Translate this page into:
The Development of the Community-based Palliative Care Model in a District Health System, Phitsanulok Province, Thailand
Address for correspondence: Dr. Nithra Kitreerawutiwong, Faculty of Public Health, Naresuan University, Phitsanulok 65000, Thailand. E-mail: nithrakm@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Palliative care (PC) refers to a set of basic health services in Thailand and is in the early stage of implementation.
Aim:
The aim of this study is to develop a community-based PC model in a district health system (DHS) based on the form of action and evaluation.
Methods:
A three-step action research: look, think, and act was designed with mixed methods of data collection.
Results:
A key finding was the confusion on the terminology of the PC, challenge of the referral system of PC patients in DHS, medical equipment and supplies for the PC patients, and insufficient access to opioid analgesics at home. The model of development comprised the training of health professionals, the management of the medical equipment and supplies by people sector, and the development of a referral guideline of the PC patient in DHS. The evaluation showed the higher score of the accessibility to PC than the score of accommodation for patients. It also showed the higher score of the care continuity over the longitudinal continuity for patients. For the carers, the score of guilt is higher than the score of the care burden.
Conclusions:
A community-based PC model should be monitored by district health managment. The methods of this study are expected to be useful advice on how to solve similar problems in the other regions of similar context.
Keywords
Action research
community-based palliative care
district health system
Thailand
INTRODUCTION
The rapid increase of aging population and epidemiologic transition consequence to enlarge life-limiting diseases across the world have growing need for palliative care (PC) development.[12] The World Health Organization (WHO) and the Worldwide Hospice and PC Alliance (WHPCA) promote activities, monitor progresses, and provide resources on education and policy to many countries in order to develop PC.[345] Each year, approximately 20-million people rely on the end stage of their lives with PC, including 6% who are children. These numbers are mere low estimation because, in fact, around 20 million or higher require PC in their years before death. In many countries, opioid analgesics are not available or accessible to the majority of patients suffering moderate-to-severe pain which is one of the sufferings at the end stage of life.[6] In line with Reville and Foxwell,[7] one-third of people with serious to terminal illness of the world has no access to PC.
The WHO[8] defines PC as “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial, and spiritual.” This definition includes the provision of PC for people who have other chronic diseases who need PC services in the early stage of the disease trajectory[9] and support the family caregiver throughout the care process and provides bereavement services to family members after the patient's death[1011] rather than traditional concepts of PC as the end-of-life care for cancer patients. Hence, PC should be integrated with other chronic illnesses across the variety of settings to serve the needs of patients.
Thailand was classified in the third category by WHPCA which is the isolated provision of PC services. The category is characterized by the development of PC activism that is patchy in scope and not well supported; source of funding that is often heavily donor dependent; limited availability of morphine; and a small number of hospice – PC services that are often home based in nature and limited in relation to the size of the population.[12] In addition, the Economist Intelligence Unit has devise the quality of death index to rank the availability, affordability, and quality of end-of-life care in 80 countries, and this ranking shows that Thailand is ranked in the 44 with the score of Death index of 40.2.[13] However, Thailand has attempted to improve the PC services.
In Thailand, the National Health Act B. E. 2550 (A. D. 2007), Section 12 indicates that “a person has the right to make a living will in writing to refuse the medical treatment or other health-related services which are provided merely to prolong his/her terminal stage of life or to make a living will to refuse the service to cease the severe suffering from illness.” The living should be carried out in accordance with the guideline under the Ministry of Public Health (MOPH). Although most patients passed away at home, PC at home is limited.[14] Most services of the PC are provided at tertiary hospitals and cancer centers by public facilities, private hospitals, and faith-based institutions.[15] Therefore, the services are not in concordance with the concept of PC that covers bereavement services.
In the year 2014, The MOPH, Thailand, announced PC Policy to provide quality service coverage for the whole country.[16] Then, in the year 2015, the National Health Security Office (NHSO) supported the network services on PC provision of 61 district health system (DHS) networks with the budgetary of 135,000 baht/network/year.[17] Moreover, in the year 2016, Thailand PC Policy was expanded to subdistrict health-promoting hospital (previously called health center) and homes. Moreover, PC was determined in service plan in B. E. 2560–2564 (A. D. 2017–2021) under the MOPH. PC services were translated into practice in DHS. DHS provides health services to population in a district to improve health and quality of life through collaborative working with local organizations and other stakeholders in the community.[18] In accordance with the WHO, PC strategies should be combined with primary care and public health services in the community[19] and should be adopted by all stakeholders of the same community, not just by professionals specializing in PC.[20]
Regardless of the level of development, challenges related to PC in Thailand include the PC that has not been recognized, poor access to pain medications in the community,[21] limitation of community- and home-based PCs, and inadequate training for health-care personnel and volunteer for patients,[15] and the inappropriate management of the referral system from hospital to home to assure continuity of care.[22] As consonant with the barriers that were found in the country in Southeast Asia which were mapped out the development of PC in category 3 is the isolated provision of palliative. The barriers were drug availability and fear of using opioids among public as well medical practitioners and misconception regarding the role and concept of PC among health-care professionals.[23] To effectively develop the PC in community with many challenges based on the support from National Health Act and PC Policy, community-based PC needs to be designed.
