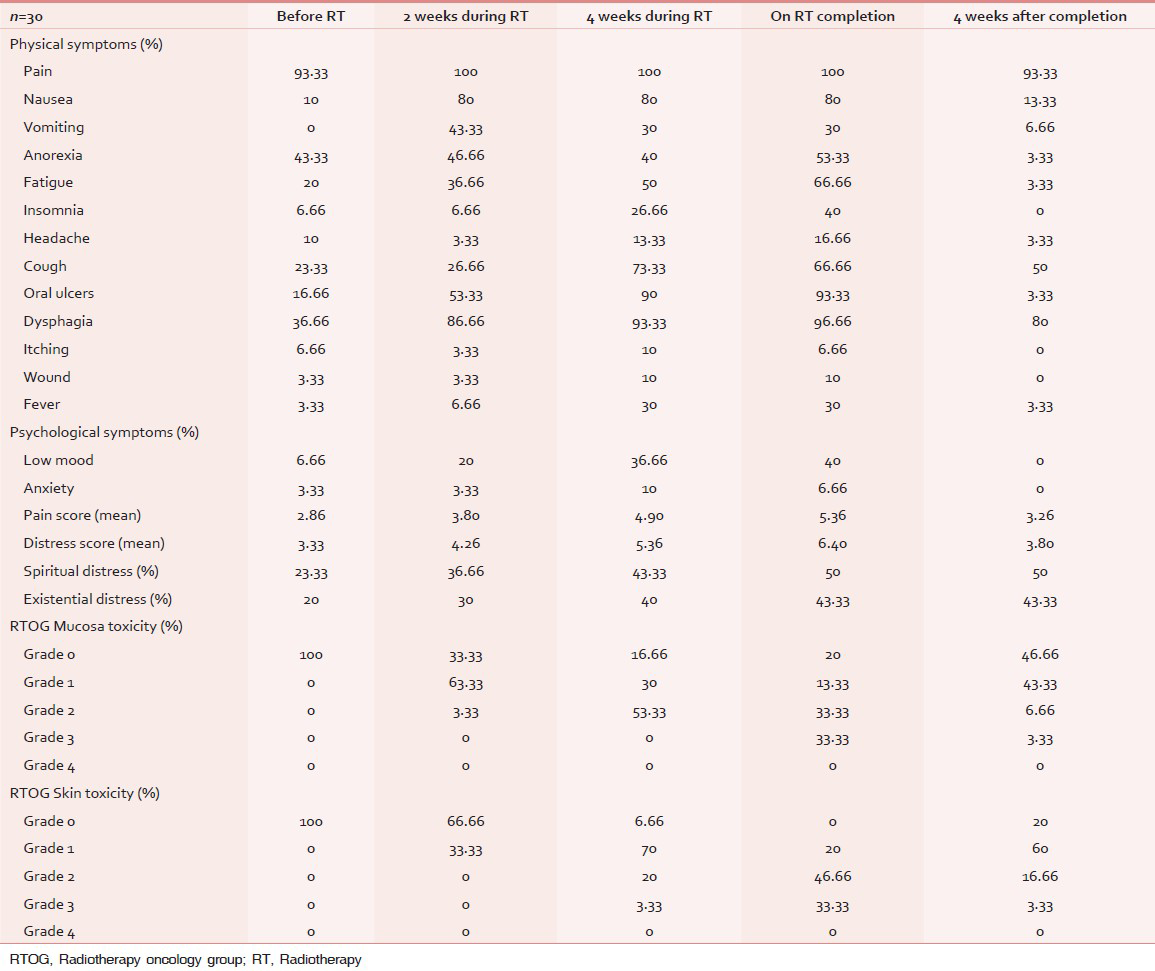
Higher incidence of physical symptoms such as nausea, vomiting, anorexia, fatigue, cough, oral ulcers, and dysphagia was seen during RT treatment and during completion of RT. These symptoms subsided within 4 weeks of RT completion [Table 1].
RT induced mucosal toxicity was seen during treatment and there was a sustained increase in percentage of toxicity over the period of treatment and decrease in incidence over next 4 weeks after completion. Higher grades of mucosal toxicity was noted in week 4 of treatment and during completion of RT. RT induced skin toxicity followed similar pattern of mucosal toxicity; however, the skin toxicity persisted even at 4 weeks after RT completion [Table 1].
