Translate this page into:
Hypofractionated Radiotherapy for Palliation in Locally Advanced Head and Neck Cancer
Address for correspondence: Dr. RK Spartacus, Department of Radiotherapy, SMS Medical College, Jaipur, Rajasthan, India. E-mail: meg80224@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
In India, a considerable proportion of patients with head and neck cancer present with locoregionally advanced disease. Symptom palliation becomes a major objective in these cases when they could not be considered for a curative approach.
Aims:
The aim of this study is to assess the role of palliative radiotherapy for symptom control in patients with locally advanced head and neck cancer.
Settings and Design:
This was a retrospective study.
Subjects and Methods:
Between July 2015 and June 2016, 98 patients with stage IV head and neck cancer were treated with palliative radiotherapy 25 Gray (Gy)/4 fractions (fr)/1 fraction (6.25 Gy)/week. Presenting symptoms were noted. The primary end point was relief of symptoms in the 4th week after radiotherapy. Percentage symptom relief was quantified by the patient using a rupee scale. Treatment response was noted using the WHO criteria. Acute toxicity was graded as per the Radiation Therapy Oncology Group (RTOG) criteria.
Results:
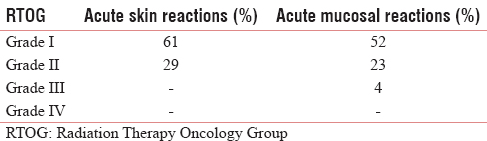
The most common presenting symptom was pain. At 4 weeks after radiotherapy completion, all patients had >50% pain relief. Dysphagia was improved in 82% of patients. Respiratory distress was improved in all the symptomatic patients. Tumor complete response (CR) was seen in 2 patients, partial response in 89, stable disease in 3, and progressive disease in 4. RTOG Grade 2 and 3 acute skin and mucosal toxicities were seen in 29% and 27% cases, respectively. No patient had Grade 4 adverse effect.
Conclusions:
Hypofractionated radiation could provide effective symptom palliation in advanced head and neck cancers. The weekly schedule was well tolerated and found convenient by the patients.
Keywords
Head and neck carcinoma
palliation
radiotherapy
INTRODUCTION
Squamous cell carcinoma of the head and neck (SCCHN) is one of the most common cancers seen in India, constituting up to 25% of the overall cancer burden. A sizeable majority present with locoregionally advanced disease.[12] Extensive locoregional spread, poor general condition of the patient, distant metastasis, or comorbidities preclude curative treatment. This group of patients requires some form of treatment to control their locoregional disease and to alleviate symptoms. A palliative radiotherapy schedule should target symptom control and tumor regression within a short overall treatment time with minimal side effects.[34] Various palliative schedules have been used in head and neck cancer. Our study retrospectively assesses the 25 Gy/4 fr/1 fr per week schedule which has been practiced at the department.[5] Our institute serves as a comprehensive cancer care center in the North-Western India and caters to the needs of people of Rajasthan as well as eastern Uttar Pradesh, Haryana, and Madhya Pradesh.
SUBJECTS AND METHODS
Ninety-eight patients with inoperable, head, and neck cancer not fit for radical treatment were treated with a short course of radiotherapy (July 2015–June 2016) after obtaining informed consent. Patients with stage IV American Joint Committee on Cancer (AJCC) who had received no prior radiotherapy or chemotherapy, no previous history of cancer and of Eastern Cooperative Oncology Group performance status 2 and 3 were included for this retrospective study. The consideration for palliative approach was based on factors which included Medically inoperable, fixed, and unresectable disease; very advanced locoregional disease; poor general condition/comorbidities; metastatic disease; achievable symptomatic relief; and short life expectancy.
All the patients were treated in Cobalt 60 teletherapy units, and the gross tumor volume (including the primary tumor and/or involved nodes) with 2 cm margin was irradiated. Patients received 4 weekly fractions (day 1, 8, 15, and 22) for a total dose of 25 Gy. That is a dose of 6.25 Gy was given once a week. The biologically equivalent dose (BED) was 40.6 Gy10 and 77.08 Gy3 for tumor and late reacting tissues, respectively. Surface bolus was applied in fungating lymph nodes.
At the 4th week after completion of radiation, percentage symptom relief was quantified by the patient using a rupee scale.[3] Treatment response was assessed using the WHO Criteria.[6] Acute skin and mucosal reactions grading was done as per the Radiation Therapy Oncology Group toxicity criteria.[7] Further treatment of patients was done according to tumor regression status.