Community-based PC means that PC service was integrated into DHS. This type of services requires a strong network of organization in the district. It is in line with group 4 of the preliminary integration PC into national health system which is characterized by the development of a critical mass of PC in a number of locations, a variety of PC providers and types of services, awareness of PC on the part of health professionals and local communities, the availability of morphine and some other strong pain-relieving drugs, limited impact of PC on policy, the provision of training and education initiatives by a range of organizations, and existence of a national PC association.[12] The WHO suggests that the public health model for PC is needed to translate a concept of PC including policy, drug availability, education, and implementation for population by cooperating with the community.[19] PC delivered by DHS has the advantage of providing better access and continuity, and decrease burden for caregiver. Therefore, this concept was applied to fill the gap of PC in a DHS of this study.
Objectives
The aim of this study is to develop a community-based PC model in a DHS.
METHODS
This study applied action research, a methodology that is built from the involvement of the stakeholders in the context to improve a situation by empowering them. This approach emphasizes on community participation to ensure a broader contribution to social sciences and social change.[24] The role of the researcher is to be a facilitator who assists stakeholders in clearly defining their problems and to support them to work for effective solutions toward the issues that concerning PC. Stakeholders were patients and families undergoing PC, health professionals, and social workers in the district. Data collection were from both quantitative and qualitative data. Action research is often described as a process involving three phases: look, think, and act. The look phase is about defining the problem. The think phase involves interpreting and analyzing the issues. The act phase is about planning, implement, and evaluation.[25] This paper presents an action to develop a community-based PC for people living in Phompiram district, Phitsanulok under Phompiram DHS. PC services regulated by National Health Act in B. E. 2550 (A. D. 2007) and determined in services plan in B. E. 2560–2564 (A. D. 2017–2021). Notwithstanding the existence of the regulation since the year 2007, the introduction of the PC is still in the early phase and is limited in translation into practice. Hence, it is essential to develop the appropriate intervention of the PC for this DHS through the collaboration with stakeholders in DHS to enhance participation in the health care and to increase the chance of success.
Setting
This study was conducted in Phompiram DHS, covering the community hospital (CH) located in one province of lower northern region, Thailand. This hospital acted as a contracting unit for the primary care and a contracting unit for the secondary care. These two units worked together through the referral system with 19 subdistrict health-promoting hospitals, which provided primary care facilities, and these two units shared resources for the primary care in the district. The proportion of the elderly in this district was 14.7% out of the whole population that was in the aging society.[26] The CH had developed a PC guideline to effectively provide PC in the hospital. In addition, CH provided a training program regarding long-term care to health professionals (a care manager) and volunteer lay caregiver (a caregiver) for the dependent elderly patients, such as homebound, bedridden, and patient at the final stage of cancer at home according to the NHSO manual.[27] The care manager needed the information of the patient in the district who required long-term care services. Then, he/she would manage home care service plan for a caregiver to take care of the patient through home visits. A total of 10 formal caregivers were trained for 72 h and 2 care managers were for 70 h.[26] However, the efficiency of the training needs to be examined for the transfer of learning into action in the community.
Design
Three phases: look, think, and act, was employed from Stringer.[25] Two focus-group discussions (FGDs) were carried out in the look phase to identify the problem and organize the PC information. In the think phase, a FGD 2 was performed to identify the action to be implemented. In the act phase, the plan was implemented and evaluated for its accessibility, continuity of care from patient side, and burden of caring from family caregiver side. In the evaluation process of the act phases, a non-one-group posttest only was employed. In this study, there was no control group since the data collection was done for a long period which might affect the internal validity of the intervention and maturation. This change might occur due to the change in skill and experience of the participants. Another limitation is the use of the only posttest as there was no internal and external validity test. The test was considered as the reduction of functional interference in PC for patients and carers. In spite of these limitations, this research design is appropriate to action research as its philosophical premise is not related to the positivism of the testing. As the action research concepts were dialogue, participation, and reflection on norms and values,[28] a nonequivalent posttest only was used in evaluating the development of collaborative PC services in DHS.
