Translate this page into:
The Palliative Care Information Act and Access to Palliative Care in Terminally ill Patients: A Retrospective Study
Address for correspondence: Dr. Kitty Victoria; E-mail: kev9011@nyp.org
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Studies have shown that over 50% of end-of-life discussions take place for the first time in the hospital and that terminally ill patients often have unrealistic views regarding the possible scope of treatment. The Palliative Care information Act (PCIA) was passed in an attempt to address the lack of access for terminally ill patients to palliative care services. A multi-database systematic review was performed on published studies from 2010 to present, and there were none found measuring the effectiveness of the PCIA.
Objectives:
We aimed to study the effect of the PCIA on access to palliative care services.
Methods:
We conducted a retrospective chart review of all terminally ill patients who died at Kingsbrook Jewish Medical Center from January 2010 to August 2013 in relation to passing of the PCIA.
Results:
Prelaw (prior to the law passing), 12.3% of the terminal patients received palliative care consults, 25% during the transition period (time between passing of law and when it came into effect) and 37.7% postlaw (after coming into effect) (P < 0.001).
Conclusions:
Legislation can have a significant effect on terminally ill patient's access to palliative care services and can change the culture of a hospital to be more pro-palliative for the appropriate populations.
Keywords
Access to palliative care in terminal patients
End-of-life care
New York Palliative Care Law
Palliative Care Access Act
Palliative Care Information Act
INTRODUCTION
The majority of serious and terminally ill patients lack advanced directives.[1] Nearly, 90% of Americans would prefer to receive end-of-life care at home[2] and one-third of Americans die in the hospital, 20% of those in the Intensive Care Unit (ICU).[3] Recent studies have shown that over 50% of end-of-life discussions take place for the first time in the hospital rather than in the outpatient clinic setting with their primary doctor. Patients often have unrealistic views regarding the scope of treatments for which they are agreeing. In one study of patients with metastatic cancer, 69% of those with lung and 81% of those with advanced colo-rectal cancers were unaware that chemotherapy was palliative rather than curative.[4]
Data from the Medical Expenditure Panel Survey show that 64% of the health care spending is concentrated on 10% of the population with the majority of those patients having serious illness and much of the money spent toward end-of-life care. This amounts to a large part of what is driving up health care spending as intimately tied to patients not being given the information necessary to make informed decisions.
On February 9, 2011, “The Palliative Care Information Act” (PCIA) of New York became effective. A multi-database systematic review was performed on published studies from 2010 to present. We were not able to find any measuring the effectiveness of the PCIA or its effect on access to palliative care services for its target population, terminal patients. On the subject of the law itself, there have been a few reviews and editorials.
Review of the law
The attending health-care practitioner (one who has the primary responsibility for the care and treatment of the patient) must offer patients with a terminal condition (expected to cause death within 6 months) information and counseling about palliative care and end-of-life options appropriate to the patient. Some of the specific goals outlined in the law are to (1) ensure that patients are fully informed of the options available to them (2) empower patients to make choices consistent with their goals and beliefs and to optimize their quality of life.
Palliative Care is defined as, “Health-care treatment, including interdisciplinary end-of-life care and consultation with patients and family members to prevent or relieve pain and suffering and to enhance the patient's quality of life, including hospice care.”
If the health-care practitioner is not willing to provide counseling on treatment options including palliative care, then they must refer this responsibility to a qualified professional. The discussions are to include prognosis, risks versus benefits of treatment options, and options regarding pain and symptom management. Violators of the law can face up to $5000 fine for repeat offenders and up to $10,000 fine or 1 year imprisonment for willful violation.[5]
Purpose
The purpose of our study was to study the effect of the PCIA law on the access to and utilization of palliative care services by terminal patients at a Brooklyn community hospital, Kingsbrook Jewish Medical Center (KJMC). A public opinion poll carried out by the Center to Advance Palliative Care and the American Cancer Society showed that majority of patients needed palliative care if they knew of its existence.[6] In another study of patients with late-stage cancer, over 60% of patients were identified as having an interest in palliative care services; however, they were only willing to proceed if suggested by their primary oncologist.[7]
We look at the number of palliative care consults in relation to the law as an indicator of physicians being compliant with the PCIA law, as it is implied from previous studies that when patients have accurate information about palliative care, the majority feel they would benefit.