RESULTS
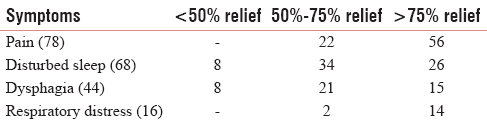
The study group had 78 male and 20 female patients with a mean age of 58 years. Patient characteristics are shown in Table 1. The most common presenting symptom was pain as reported by 78 patients. 68 patients complained of disturbed sleep and 90 complained of a decline in general well-being. At 4 weeks after radiotherapy completion, majority of patients had appreciable relief in symptoms [Table 2]. All patients had >50% pain relief. Dysphagia was improved in 36 patients (out of the 44 who had this complaint). Respiratory distress was improved in all the symptomatic patients. Appreciable reduction in tumor size, bleeding, and fungation was observed by many of the patients. Palliation of symptoms allowed better sleep in 60 (out of the 68 who initially complained of insomnia) patients. An overall improvement in general well-being was observed by 54 (out of the 90 who had this complaint) patients.

Regarding disease control, complete response (CR) was seen in two patients. Partial response (PR) was achieved in 89 patients and 2 had progressive disease [Table 3]. Grade 2 and 3 acute skin and mucosal toxicities were seen in 29% and 27% cases, respectively [Table 4].

DISCUSSION
In India, about 70%–75% of cases of head and neck cancer present in a locally advanced inoperable stage.[4] Palliation of symptoms becomes a primary the primary objective. Palliative radiation in any advanced cancer should aim to relieve the symptoms quickly while minimizing the side effects. The treatment should also be delivered in the shortest possible time for the patients’ and caregivers’ convenience.[8]
Vikram suggested that advanced head and neck cancers from developing countries do not show favorable outcomes and it would be prudent to explore novel ways of providing relief. A significant proportion of advanced stage patients have life-limiting disease. Totally 808 untreated head and neck cancer patients (91% stage IV) followed up longitudinally; the median survival time was approximately 100 days. It has further been studied that treated patients showed higher survival rates compared to best supportive group and type of treatment performed, even when aggressive, did not influence the survival. When the patient has more than 80% likelihood of death within 12 months, palliative treatment seems judicious and such practices have become standard therapeutic decisions for many other advanced or metastatic solid tumors.[9]
Weissberg et al. compared conventionally fractionated (60 Gy to 70 Gy in 6–7 weeks) versus hypofractionated (40 Gy to 48 Gy in 10/12 fractions at 400cGy/fr) palliative external beam radiation therapy schedules in 64 patients with stages III and IV surgically unresectable SCCHN. No differences were noted in tumor control, acute side effects, or long-term sequelae.[10]
In a large study, 505 patients with stage IV head and neck squamous cell carcinoma, Mohanty et al. gave a uniform regimen of 20 Gy/5 fractions, once daily over l week. They reported good symptom relief (>50% for pain, 53% for dysphagia, 57% for hoarseness, 47% for otalgia, 76% for respiratory distress, and 59% for cough). At 1-month assessment, 189 (37%) achieved a PR and had ambulatory physical state suited for further curative-dose radiotherapy. The main acute toxicity of palliative radiotherapy was patchy oropharyngeal mucositis and dermatitis.[11]
Ghoshal et al. studied 25 patients with stage 3 and 4 head and neck cancer who were treated with a short course of palliative radiotherapy (30 Gray [Gy] in 10 fractions over 2 weeks). Baseline symptoms were assessed using an 11-point numerical scale for pain, dysphagia, cough, insomnia, and dyspnea. The primary end point was relief of symptoms in the 4th week after radiotherapy. All 22 patients with pain and 90% of patients with dysphagia, dyspnea, and disturbed sleep had >50% relief in symptoms after radiotherapy. Cough was relieved in 60% of cases.[4] Similar improvement in symptoms was seen in our study.