Participants
Participants in phase 1 and 2 were the key informants who involved in PC services in the district. The number of participants for each FGD was 8–10. The first group was health professionals who were responsible for PC including a physician, a pharmacist, three nurses, three public health professionals, a Thai traditional medicine, and a physiotherapist. The second group comprised four formal caregivers, two family caregivers, and two representatives of the local organization. Purposive sampling was used to select the participants. The criterion of participant for FGD 1 was being health professional who was responsible for PC for at least 2 years to ensure sufficient experience to share among the discussion and who was willing to participate. For the participant selection of FGD 2, the key informant was determined by being the layperson and the representative of the local organization of the people in this district, had experience in taking care of the homebound and bedridden patients at home for at least two years and was willing to take part. The number of patients in FGD 1 was 8 whereas that in FGD 2 was 10. Participants in phase 3 were 41 homebound and bedridden patients since the coding Z515 was no evident, and 41 family caregivers who received home PC service in DHS.
Data collection
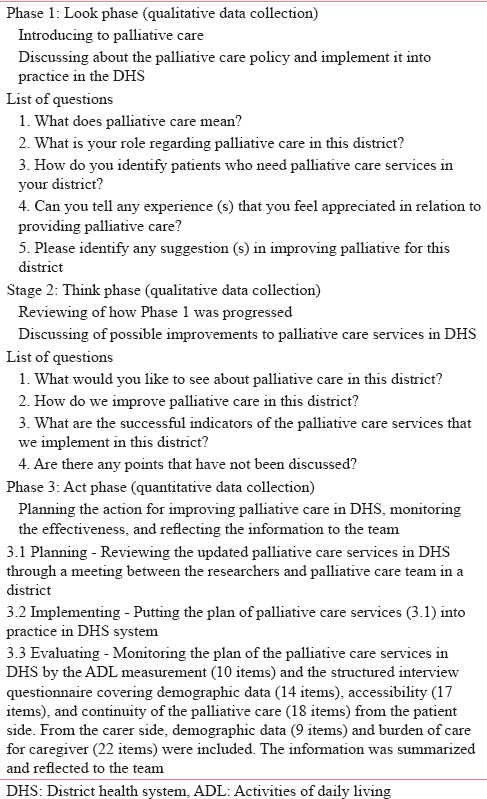
Data collection was undertaken in three phases. Phase 1: look, two FGDs were conducted with 8–10 participants through the purposive sampling mentioned above. The participant who met the eligibility criteria were invited through personal contact by one of the researchers. FGDs were carried out at a meeting room at Phrompiram hospital. The moderator was the first author who led the discussion, kept the conversation flowing, asked probing questions, took notes for comments that might be essential later, and summed up the main points. The assistant moderator was the second author who took comprehensive notes, operated the voice recorder, and kept track of time. The third author controlled the meeting atmosphere and logistics and responded to unexpected interruptions. Phase 2: think, the other two FGDs with the same participants from phase 1 were carried out. The moderator reviewed the topic and summarized the result from phase 1 to participants. This phase was intended to develop an action plan to improve the PC. The discussion encouraged participants to share their points of views according to the discipline and role of DHS. In this phase, the conclusion regarding the action plan from the group discussions was reached. Phase 3: act, the conclusion of the action plan was the input for the plan regarding the project or activity in improving the PC services. The researcher and the PC team had a meeting to set the tasks. Then, project and activity were implemented. Finally, the evaluation phase, the accessibility and continuity from the patient side, and burden of care from the carer side were investigated. The evaluation was related to the dimension of the burden of care for carers and accessibility, continuity for PC patients.[29] Before data collection, the Naresuan University Institutional Review Board approved the ethics of this study (COA no. 518/2016, IRB no. 772/59). The researcher explained the purpose of the study through the information sheet and clarified the questions. The participants voluntarily took part in this study as they signed the consent form before joining in the activities.
Instrument
The research instruments of each phase were developed. The semi-structured interview was employed in Phase 1 and Phase 2. The questions in the Phase 1 focused on assessing the situation of PC in DHS. The queries for Phase 2 focused on structural analysis of the situation from Phase 1. As phase 3 focused on planning, implementing, the action, and the evaluation of the action comprised 10 items of activities of daily living (ADL) measurement proposed by Katz et al.[30] which is the structured interview questionnaire. In addition, the instrument of patient side included 14 items of demographic data, 17 items of accessibility, and 18 items of continuity of PC. For carer side, 9 items of demographic data and 22 items of burden of care were used. Table 1 shows the activities and questions of the three phases.
