Translate this page into:
The Palliative Performance Scale Predicts Survival among Emergency Department Patients, Minia, Egypt
Address for correspondence: Dr. Nashwa Nabil Kamal, Department of Public Health, Faculty of Medicine, Minia University, Egypt. E-mail: nashwakamal@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Emergency department (ED) physicians provide care to patients with a wide range of prognoses, and must develop care plans that anticipate patient's survival. However, the tools available to guide care planning had limited data to support their use. There is a new concern to understand if palliative care (PC) should be offered in the ED and the Palliative Performance Scale (PPS), a screening tool used in other settings in PC, has been little used in the ED.
Aim:
The aim of this study is to assess the prognostic value of the PPS in predicting 1, 3 and 6 months survival in patients admitted through the ED.
Design:
This was a prospective, cohort study.
Subjects and Methods:
We evaluated 147 patients at the age of 35 years and more admitted through the ED of Minia University hospital from May 1, 2016 to June 31, 2016. Each patient's PPS score was evaluated initially in the ED, with follow-up assessments of survival at 1, 3, and 6 months.
Results:
Baseline PPS for the 147 patients was 50. The PPS score was a strong predictor of survival (Log-rank test of Kaplan–Meir P < 0.0001). Patients with an initial PPS score of 40 or less were less likely to survive at 6 months.
Conclusion:
The PPS score may predict survival in patients admitted to the hospital through the ED. The ease of use holds promise that the use of the PPS in the ED may help ED physicians predict survival and plan for a better decision.
Keywords
Egypt
emergency
Palliative Performance Scale
survival
INTRODUCTION
Assessment and treatment of physical and psychosocial symptoms are essential components of high-quality palliative care (PC) practice.[1] However, PC is underdeveloped in Eastern Mediterranean Region (EMRO) compared to other regions of the world. As according to the “WHO global atlas of PC at the end-of-life” which classifies countries based on the level of PC development, none of the EMRO countries was classified in group 4 countries in which PC is integrated into mainstream service provision.[2]
Despite advances in medical diagnoses and therapies, symptoms remain a major source of distress to many terminally ill patients, which often are not well addressed and requiring significant attention and proper management.[3]
The culture of emergency medicine to provide stabilization of acute medical urgencies is now shifting to a more patient-goal-centered culture. There has been a large movement to educate emergency physicians on end-of-life care and improve PC in emergency medicine, leading to clinical practice guidelines.[4]
Patients with a serious, life-threatening illness and one or more of the following need a PC consult.[5]
-
Not Surprised
You would not be surprised if the patient died in the next 12 months.
-
Bounce-backs
The patient makes more than one emergency department (ED) visit or hospital admission for the same condition within several months.
-
Uncontrolled symptoms
An ED visit is prompted by difficult-to-control physical or emotional symptoms.
-
Functional decline
There is decline in function or worsening of feeding intolerance, unintentional weight loss, or caregiver distress.
-
Increasingly complicated
Complex long-term care needs require more support.
Emergency medicine physicians routinely manage patients with life-threatening illnesses while the primary concern of emergency medicine has been to provide life-sustaining treatment for the severely ill patient, these life-prolonging therapies may not necessarily be in concordance with patients' goals of care.[6] PC has been shown to improve the quality of life and patient and caregiver satisfaction, all while decreasing costs and length of stay.[78]
Survival estimates have important implications on the physician's provided care, decision-making, and treatment recommendations and also on a person's understanding of their illness, their expectations for the future, and the overall patient outcome.[9]
The Palliative Performance Scale (PPS) was designed to represent the functional or performance status among patients receiving PC, and it incorporates five parameters that are scored by an observer: ambulation, activity and/or evidence of disease, self-care, dietary intake, and level of consciousness.[10] A number of studies have reported a strongly positive relationship between PPS and survival duration in multiple settings[1112] but has limited use in the ED.[13]
The aim of the current study was to assess the prognostic value of the PPS in predicting 1-, 3-, and 6-month survival in patients in the ED.
SUBJECTS AND METHODS
Study design
This study was a prospective study conducted at the ED of an academic tertiary care facility between May 1, 2016 and June 31, 2016.
Participants
The study was conducted on patients admitted to Minia University Hospital through the ED. Those patients ≥35 years admitted for the 1st time were considered for inclusion; excluded from participation were prisoners, patients with a primary psychiatric or obstetric/gynecologic diagnosis, and patients referred to the ED from other departments. The recruitment was done 5 days a week during the study excluding the weekend. Eligible patients were identified in chronological order by which they were admitted.
We approached the doctor in the ED, discussed our study to get his agreement to meet the patients. If the patient then verbally agreed to be approached by the authors, we entered the room and began the enrollment process. The eligible patients were 152, but 147 patients were included, as the remaining five patients were lost to follow-up.
Data collection
The study included an interview assessing the following variables: PPS score, age, sex, marital status, residence, and primary diagnosis. For all patients, a PPS score was recorded at the time of enrollment. This score was recorded only once. The PPS was developed to measure five domains: (1) ambulation, (2) activity and evidence of disease, (3) independence in self-care, (4) oral intake, and (5) level of consciousness.[14] Each domain is arrayed on a scale from 10 (bedbound) to 100 (full ambulation).
A score of 0, corresponding to death, anchors the lower end of the scale. We conducted the study on 15 patients (a pilot study). The interrater reliability was high (κ = 0.87; P = 0.001). These patients were included in the study.