The “Christie scheme” used a hypofractionated scheme of radiotherapy consisting of 16 fractions of 3.125 Gy. In 158 patients, they had 45% CR and 28% PR; an overall response rate of 73% was achieved. Nearly 6% had stable disease (SD) and 21% progressed during or directly after completion of treatment. The CR rate was higher in this study as they also included stage I–III in their study whereas our study included only stage IV patients. Acute grade >3 skin and mucosal toxicities were observed in 45% and 65% of patients, respectively.[3]
Paris et al. reported on a phase I/II study of novel fractionation involving 370 cGy/fraction given twice daily for 4 fractions over 2 days. This was repeated every 3–4 weeks giving a total dose of 44 Gy over 9 weeks. Good palliation was achieved in 33 (84.6%) of 39 lesions in 37 patients with minimal acute toxicity interruptions. Irradiation had to be discontinued in 18 and no long-term complications.[12]
The QUAD SHOT regimen gave 14 Gy in 4 fractions, given twice daily and at least 6 h apart, for 2 consecutive days. This was repeated at 4 weekly intervals for a further two courses if there was no tumor progression. Thirty eligible patients (29 stage IV, 20 performance status 2–3) had at least one treatment and 16 patients completed all three cycles. Sixteen patients (53%) had an objective response (2CR, 14PR) and a further seven had SD. The treatment was well tolerated, with improved quality of life (QoL) in 11 of 25 evaluable patients (44%).[13]
The “Hypo Trial” planned 37 patients to receive 30 Gy in 5 fractions at 2/week, at least 3 days apart, with an additional boost of 6 Gy for small volume disease (< or = 3 cm) in suitable patients. The majority (73%) presented with stage III-IV disease. Thirty-five patients received radiotherapy, 1 died before treatment, and one refused treatment. Of the 35 patients receiving radiotherapy, 31 (88%) received >30 Gy. Of the 35 patients who received treatment, the overall objective response was 80%. Grade 3 mucositis and dysphagia were experienced in 9/35 (26%) and 4/35 (11%), respectively. Thirteen (62%) reported an overall improvement in QoL and 14 (67%) experienced an improvement in pain.[14]
Talapatra et al. in an extensive review favored a short-course fractionated regimen (20 Gy/5 or 30 Gy/10 fractions) or cyclical treatment (QUAD SHOT) over protracted courses of radiotherapy for the purpose of palliation.[1]
The current schedule of 6.25 Gy/week for 4 fractions gave BED similar to the well acceptable 30 Gy/10 fractions. In a department dealing with large number of cancer patients, this schedule could optimize available resources in terms of technical workforce and machine time. Furthermore, the weekly schedule was convenient to the patient who had to come just once a week for treatment. This avoided long stay at the hospital for patients as well as the caretakers who mostly came from far-flung rural areas.
CONCLUSIONS
The once weekly hypofractionated schedule showed results comparable with other palliative schedules. Acceptable symptom palliation was achieved in the majority of patients. The weekly schedule was well tolerated by the patients and convenient to both the patient and the accompanying relative/caretaker who mostly came from far-flung areas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Palliative radiotherapy in head and neck cancers: Evidence based review. Indian J Palliat Care. 2006;12:44-50.
- [Google Scholar]
- Hypofractionated, palliative radiotherapy for advanced head and neck cancer. Radiother Oncol. 2008;89:51-6.
- [Google Scholar]
- Hypofractionated radiotherapy denoted as the “Christie scheme”: An effective means of palliating patients with head and neck cancers not suitable for curative treatment. Acta Oncol. 2009;48:562-70.
- [Google Scholar]
- Palliative radiotherapy in locally advanced head and neck cancer-a prospective trial. Indian J Palliat care. 2004;10:19-23.
- [Google Scholar]
- Palliative radiotherapy in the management of advanced pediatric malignancies. Natl J Med Res. 2014;4:58-60.
- [Google Scholar]
- Radiation Therapy Oncology Group Acute Radiation Morbidity Scoring Criteria. Available from: http://www.rtog.org/ResearchAssociates/AdverseEventReporting/AcuteRadiationMorbidityScoringCriteria.aspx
- Quad shot: A short but effective schedule for palliative radiation for head and neck carcinoma. Indian J Palliat Care. 2009;15:137-40.
- [Google Scholar]
- Cancers of the head and neck region in developing countries. Radiother Oncol. 2003;67:1-2.
- [Google Scholar]
- High fractional dose irradiation of advanced head and neck cancer. Implications for combined radiotherapy and surgery. Arch Otolaryngol. 1983;109:98-102.
- [Google Scholar]
- Short course palliative radiotherapy of 20 Gy in 5 fractions for advanced and incurable head and neck cancer: AIIMS study. Radiother Oncol. 2004;71:275-80.
- [Google Scholar]
- Phase I-II study of multiple daily fractions for palliation of advanced head and neck malignancies. Int J Radiat Oncol Biol Phys. 1993;25:657-60.
- [Google Scholar]
- The ‘QUAD SHOT’ – A phase II study of palliative radiotherapy for incurable head and neck cancer. Radiother Oncol. 2005;77:137-42.
- [Google Scholar]
- Hypofractionated radiotherapy for the palliation of advanced head and neck cancer in patients unsuitable for curative treatment-”Hypo Trial”. Radiother Oncol. 2007;85:456-62.
- [Google Scholar]