The 10-item ADL measurement comprised eating, dressing, indoor mobility, bathing, using the toilet, and continence. The questionnaire of patients regarding demographic data included sex, age, marital status, education, occupation, income, health services utilization, health insurance scheme, comorbidity, received treatment, blood pressure, relationship between them and the carers, method to go to facility, and the number of received home visits. The accessibility part included five domains of availability, accessibility, accommodation, affordability, and acceptability[31] with 5-point Likert scale items with 1 (strong inaccessibility) to 5 (strong accessibility). The continuity of PC instrument adopted from Gulliford et al.[32] consisting of four dimensions of longitudinal continuity, flexible continuity, relational continuity, and team and cross-boundary continuity on a 5-point Likert scale. For the carer side, demographic data were sex, age, marital status, education, occupation, income, comorbidity, received treatment, and relationship between them and the patients. Twenty-two items for the burden of care for caregivers adapted from Toonsiri et al.[33] which comprised four dimensions: personal strain, privacy conflict, guilt, and uncertain attitude on a 5-point Likert scale response from 0 (never) to 4 (nearly always). The higher burden of care scores indicate the greater the burden.
Validity and trustworthiness
Trustworthiness was conducted in Phase 1 and 2. To validate data through multiple perspectives of the people who involved in this phenomenon, the triangulation of person data was carried out by gathering data from different groups of people including health professionals, formal caregivers, family caregivers, and representatives of the local organization. Verbatim quotations were illustrated to establish the credibility of the prominent themes and to ensure the meanings and feelings of the participants.[34] Thick description of the process in this situation for promoting credibility was formulated. The information of this study was provided to enable the reader to make the transferability judgments.[35]
The validity and reliability of the instrument in Phase 3 were conducted for the accessibility, the continuity of PC, and the burden of care for caregiver. The three instruments were validated by applying an item content validity index (I-CVI) with five experts, obtained I-CVI scores were 0.98, 0.98, and 0.99, respectively. The pilot testing to assess reliability was performed using Cronbach's alpha coefficients of accessibility, continuity of PC, and the burden of care for caregiver, obtaining 0.86, 0.76, and 0.82, respectively.
Data analysis
As phase 1 and 2 used qualitative data collection method, a process of content analysis was undertaken. The discussions were transcribed verbatim. The data from interview were coded to describe all aspects of the content.[36] The researchers separately analyzed the transcript through the codes. Then, the meeting of the researchers was held to discuss the themes until the consensus was reached.
In Phase 3, quantitative data collection method was conducted. Descriptive statistics were used to describe the demographic data, including means, standard deviations (SDs), percentages, and ranges. For ADL score, out of 20 points, the score higher than or equal to 12 means “fully independent;” the score between 5 and 11 means homebound; and the score between 0 and 4 means bedridden requiring complete assistance. The accessibility, continuity of PC, and burden of care for caregiver were compared through their mean scores of the three scales to determine the cutoff acceptable level.
RESULTS
As the action research cycle comprised three phases: (1) look, (2) think, and (3) act, the results from these three phases are presented as follows.
Look phase: the situation of palliative care services in a district health system
The themes that were emerged during the look phase were as follows: confusion about the terminology of the PC, challenge of the referral system of the PC patients in DHS, medical equipment and supplies for the PC service, and insufficient access to opioid analgesics at home.
Confusion about the terminology of the palliative care
Participants were confused about terminology regarding the PC. The diagnosis for patients who needed PC services in DHS is rare. In addition, the health-care providers did not have sufficient skill in using the Palliative Performance Scale (PPS).
“At the ward, the physician will diagnose according to ICD-10 and evaluate according to PPS.” (NU1)
“In the home visit, we used ADL to assess the clients. If the client gets ADL score of 0–4, it suggests that this client requires complete assistance of the PC service or who is at the final stage of cancer.” (PH 3)
“I think that some health-care providers who work at a subdistrict health-promoting hospital (previously called health center), nurses and public health staff did not recognize PPS.” (PH 2)
“When I visit the patient at home, I use PPS to assess the patient whether he/she needs PC and then provide the supportive care according to the symptoms.” (PH 1)
“The patient who requires PC is the patient with cancer who is diagnosed to be in the last stage of cancer – there is no way to improve his/her condition.” (FCG2)
“Most diagnoses encode the illness which is the main symptoms being cured. The assigning of the code Z515 of the PC is still rare.” (PHY1)
“Many physicians work at the CH to pay off their studying funding around three years. Then, they will pursue their study as specialists. Due to this high turnover rate of the physicians at the hospital, there is no continuity of the PC development.” (NU1)
Challenge of referral system of palliative care patients in district health system
In general, the patients are referred from the CH to the subdistrict health-promoting hospital according to the individual discharge plan. However, the referral system from the subdistrict health-promoting hospital to the CH is still unsystematic.
