Translate this page into:
Radiation-Induced Neuropsychiatric Manifestations in a Patient with Brain Metastasis: A Diagnostic and Therapeutic Challenges for Consultation-Liaison Psychiatrist
Address for correspondence: Dr. Ramdas Ransing, Department of Psychiatry, B.K.L. Walawalkar Rural Medical College, Sawarde, Ratnagiri - 415 606, Maharashtra, India. E-mail: ramdas_ransing123@yahoo.co.in
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The aim of this case report is to highlight diagnostic and therapeutic challenges for consultation-liaison psychiatrist in the case of radiation-induced neuropsychiatric syndrome. We report the case of a 61-year-old man presented with neurological and psychiatric manifestations following the radiation therapy for non-small cell lung carcinoma with brain metastasis. We have briefly reviewed and discussed the risk factors, clinical features, diagnostic, therapeutic, and preventive aspect of radiation-induced neuropsychiatric manifestations.
Keywords
Acute radiation syndrome
acute stroke
delirium
non-small cell lung carcinoma
INTRODUCTION
Lung cancer is the leading cause of cancer mortality worldwide, accounting about 16%–18% of total death from cancer.[1] Among those, approximately 7.4% of non-small cell lung cancer patients present with brain metastases (BM) and 25%–30% will develop BM during the course of the disease.[23]
The recently published Cochrane review reports that the palliative whole brain radiotherapy in the dose of 30 Gy over the period of 2 weeks achieves palliation in terms of symptom in almost 64%–85% patients with brain metastasis.[45] Although the cranial irradiation is relatively well-tolerated therapy, it can cause number of short- and long-term adverse effect such as acute toxicity, ischemic stroke, cerebral microbleed, delirium, and long-term cognitive deterioration.[678] Most of these manifestations are difficult to diagnose and treat due to nonspecific and overlapping symptoms.
The literature in terms of management of radiation-induced acute neuropsychiatric manifestations is limited. Through this case report, we present an interesting case of radiation-induced neurobehavioral syndrome in a patient with brain metastasis.
CASE REPORT
Mr. XYZ, a 61-year-old man was undergoing treatment from tertiary care center (Model Cancer Care Centre) for Adenocarcinoma of Lung since June 2007 [Figure 1a-Heterogeneous soft-tissue density lesion in the right upper lobe compressing the anterior-posterior bronchus of right upper lobe causing abrupt narrowing of bronchus]. He was receiving tablet gefitinib 250 mg/day and poor compliance to medicine. There was no history of past psychiatric disorder, neurological deficit, and other medical disorders.
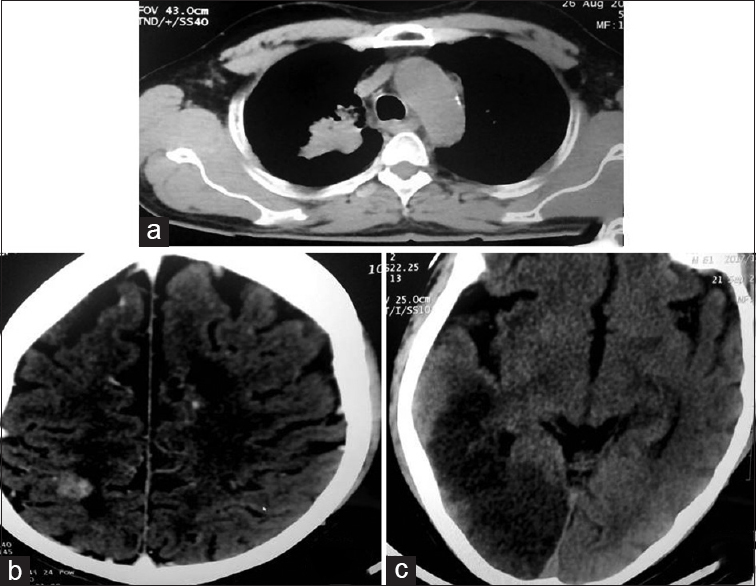
- (a) Carcinoma of lung, (b) cerebral metastasis, (c) acute infarct in temporo-occipital region (venous origin)
During his regular follow-up at our center, he developed difficulty in speech and headache. His computed tomography (CT) brain showed a well-defined round, hyperdense, enhancing lesion in the subcortical white matter of right high parietal region with surrounding hypodensity [Figure 1b]. These features were suggestive of brain metastasis with cerebral edema.