METHODS
Eligibility
The study included all patients who had a terminal diagnosis and expired at KJMC prior to the passing of the law (January to August 12, 2010), between the law being passed and going into effect (August 13, 2010 to February 8, 2011), the year following the law going into effect (February 9, 2011 to February 8, 2012), and a follow-up year of the whole of 2013.
Quality assurance data
Mortality data files were obtained through the quality assurance department from their annually generated reports. The information available via the mortality reports included age, medical record number, sex, date admitted, date expired, terminal diagnosis, cause of death, and attending physician. The data acquired here were supplemented with data extracted from chart review including details of end-of-life discussions, discussions of advanced directives, and palliative care consults.
Study design
We used a data collection tool to go through each patient's chart and identify charts with palliative care consults. The data was organized into the previously noted time periods as to compare our results in relation to the law. During the time between when the law was passed and took effect, there were in-services given to administration, faculty, house staff, and nursing, around the meaning of the law and the importance of compliance given by the director of palliative care services. A hospital-wide memo was also sent to all physicians and hospital staff to make them aware of the law in addition to links for further reading online.
Our palliative care team comprised a board-certified pain and palliative care physician and a registered nurse specialized in palliative medicine. Our consult service used the Medical Orders for Life-Sustaining Treatment form, almost exclusively in documenting patient's preferences. Our team had a standard procedure for every consult, in that, prior to speaking with patients or their families, we would meet with all the concerned medical teams to understand what treatments were and were not being offered. We would, in this way, have the ability to thoroughly go over treatment options, palliative care and hospice, pain management, and advanced directives with every patient and family.
Statistical analysis
Comparison between palliative groups was assessed with Fisher's exact test for categorical variables and t-test for continuous variables. All statistical tests were two-sided with a test level of 0.05 used in assessing significance. All analyses were conducted using R, version 3.22 (R Core Team (2015). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/).
RESULTS
Sample characteristics
There were 754 total patients surveyed whom had expired in the hospital during the previously mentioned time periods and also had a terminal diagnosis at the time of death. There were 171 patients studied during the “pre-law” period from January 1, 2010 to August 12, 2010, 163 patients during the “transition” period from August 13, 2010 to February 8, 2011, 324 patients during the year following the law going into effect from February 9, 2011 to February 8, 2012, and 96 patients in the follow-up year of 2013. Out of all patient charts reviewed during the four periods, 70.6% did not and 29.4% of patients did have palliative care consults. Of the total patients whom had consults, the patients’ stated terminal diagnoses were 34.9% respiratory failure, 42.9% sepsis, 17.9% cancer, and 10.4% end-stage renal disease. From this same group, 56.1% were females and 43.9% were males. In relationship to location at time of death, from the palliative consult group, 46.2% were on the regular floor, 27.8% in the coronary care unit, and 25.9% in the ICU [Figure 1].

- Study population characteristics
Outcomes
We found statistically significant differences in the number of patients with palliative care consults between all times periods with the largest percentage being during the postanalysis year. Out of all patients reviewed who had palliative care consults, 12.3% were in the prelaw period, 25% were in the transition, 37.7% in the postanalysis year, and 25% in the follow-up year [Figure 2]. In addition, we found that 30% of all patients during all time periods had no discussion documented regarding advanced directives or palliative care. Within the patients who had no documented advanced directives discussion, 95.6% also did not have a palliative consult. Patients with palliative care consults were much less likely to have had a resident or attending document discussion of advanced directives in the chart, whereas of the patients who had not had a palliative care consult, the opposite was true. In the palliative consult group, 17.5% had a resident and 15.6% had an attending physician also documenting advanced directives, whereas, in the no palliative consult group, 32% had a resident and 24% had an attending with the same.