“The patients who require PC services will be taken care at the CH. Then, they will be referred to the primary care facility (subdistrict health-promoting hospital). However, for the patients in the community, the subdistrict health-promoting hospital will assess the need for the PC for the patients in the community. The patients will be looked after according to their main symptoms and condition at this hospital. The patients will not be referred to other hospital nor diagnose with the code Z515 with the CH. They will be referred to the CH only when their symptoms are complex.” (NU1)
“For the patient who is diagnosed at the CH that he/she requires PC serve, he/she will be discharged by the multidisciplinary team to be referred to the subdistrict health-promoting hospital. On the other hand, for the patient that the subdistrict health-promoting hospital assesses the symptoms from PPS at PC patient's home, the CH might not have the information as it is with the subdistrict health-promoting hospital.” (NU2)
“If we (the health-care provider who worked in subdistrict health-promoting hospital) assess the patients by PPS and ADL and found that they are bedridden or at the last stage of cancer, we will provide the care services according to the symptoms and as the information recorded at the subdistrict health-promoting hospital.” (PHY1)
“The caregiver will visit the patients according to the plan of the public health officer, then complete the form, and to be given to the health-care provider.” (FCG2)
Medical equipment and supplies for the palliative care patients
The temple is the place of donation and the storage of the medical equipment and the service materials for the PC patients in the community. The process of loaning these medical devices was done by the volunteer who is the leader of the community. He/she will create an account of borrowing and returning the medical equipment.
“Generous people donate air mattresses, oxygen generator, and suction to the hospital. The district health management team set a meeting to reach the consensus that the donation of medical equipment and medical supplies was done at the temple such as pampers and set dressing should be supplied at the temple. The advantage of storing the equipment at the temple is it is free of charge. If they are at the hospital, the borrower will pay 20,000 baht for the deposit resulting in the difficulty in borrowing for poor people.” (NU3)
“The temple has a community-developing monk, whose name is …. He is the monk that people trusted and was trained as a caregiver. He was one of the multidisciplinary team who visited patients at their last stages of lives. The record of the borrowing-returning account was done in the notebook at the temple by the volunteer.” (CG2)
“Subdistrict administrators usually provide home visit with the multidisciplinary team. For patients with financial problem, the local organization will provide living supplies based on patient's need, such as diapers, wound dressing set, tissue papers, and so on.” (LO1)
Insufficient access to opioid analgesics at home
The NHSO provides the fund to allocate morphine treatment for the patients with cancer at the last stage for the PC at the community or at home according to the clinical and morphine use practice. In addition, in October 2017, Phrompiram Community Health Fund provided a syringe driver to support the PC in the community. However, there is no guideline for morphine management to be used in the community/at home. Health-care providers at primary care level were not received the training regarding the PC service for patients who received morphine in the community/at home.
“In October 2017, a patient with the final stage of cancer who needed the PC service was referred from Buddhachinaraj Hospital (Tertiary level) to Phompiram hospital (Secondary level). The patient asked to be treated at home. Therefore, Phompiram hospital referred him/her to the subdistrict health-promoting hospital (Primary care level). The patient was prescribed to have morphine at home; however, the health-care provider at primary care level did not know how to use the syringe driver.” (NU1)
“Prescribing morphine to be used at home is new for this DHS. I am concerned about the drug abuse; therefore, this DHS does not prescribe morphine to be used in the community/at home. We need to set a guideline first.” (PHAR1)
“If the patient uses morphine at home by the syringe driver, his/her carer cannot control the equipment. What would happen if some other people use this morphine abusively?” (TTM1)
Think phase: insights of improvement of palliative care services in a district health system
The results from the look phase promoted the discussion on the improvement of the PC service in DHS. The participants proposed the areas to be improved including training of the health professionals, managing medical equipment and supplies by people sector, and developing a referral guideline of PC patient in DHS as shown in Table 2.

Act phase: translating the planning into practice
The theme of the improvement on the PC services in DHS was planned and implemented in this phase. After implementing the activities for 6 months, the evaluation was set to monitor both patients and informal carers. For the patients, the evaluation was focused on accessibility and continuity of the PC whereas for the carers, the appraisal was focused on the burden of care.
51.2% of 41 PC patients in DHS had ADL score of 0–4 whereas 48.8% of them had 5–11 points. According to the long-term care guideline, the ADL score 0–4 points is called bedridden and that of 5–11 points is called homebound. The patients in the two groups were diagnosed as having the following: 11 had stroke; 14 had cancer; 9 had obstructive pulmonary disease; 2 had health failure; and 5 had dementia. These are medical conditions associated with substantial palliative symptom burden.
The majority of patients were female (63.4%) aged 60 years or older (70.7%). 54% were single, window, divorce, and separate. 65.9% had universal coverage scheme and 24.4% had civil servant medical beneficial scheme. Most participants (66.7%) went to the facility by their own cars. The average number of participants visiting the subdistrict health promotion hospital per year was 2.24 times (SD = 2.68). The average number of participants visiting the CH per year was 5.81 times (SD = 4.41), whereas the average number of patients received home visit per year was 2.40 times (SD = 1.95). Most caregivers were female (70.7%), with age less than 60 years. 63% of the carers were married. Out of all carers, 56% were the patients' children; 32% were spouse; 8% were in-laws; and 4% were siblings. 68% were educated until primary school and 58.6% were employed.