Spiritual distress was seen in 23.3% of patients prior to starting RT and incidence peaked to 43.3% 4 weeks during RT and 50% at completion and remained the same even at 4 weeks after RT completion. Existential distress followed a similar pattern as spiritual distress, however its incidence was lower than spiritual distress.
Mean distress score prior to RT commencement was 2.86, which peaked to 5.36 and 6.40 at 4 weeks during RT and RT completion, respectively. Distress scores decreased to 3.80 during 4 weeks after completion of RT.
None of the patients included in the study had concerns regarding medical communication and all patients enjoyed good family support. As all the patients included in the study were treated in a public health system, hence there was no overt finance related issue.
The results suggest that there was a significant increasing trend for increase of pain score, distress score, and total number of symptoms during 2nd week, 4th week, and completion of radiotherapy treatment (all P's < 0.001) compared to pretreatment. These tended to return to baseline level 1 month after completion of treatment. Those who had CT along with radiation had significantly greater pain score (t = 5.54, P = 0.03) and distress score (t = 3.9, P = 0.05) at 2 weeks into radiotherapy compared to those who did not receive CT. There were a significantly greater number of distressful symptoms at 2 weeks (t = 5.81, P = 0.02), 4 weeks (t = 4.81 P = 0.05), and after completion (t = 4.88, P = 0.03) of radiotherapy and greater distress after one month after radiotherapy (t = 5.41, P = 0.02) in females compared to males. There was a significant increase in distress score in those with existential distress (t = 2.28, P = 0.03) at 4 weeks of RT. There was a near significant increase in total number of distressful symptoms and pain score (t = 2.49, P = 0.02) after completion of treatment in those with existential distress compared to those without the same. There was a trend towards increase in symptoms and distress in those with spiritual distress, but was not significant compared to those without. There was significantly higher grade of skin toxicity in those with spiritual distress (Somers’ d = 0.36, P = 0.02) and higher grade of mucositis in those with existential distress (d = 0.34, P = 0.02) at 4 weeks into radiotherapy.
DISCUSSION
Head and neck cancer patients who have advanced disease have higher incidence of distress and should be routinely evaluated for distress so that it is detected early and appropriate intervention is made.[7] Distress has significant relationship to health-related quality of life (HRQoL) status and occurrence of specific symptoms. In this study clinically significant distress (distress score >4) was seen during 2 weeks on treatment, 4 weeks on treatment, and treatment completion (4.26, 5.36, and 6.40, respectively). Lower distress scores were seen before treatment and 4 weeks after completion of treatment.[8]
The most important physical symptoms noted in head and neck cancer patients during treatment are pain, mouth ulcers, and swallowing problems. In this study pain was seen in >90% of cases with higher pain scores during 4 weeks on RT and completion. Mouth ulcers and difficulty in swallowing was noted in up to 90% of patients during mid-treatment and on completion. Disturbances in psychosocial functioning and psychological distress are reported by a considerable number of patients; worry, anxiety, mood disorder, fatigue, and depression are the main symptoms. Cancer of the head and neck has a negative effect on social, recreational, and sexual functioning. In this study low mood was observed in 1/3 of patients during late phases of RT treatment and completion and anxiety was seen in less than 10% of patients.[9]
Pain is common in patients with head and neck cancer and they also have higher incidence of breakthrough pain. In this study, mean pain score was mild to moderate during 2 weeks on treatment and in next 4 weeks there was a steady increase in pain score ranging in moderate intensities and peaking during RT completion. The important observation made was large number of patients included in the study had inadequate pain relief. A positive correlation was noted between pain score and distress score. The majority of patients in India have head and neck cancer and it is imperative that we must approach the problem of unrelieved pain in these patients as it has a direct impact on patient's HRQoL.[10] Studies show that pain also has an adverse effect on the general well-being and psychological distress in patients with head and neck cancer patients who were free of disease.[11]
In this study, RTOG toxicity assessment showed higher grade of mucosal and skin toxicity during 4 weeks on treatment and RT completion. Late radiation-induced toxicity in head and neck cancer patients has a significant impact on the more general dimensions of health related quality of life (HRQoL). As the patients in this study received conventional radiotherapy (cobalt), newer radiation-induced delivery techniques may minimize these toxicities.[12]