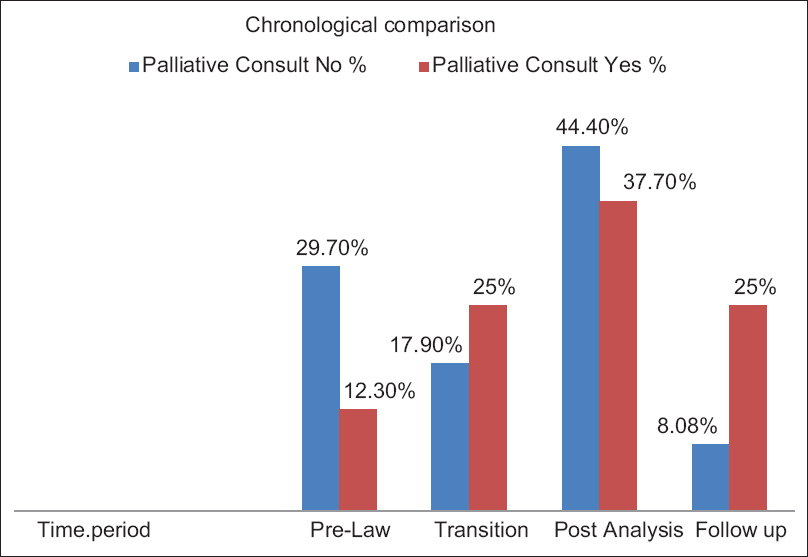
- Chronological comparison, in relation to passing of the law, of percentage of patients receiving palliative care consults in the total discussion group
DISCUSSION
The PCIA and now more recent Palliative Care Access Act (PCAA) were passed in a reaction to studies like the landmark study published in the 2010 NEJM, showing that patients with terminal lung cancer referred to palliative care from the time of diagnosis, not only had greater quality of life with better moods and pain control, but also lived on an average of 3 months longer.[8] A 2011 survey by the Center to Advance Palliative Care found that once patients are provided the appropriate information regarding palliative care, 95% agreed that it was important to be educated about palliative care and 92% would consider it for a family member with serious illness.[9]
Both the PCIA and PCAA address overuse by increasing access to various forms of support, potentially underused therapies, and beneficial conversations. Chemotherapy,[10] radiation therapy,[11] feeding tubes, surgery,[12] nonbeneficial medications,[1314] and therapies at the end-of-life[1516] can have a potential for overuse. Levels for family distress[17] may rise while quality of life for patients may decrease[18] as the amount of life-sustaining treatments and interventions increases.
The majority of terminally ill patients do not want emergency life-sustaining interventions; however, often their physicians are not aware of their preferences.[19] Most patients nearing the end-of-life would rather die at home, but fail to ever document these wishes[20] and believe that quality of life in the seriously ill is paramount, even if that means a shorter life.[21]
In a review of the PCIA law by Dr. Beth Popp published in the 2013 American Medical Association Journal of Medical Ethics, she discusses the ways in the law falters as to not ensure the accuracy of information provided. She makes the point that the decision to enroll in hospice or utilize palliative care services is frequently based on the way in which the physician presents such options. Although the law does not specifically address these deficiencies, we can look at passing of this law in New York as an initial step toward patients gaining access to deserved care, having a law that changed access to palliative care in terminal patients from a personal preference of the primary attending to a patient right and tagged on penalties for not honoring this right.
CONCLUSIONS
We can surmise from the statistical data gathered that a combination of the passing of the PCIA law and the justification it gave to the proceeding educational interventions led by the director of palliative care services was the primary driving force behind the number of palliative consults in terminally ill patients at KJMC increasing by more than 50%. We also observe that if patients had a palliative consult, they were much less likely to have had a resident or consultant documenting any discussion pertaining to advanced directives. As the law states, if the primary care provider opts to not discuss these issues with patients, they may refer to another qualified professional, such as a palliative physician or NP, this outcome would be expected if practitioners were attempting to be complaint with the law. Although the number of palliative consults increased by greater than 50%, we see the overall percentage of patients without palliative care consults as 70.6% in a population of terminal patients, an unfortunately common finding among many US hospitals.