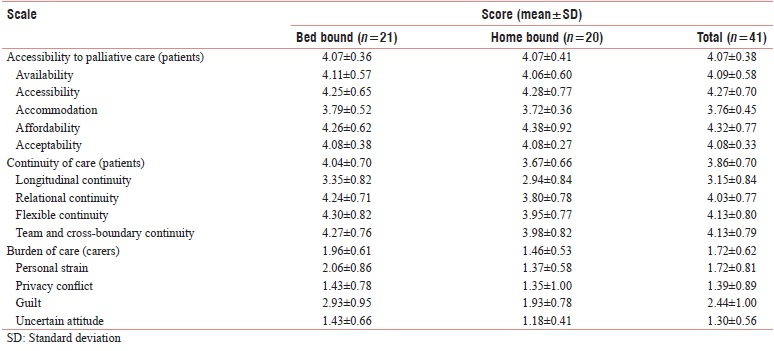
The total score of the accommodation (3.76 ± 0.45) is lower than the total mean of accessibility to PC (4.07 ± 0.38). The total score of longitudinal continuity (3.15 ± 0.84) is lower than the total score of the care continuity (3.86 ± 0.70). For the carers, the total score of guilt (2.44 ± 1.00) is higher than the total score of burden of care (1.72 ± 0.62). The details of the total scores are in Table 3.
DISCUSSION
The results from this study in the look phase showed that the confusion in terminology of the PC and the reluctance to refer PC patients in DHS resulted in the insufficient access to opioid analgesics at home. This information suggests that Thailand is in the early stage of the PC development. At the macro level, the National Health Act in B. E. 2550 (A. D. 2007) was enacted; PC Policy was launched by MOPH and the extra fund for caring PC patient who diagnosed with the code Z515 was provided by NHSO.[14] The number of the diagnosis with the code Z515 in cancer patients was 1.7 × 10−3 for both in- and outpatients which is the very low prevalence of coding Z515 use. Without code Z515, many patients were not able to access to the PC services.[37] The study of Suvarnabhumi et al.[38] indicated that the lack of knowledge in PC in medical students in Thailand lowered confidence to practice PC. Furthermore, Hannaon[39] indicated that the barriers in accessing to opioid medications were the lack of infrastructure to store and distribute them, inadequate training of health-care professionals, and insufficient regular control relating to the abusive use. These situations led to the development of the understanding of the PC services in DHS.
The development of PC services was focused on the training of the health professionals, managing medical equipment and supplies by people sector, and developing a referral guideline of PC patient in DHS. This development is in accordance with the building blocks of the WHO regarding health workforce, service delivery, and medical equipment.[40] It is also in line with Kim et al.[41] described the development process of the community-based PC model in Busan, Korea that they developed the provision of PC, established the supportive system, improved personal capacity, developed the education and promotional program, and established the assessment system to improve quality. In addition, this study found the role of monk who was trained to be caregiver to manage medical equipment and medical supplies and provides home visit with health-care professionals. This situation occurred because Thailand implemented DHS since 2012 in mobilizing resource and promoted the collaboration between DHS and the other sectors in the district to improve the population health.[18] Therefore, the PC services were designed by engaging the partnership with other sector (temple), in community to achieve the goal of the team. The referral guideline of the PC for patients was developed to bridge the PC services in DHS from home-based to community-based. In this study, the team developed the referral guideline of PC patients in DHS for four months. The referral system was consistent with Ansari et al.[42] indicating that the referral system is the most important pillar of the first level PC, which satisfies the patients' needs with a small cost, and if possible, leads them to the higher levels of the service resulting in the continuity of care.