Total distress, emotional, and social distress subscales were found to have positive correlation with anxiety and depression. Results of present study suggest significant psychological morbidity in head and neck cancer patients undergoing curative treatment.[13] One-third of patients were depressed in late stages of cancer treatment. Patients undergoing radiation are increasingly depressed as treatment progresses, with worsening QoL during the treatment.[14] Rates of depression in patients with head and neck cancer increase after cancer treatment, with a third of patients experiencing clinically significant symptoms of depression after radiotherapy.[15]
Up to half of patients had spiritual and existential distress during and late stages of cancer treatment, completion, and 4 weeks after completion of treatment. Study showed positive correlation between existential distress and distress score, pain score, occurrence of distressful symptoms, and mucosal toxicity; and positive correlation between spiritual distress and skin toxicity. Spiritual assessment should be a part of the interdisciplinary approach to optimize symptom control.[16] Existential issues can be very disturbing to patients, leading to distress and potentially to a lowered quality of life (QoL).[17] The meaning-making intervention can be presented as an approach to address normative distress associated with the search for meaning within the context of cancer.[18]
In this study patients who had CT with radiotherapy had higher incidence of pain scores and distress score during 2 weeks on treatment. Studies showed that there is a higher incidence of distress in the chemoradiation group compared to RT group[19] A number of early morbidity items were found to be more prevalent and/or more severe after RT + CT than after RT alone.[20]
CONCLUSION
-
Positive correlation seen between distress and pain score, and distress score and occurrence of physical symptoms
-
Those who had chemotherapy along with radiation had significantly greater pain score and distress score compared to those who did not receive chemotherapy
-
Increase in distress score in those with existential and spiritual distress.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Screening for distress and unmet needs in patients with cancer: Review and recommendations. J Clin Oncol. 2012;30:1160-77.
- [Google Scholar]
- Screening and referral for psychosocial distress in oncologic practice: Use of the Distress Thermometer. Cancer. 2008;113:870-8.
- [Google Scholar]
- Comprehensive N, Network C. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) Distress Management; Annual guidelines. 2013
- [Google Scholar]
- Screening cancer patients for distress: Guidelines for routine implementation. Community Oncol. 2011;8:502-5.
- [Google Scholar]
- Psychological distress in patients with head and neck cancer: Review. Br J Oral Maxillofac Surg. 2001;39:67-70.
- [Google Scholar]
- Higher distress relates to poor quality of life in patients with head and neck cancer. Int J Oral Maxillofac Surg. 2009;38:955-9.
- [Google Scholar]
- Prevalence, predictive factors, and screening for psychologic distress in patients with newly diagnosed head and neck cancer. Cancer. 2000;88:2817-23.
- [Google Scholar]
- A descriptive analysis of the relationship between quality of life and distress in individuals with head and neck cancer. Support Care Cancer. 2011;20:2157-65.
- [Google Scholar]
- Physical and psychosocial correlates of head and neck cancer: A review of the literature. Otolaryngol Head Neck Surg. 1999;120:427-36.
- [Google Scholar]
- Prevalence and characteristics of breakthrough pain in patients with head and neck cancer: A cross-sectional study. J Palliat Med. 2010;13:291-5.
- [Google Scholar]
- A prospective, longitudinal study of pain in head and neck cancer patients. Head Neck. 1999;21:531-7.
- [Google Scholar]
- Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol. 2008;26:3770-6.
- [Google Scholar]
- Distress overlaps with anxiety and depression in patients with head and neck cancer. Psychooncology. 2007;16:582-6.
- [Google Scholar]
- Deterioration in quality of life and depressive symptoms during radiation therapy for head and neck cancer. Otolaryngol Head Neck Surg. 2007;136:108-11.
- [Google Scholar]
- Psychological distress (depression and anxiety) in people with head and neck cancers. Med J Aust. 2010;193:S48-51.
- [Google Scholar]
- The frequency and correlates of spiritual distress among patients with advanced cancer admitted to an acute palliative care unit. Am J Hosp Palliat Care. 2011;28:264-70.
- [Google Scholar]
- The challenge of existential issues in acute care: Nursing considerations for the patient with a new diagnosis of lung cancer. Clin J Oncol Nurs. 2012;16:E4-11.
- [Google Scholar]
- The existential plight of cancer: Meaning making as a concrete approach to the intangible search for meaning. Support Care Cancer. 2008;16:779-85.
- [Google Scholar]
- Preliminary investigation of symptom distress in the head and neck patient population: Validation of a measurement instrument. Am J Clin Oncol. 2006;29:158-62.
- [Google Scholar]
- Early morbidity after radiotherapy with or without chemotherapy in advanced head and neck cancer. Experience from four nonrandomized studies. Strahlenther Onkol. 2003;179:390-5.
- [Google Scholar]