Subsequently, he was admitted to oncology inpatient department for the treatment of metastasis to the brain with Stage IV Adenocarcinoma lung [Figure 1b]. At the time of admission, patient was conscious and physically stable with no obvious abnormality in his complete blood count, serum electrolytes, thyroid function test, and liver function test. Radiation therapy of doses 30 Gy/setting was planned for brain metastasis over the period of 2 weeks and in 10 fractions. The patient was admitted and injectable dexamethasone 10 mg/day was started as prophylactic antiemetic along with injectable pantoprazole 20mg/day. He underwent 5 radiation fractions in 7 days. First 5 radiation fractions were uneventful. After 6th radiation fraction, the patient developed seizures, slurring of speech, decreased level of consciousness and irritability. The above symptoms developed after 2 h of radiation exposure. Probable diagnosis of delirium secondary to acute radiation syndrome with neurovascular type was considered.
The CT brain was suggestive of large acute infarct in cortical and subcortical areas of the right temporo-occipital lobe and small infarcts in bilateral occipital and temporal lobe [Figure 1c]. The dose of dexamethasone was increased to 10 mg QID, and the patient was started on injection mannitol 100 mg TID in view of cerebral and vasogenic edema. Injection haloperidol 2.5 mg/day with injection promethazine 25 mg was started to manage the symptoms of delirium. Considering the poor outcome of the medical condition, relatives of patient decided to shift the patient to a higher center. Therefore, we failed to assess the clinical outcome of delirium and associated medical condition.
DISCUSSION
In this case, the patient reported with acute onset of neurobehavioral symptoms following 6th fraction of radiation dose. The initial clinical presentation was suggestive of neurovascular type of acute radiation syndrome. Acute neurovascular syndrome or central nervous system (CNS) syndrome develops within 6–24 h of radiation dose of more than 10 Gy.[69] It results from localized changes in CNS, namely, damage to blood-brain barrier, interstitial edema, petechial hemorrhages, and acute edema. This localized damage to brain manifests as disorientation, fatigue, fever, headache, nausea, vomiting, dysphagia, dysarthria, confusion, ataxia, and seizure.[69]
In our case, CT brain demonstrated the acute infarct in temporal and occipital region supporting the neurological deficit in the patient and also it has clear temporal association with radiation therapy. The relationship between stroke and cancer is more complex, they may occur independently, or cancer may directly or indirectly lead to stroke.[10] Cancer-related hypercoagulability, nonbacterial thrombotic endocarditis, direct tumor compression, and treatment-related side effects are the important reasons for stroke in a patient with brain metastasis. The radiation to brain almost doubles the risk of developing ischemic stroke in those patients.[1112] The radiation dose (>10 Gy), age (>61 years), advanced stage of adenocarcinoma and related hypercoagulability were important predisposing factors for developing stroke in our patient.[813] The CT and magnetic resonance imaging are reliable, accurate and useful to demonstrate the presence of brain edema and ischemic/hemorrhagic stroke in such patient.[9]
Management of this case was challenging in our rural and limited setting. Dexamethasone is potent and effective steroid used to reduce the tumor-associated edema (dose-10 mg to 100 mg/day),[14] radiation-induced cerebral edema (dose-10 mg to 100 mg/day),[14] and as prophylactic antiemetic (dose-2 mg to 10 mg/day)[15] in patients with radiation-induced emesis. The dexamethasone-induced psychiatric disorders such as delirium, psychosis, insomnia, and irritability are common and known to complicate the clinical picture.[1416] The initial low dose of dexamethasone, the presence of acute brain infarct favors the diagnosis of radiation-induced delirium than the dexamethasone-induced delirium. Therefore, the dose to dexamethasone was increased to optimal dose, i.e., 40 mg/day along with injectable mannitol 300 mg/day after CT brain to reduce the radiation-induced cerebral edema. Further, we decided to start injectable haloperidol to reduce the symptoms of delirium. Injectable dose was preferred due to poor oral intake of patient and risk of aspiration pneumonia. Haloperidol is the first line of drug for the treatment of delirium in patients with cancer.[17] It is an inexpensive antipsychotic that can be used in all settings. The antipsychotics also help to reduce the nausea and vomiting associated with radiotherapy and chemotherapy.[18] Among the antipsychotics, penfluridol, haloperidol, and olanzapine are the widely studied and clinically effective drugs to reduce metastatic growth to the brain.[192021] In this case, we used promethazine as rapid tranquilizer and to control extrapyramidal side effects of haloperidol.[22] However, one should try to avoid promethazine while treating postradiation syndrome, as it blocks the neuroprotective effect of acetylcholine. Memantine, an N-Methyl-d-Aspartate receptor antagonist is effective in prevention of neurological excitotoxicity.[23] Therefore, while treating the radiation-induced adverse effect, clinician must consider the therapeutic role of various antipsychotics and neuroprotectors.