The total score of accommodation (3.76 ± 0.45) is lower than the total mean of the accessibility to PC (4.07 ± 0.38). When considering on the items, it was found that the process of services was complex due to the long-waiting time and inconvenience. The patients who required PC services had discomfort symptom; therefore, they should receive the care within a short time. This item was consistent with the patients' perceptions of the PC scale that the dimension of physical-technical condition which included the item of access to help, food, and equipment receive an average score of 3.51 (SD. = 0.58) on the 4-point Likert scale.[43]
The total score of longitudinal continuity (3.15 ± 0.84) is lower than the total score of the care continuity (3.86 ± 0.70). Longitudinal continuity of the care refers to an ongoing pattern of the health-care interaction that occurs in the same place, with the same medical record, and with similar professionals; hence, care providers should gain more knowledge in providing the care to the patients. Longitudinal continuity is a key feature in a pattern of visits.[44] In this present study, longitudinal continuity of the care in the PC is a pattern of visiting the provider at the primary and secondary care facilities. The lower score than the mean score is due to the visit of the patients at the primary care facility. As this facility provided home visit, patients had no necessity to go to the care facility of the secondary care. If the patients required the medical equipment, the health-care provider would suggest appropriate usage and monitor by home visit so that the patients could get the medical equipment to be used at home by borrowing the medical equipment from the temple. In agreement with the WHO, the PC services should be combined with the primary care in the communities.[19]
The lack of explicit attention to caregivers is a serious gap in health care. The caregivers are hidden patients themselves, with serious adverse physical and mental health and financial hardship.[45] The study of Naoki et al.[46] found that caregiver burden had a strong negative correlation to family satisfaction with end-of-life care (Spearman's rho [ρ] = −0.560, P = 0.005). Understanding and reducing the burden on the caregiver contributes to maintaining or enhancing the quality of life of people. For the carers, the total score of guilt (2.44 ± 1.00) is higher than the total score of burden of care (1.72 ± 0.62), suggesting the need for improved of this aspect. In line with the study of Chindaprasirt et al.,[47] the guilt was the highest score of burden of care. The items regarding guilt, such as feeling suggesting that he/she should be doing a better job in taking care of the patient. However, for Thai culture, taking care of the parents is mandatory according to the Buddhist doctrine. The result was contradictory to the study of Galvin et al.[48] reporting that guilt was the third factor after the role strain and personal strain among caregivers in Amyotrophic Lateral Sclerosis in Dublin. Due to this cultural difference, the result of this study might not be directly comparable to that of the other study.
This study applied action research based on the democratic paradigm to the development of the PC to ensure that the process reflects the participation of all sectors in DHS. The approach started with the understanding of the situation, interpreting the situation, and establishing the intervention to improve the context. In addition, the evaluation was conducted to judge the value and provide the suggestions for the improvement. There are some limitations in this present study. As the study was carried out in one DHS, the results might not be generalized to all DHS. However, the research methods of this study might be useful in terms of being a guideline on how to solve similar problems in the other areas of similar context.
CONCLUSIONS
The findings of this study are expected to develop the understanding of the health-care providers toward the PC in DHS with the action and evaluation of the model designed. District health management team should monitor the coding diagnosis of PC, manage opioid in community, promote the PC services to achieve accessibility and continuity, and decrease burden of care for carer. For the long-term development, a call of the financial support system, the information center, and the leadership in DHS need to be considered to cover all the dimension of the health system.
Financial support and sponsorship
This study was financially supported by the National Research Council of Thailand in the year 2017 (Grant No. R2560B114).
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Strengthening of palliative care as a component of integrated treatment throughout the life course. J Pain Palliat Care Pharmacother. 2014;28:130-4.
- [Google Scholar]
- 2014. Strengthening of Palliative Care as a Component of Integrated Treatment within the Continuum of Care. Available from: http://www.apps.who.int/iris/bitstream/10665/173012/1/B134_R7-en.pdf
- International progress in creating palliative medicine as a specialized discipline. In: Hanks G, Cherny NI, Christakis NA, eds. Oxford Textbook of Palliative Medicine. Oxford: Oxford University Press; 2010. p. :9-22.
- [Google Scholar]
- The Worldwide Hospice Palliative Care Alliance. 2015. Defining palliative care. Available from: http://www.thewhpca.org/resources/item/definging-palliative-care
- [Google Scholar]
- Cancer Control: Palliative Care. In: World Health Organization Guide for Effective Programmes. Geneva: World Health Organization; 2007.
- [Google Scholar]
- World Palliative Care Alliance. In: Global Atlas of Palliative Care at the End of Life. London: World Palliative Care Alliance; 2014.
- [Google Scholar]
- The global state of palliative care-progress and challenges in cancer care. Ann Palliat Med. 2014;3:129-38.
- [Google Scholar]
- 2002. WHO Definition of Palliative Care. Available from: http://www.who.int/cancer/palliative/definition/en/
- Guidelines for the psychosocial and bereavement support of family caregivers of palliative care patients. J Palliat Med. 2012;15:696-702.
- [Google Scholar]
- Increased access to palliative care and hospice services: Opportunities to improve value in health care. Milbank Q. 2011;89:343-80.
- [Google Scholar]
- Mapping levels of palliative care development: A global update. J Pain Symptom Manage. 2013;45:1094-106.