The PCIA and other such laws may serve as a means to justify allocation of resources and energy toward educating physicians and staff on the importance of palliative care and also as to what kinds of patients are entitled. We were able to find a statistically significant rise in the percentage of terminal patients with referrals to palliative consultation in correlation chronologically with the passing of the law. Although there have been many positive advances in the last decade in relation to chronically ill patients's access to palliative care, we still have a long road ahead and laws may act as part of a whole driving force towards change. Legislation can have significant effect on terminally ill patient's access to palliative care services and can change the culture of a hospital to be more pro-palliative for the appropriate populations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Research in Action Issue #12: Advance Care Planning: Preferences for Care at the End of Life. In: AHRQ Pub No. 03-0018. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ); 2003.
- [Google Scholar]
- 86% of Americans Believe that People with Terminal Illness Would Prefer to Receive End-of-life Care at Home. (2002 Harris Survey on End-of-Life Care) 2002
- [Google Scholar]
- on behalf of the Robert Wood Johnson Foundation ICU End-of-Life Peer Group. Use of intensive care at the end of life: An epidemiological study. Crit Care Med. 2004;32:638-43.
- [Google Scholar]
- Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med. 2012;367:1616-25.
- [Google Scholar]
- Palliative Care Information Act. NY Pub Health Laws. Ch. 331, Sec. 2997-c. Available from: http://www.health.ny.gov/professionals/patients/patient_rights/palliative_care/information_act.htm
- [Google Scholar]
- 2011. Center to Advance Palliative Care 2011 Public Opinion Research on Palliative Care. Available from: http://www.capc.org/tools-for-palliative-care-programs/marketing/public-opinion-research/2011-public-opinion-research-on-palliative-care.pdf
- Do patients with advanced cancer and unmet palliative care needs have an interest in receiving palliative care services? J Palliat Med. 2014;17:667-72.
- [Google Scholar]
- Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733-42.
- [Google Scholar]
- 2011. Center to Advance Palliative Care, 2011 Public Opinion Research on Palliative Care 3. Available from: http://www.capc.org/tools-for-palliative-care-programs/marketing/public-opinionresearch/2011-public-opinion-research-on-palliative-care.pdf
- Aggressiveness of cancer care near the end of life: Is it a quality-of-care issue? J Clin Oncol. 2008;26:3860-6.
- [Google Scholar]
- Radiation oncology quality: Aggressiveness of cancer care near the end of life. J Am Coll Radiol. 2012;9:199-202.
- [Google Scholar]
- Hospital characteristics associated with feeding tube placement in nursing home residents with advanced cognitive impairment. JAMA. 2010;303:544-50.
- [Google Scholar]
- Discontinuing medications: A novel approach for revising the prescribing stage of the medication-use process. J Am Geriatr Soc. 2008;56:1946-52.
- [Google Scholar]
- Discontinuing cardiovascular medications at the end of life: Lipid-lowering agents. J Palliat Med. 2005;8:876-81.
- [Google Scholar]
- The implications of regional variations in medicare spending. Part 1: The content, quality, and accessibility of care. Ann Intern Med. 2003;138:273-87.
- [Google Scholar]
- Enhancing physician-patient communication. Hematology Am Soc Hematol Educ Program. 2002;2002:464-83.
- [Google Scholar]
- Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665-73.
- [Google Scholar]
- Associations between palliative chemotherapy and adult cancer patients’ end of life care and place of death: Prospective cohort study. BMJ. 2014;348:g1219.
- [Google Scholar]
- Advance directives for seriously ill hospitalized patients: Effectiveness with the patient self-determination act and the SUPPORT intervention. SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatment. J Am Geriatr Soc. 1997;45:500-7.
- [Google Scholar]
- Pew Research Center 2006: Pew Research Center for the People and the Press. Strong Public Support for Right to Die: More Americans Discussing and Planning. 2006. End-of-Life Treatment. Telephone Survey of 1,500 Older Adults Conducted 9.27 November, 2005 Under the Direction of Princeton Survey Research Associates International. Available from: http://www.people-press.org/report/266/strong-public-support-for-right-to-die
- [Google Scholar]
- Regence Foundation/National Journal. 2011. Living Well at the End of Life: A National Conversation. Available from: http://www.regencefoundation.org/docs/FDRegenceNationalJournalSurveyResults.pdf
- [Google Scholar]