The acute neurovascular syndrome is associated with poor outcome and can lead to death in approximately 6.7% of patients.[24] Early prompt diagnosis and management by multidisciplinary team including psychiatrist helps in reduction of long-term hospitalization and reduces the mortality, morbidity among these patients.[1724] The clinical features of radiation-induced adverse effects are nonspecific and overlapping with that of physical comorbidities. Thus, diagnosis should be focused on the exclusion of other causes of delirium. Brain imaging, complete blood count, serum electrolytes, electrocardiography, and electroencephalography must be considered in such patients. The identification of risk factors such as age, radiation dose, medical comorbidities, and administration of neuroprotectors during preradiation period may help to reduce morbidities associated with such adverse effects.[813]
CONCLUSION
Consultation-liaison psychiatrist, particularly those who work in oncology or intensive care setting should be aware of these diagnostic and therapeutic challenges in the patient receiving radiation therapy for brain metastasis. In addition, there is a paucity of literature, indicating the need of further research on management of neuropsychiatric symptoms of acute radiation syndrome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Current management of brain metastases, with a focus on systemic options. J Clin Oncol. 2005;23:6207-19.
- [Google Scholar]
- Treatment of brain metastases from lung cancer: Chemotherapy. Lung Cancer. 2004;45(Suppl 2):S253-7.
- [Google Scholar]
- Role of palliative radiotherapy in brain metastases. Indian J Palliat Care. 2009;15:71-5.
- [Google Scholar]
- Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev. 2012;18:CD003869.
- [Google Scholar]
- Mechanisms of radiotherapy-associated cognitive disability in patients with brain tumours. Nat Rev Neurol. 2017;13:52-64.
- [Google Scholar]
- Dose-dependent effects of radiation therapy on cerebral blood flow, metabolism, and neurocognitive dysfunction. Int J Radiat Oncol Biol Phys. 2009;73:1082-7.
- [Google Scholar]
- Stroke after radiation therapy for head and neck cancer: What is the risk? Int J Radiat Oncol Biol Phys. 2016;96:589-96.
- [Google Scholar]
- Medical management of the acute radiation syndrome. Rep Pract Oncol Radiother. 2011;16:138-46.
- [Google Scholar]
- Stroke and cancer – A complicated relationship. J Neurol Transl Neurosci. 2014;21:1039.
- [Google Scholar]
- Stroke and cancer: The importance of cancer-associated hypercoagulation as a possible stroke etiology. Stroke. 2012;43:3029-34.
- [Google Scholar]
- Corticosteroids in brain cancer patients: Benefits and pitfalls. Expert Rev Clin Pharmacol. 2011;4:233-42.
- [Google Scholar]
- Dexamethasone for the prophylaxis of radiation-induced emesis: A National Cancer Institute of Canada Clinical Trials Group phase III study. J Clin Oncol. 2000;18:1960-6.
- [Google Scholar]
- The role of steroids in the management of brain metastases: A systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010;96:103-14.
- [Google Scholar]
- Evidence-based treatment of delirium in patients with cancer. J Clin Oncol. 2012;30:1206-14.
- [Google Scholar]
- Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. N Engl J Med. 2016;375:134-42.
- [Google Scholar]
- Effect of haloperidol on the development of the solid ehrlich tumor in mice. Life Sci. 1997;60:PL69-74.
- [Google Scholar]
- Penfluridol: An antipsychotic agent suppresses metastatic tumor growth in triple-negative breast cancer by inhibiting integrin signaling axis. Cancer Res. 2016;76:877-90.
- [Google Scholar]
- Anti-tumor effects of penfluridol through dysregulation of cholesterol homeostasis. Asian Pac J Cancer Prev. 2014;15:489-94.
- [Google Scholar]
- Rapid tranquilization for agitated patients in emergency psychiatric rooms: A randomized trial of olanzapine, ziprasidone, haloperidol plus promethazine, haloperidol plus midazolam and haloperidol alone. Rev Bras Psiquiatr. 2011;33:30-9.
- [Google Scholar]
- Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: A randomized, double-blind, placebo-controlled trial. Neuro Oncol. 2013;15:1429-37.
- [Google Scholar]
- Whole brain radiotherapy for brain metastasis. Surg Neurol Int. 2013;4(Suppl 4):S236-44.
- [Google Scholar]