- [Google Scholar]
- The Economist Intelligence Unit. 2015. The 2015 Quality of Death Index Ranking palliative Care Across the World. Available from: https://www.eiuperspectives.economist.com/sites/default/files/2015%20EIU%20Quality%20of%20Death%20Index%20Oct%2029%20FINAL.pdf
- [Google Scholar]
- Status of End of Life Care in Thailand. 2006. UICC World Cancer Congress. Available from: https://2006.confex.com/uicc/uicc/techprogram/P10163.HTM
- [Google Scholar]
- Palliative care nursing interventions in thailand. J Transcult Nurs. 2013;24:332-9.
- [Google Scholar]
- 2017. Sustainable Palliative Care in Thailand. Available from: http://www.dms.moph.go.th/dmsweb/publish/publish12072017090710.pdf
- National Health Security Office. Palliative care at the end of life. Kaomai J. 2015;8:1-24.
- [Google Scholar]
- Driving District Health System in Thailand. Nonthaburi: Rural Doctor Foundation; 2014.
- The public health strategy for palliative care. J Pain Symptom Manage. 2007;33:486-93.
- [Google Scholar]
- Global Atlas of Palliative Care at the End of Life. 2014. Worldwide Palliative Care Alliance and World Health Organization. Available from: http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf
- [Google Scholar]
- 2016. Palliative Care Services in Thailand: Where are we now?. Available from: http://www.thaps.or.th/wp-content/uploads/2016/08/3-PC-services-in
- Linkage of palliative care from hospital to home in Northern Thailand. Int J Evid Based Healthc. 2016;14:S34.
- [Google Scholar]
- Action Research in Health. Upper Saddle River, NJ: Pearson Prentice-Hall; 2004.
- Action Research (3rd ed). London: Sage Publications; 2007.
- Phompiram District Health System. Annual Report 2016. Phitsanulok Phompiram District Health System 2017
- [Google Scholar]
- 2016. National Health Security Office. Long Term Care for Dependence Elderly in Universal Coverage Scheme and Financial Support in Budgetary Year; 2016. Available from: https://www.nhso.go.th/files/userfiles/file/2016/01%E0%B9%81%E0%B8%99%E0%B8%A7%E0%B8%97%E0%B8%B2%E0%B8%8759.pdf
- Participatory Research-Tradition, Theory and Practice. Karlstad: Karlstad University Studies; 2001.
- Asystematic review of measures of end-of-life care and its outcomes. Health Serv Res. 2007;42:1848-70.
- [Google Scholar]
- Studies of illness in the aged. The index of adl: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914-9.
- [Google Scholar]
- The concept of access: Definition and relationship to consumer satisfaction. Med Care. 1981;19:127-40.
- [Google Scholar]
- Measuring continuity of care in diabetes mellitus: An experience-based measure. Ann Fam Med. 2006;4:548-55.
- [Google Scholar]
- Development of the burden interview for caregivers of patients with chronic illness. 2011;4:62-75.
- Qualitative Research in Nursing and Healthcare (4th ed). Oxford: John Wiley & Sons, Ltd.; 2016.
- Competing paradigms in qualitative research. In: Denzin NK, Lincoln YS, eds. Handbook of Qualitative Research. Thousand Oaks: Sage Publications; 1994.
- [Google Scholar]
- Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277-88.
- [Google Scholar]
- Situational analysis of palliative care education in thai medical schools. Palliat Care. 2013;7:25-9.
- [Google Scholar]
- Provision of palliative care in low- and middle-income countries: Overcoming obstacles for effective treatment delivery. J Clin Oncol. 2016;34:62-8.
- [Google Scholar]
- Everybody Business: Strengthening Health Systems to Improve Health Outcomes: WHO's Framework for Action. Geneva: World Health Organization; 2007.
- Development of a community-based palliative care model for advance cancer patients in public health centers in busan, korea. Cancer Res Treat. 2017;49:559-68.
- [Google Scholar]
- Palliative care policy analysis in iran: A Conceptual model. Indian J Palliat Care. 2018;24:51-7.
- [Google Scholar]
- Patients' perceptions of palliative care: Adaptation of the quality from the patient's perspective instrument for use in palliative care, and description of patients' perceptions of care received. BMC Palliat Care. 2015;14:54.
- [Google Scholar]
- Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003;1:134-43.
- [Google Scholar]
- Supporting family caregivers in providing care. In: Hughes RG, ed. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008.
- [Google Scholar]
- Association between family satisfaction and caregiver burden in cancer patients receiving outreach palliative care at home. Palliat Support Care. 2018;16:260-8.
- [Google Scholar]
- Burdens among caregivers of older adults with advanced cancer and risk factors. Asian Pac J Cancer Prev. 2014;15:1643-8.
- [Google Scholar]
- Caregiving in ALS – a mixed methods approach to the study of Burden. BMC Palliative Care. 2016;15:81.
- [Google Scholar]