Follow-up
The goal was to indicate a survival estimate for enrolled patients at 1, 3, and 6 months after the initial enrollment. Each patient was contacted by phone. If the research author was unable to reach the patient, repeat phone calls were made over the following 7 days in an attempt to reach the patient. If after 1 week or 10 phone calls, the patient was still unable to be contacted; the patient was considered lost to follow-up. Total survival duration was calculated as the time between the date of initial visit and date of death. Deaths were identified through family, death certificate, or hospital medical records. The date of death was collected.
Data analysis
Summary statistics were generated to describe the distribution of PPS scores in the study sample, and survival was calculated for all PPS scores. We first tested the relationship between PPS score and survival with Kaplan–Meier survival test.
We calculated its ability to predict survival at 1, 3, and 6 months after enrollment. For these analyses, predictive accuracy was measured by calculating the area under the receiver operating characteristic (ROC) curve.[15]
Ethical considerations
The study protocol was approved by the Institution Research Ethical Committee. An approval of the administrator of ED was obtained. All participants gave verbal consent.
RESULTS
ED patients, who were admitted during May and June 2016, were enrolled in the study. They were 147 patients that met inclusion criteria. They were followed up through 6 months. At the time of closure, 86 participants remained alive. Demographic data including age, sex, education, occupation, and admission diagnosis were outlined in Table 1. The mean of age was 60 ± 25 years. Nearly 59.2% were female. 62.6% were rural dwellers. The most common cause of admission was cardiac disease (43.5%).
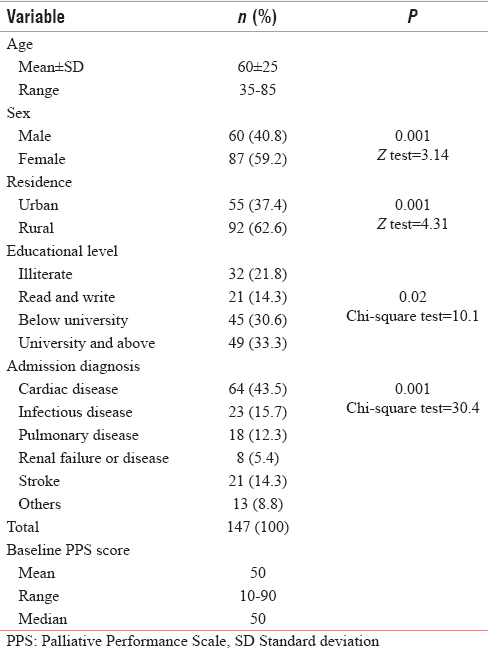
Among the study population, the median PPS at baseline was 50 with a range of 10–90.
The PPS was a good predictor of survival among the emergency adult patients with the sensitivity = 89.5% and specificity = 85.2% and the cutoff value >40 as shown in ROC curve [Figure 1].
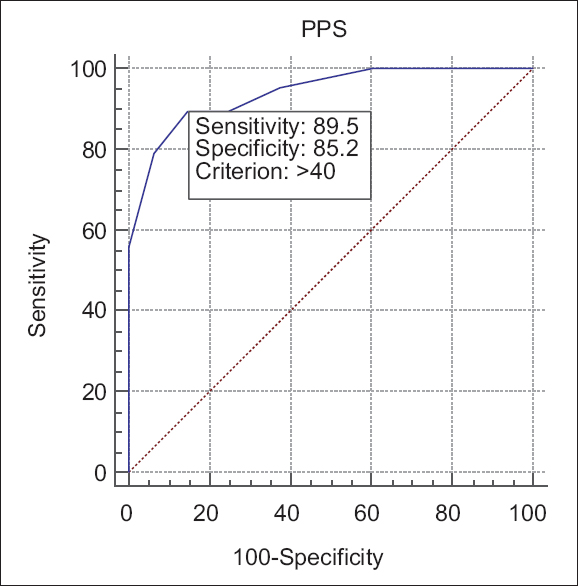
- Receiver operating characteristic analysis of Palliative Performance Scale in prediction of survival among emergency department patients
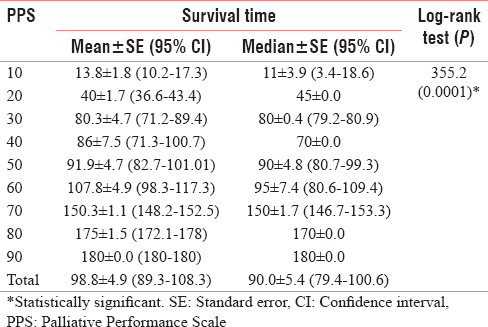
Kaplan–Meier analysis displayed the mean/median survival times, standard error, and 95% confidence interval (CI) for different PPS scores with log-rank test comparing the survival time of different scores and a significant difference was observed (P = 0.0001) as shown in Table 2. Mean survival time was 98.8 ± 4.9 and 95% CI was (89.3–108.3). Median survival time was 90.0 ± 5.4, and 95% CI was (79.4–100.6).
DISCUSSION
The present study examined the relationship between PPS and survival among patients in emergency care. Of 147 patients admitted to the ED, the mean PPS was 50 with a range of 10–90, and the mean survival time was 98.8 ± 4.9 days.
PC manages physical symptoms, prognostic awareness, and reduces psychological distress and so early access to PC is essential to increase the survival time.[16]
Our study is unique, in that our patients' age started from 35 years presenting to the ED. This was in contrast to a study[17] conducted among older adults aged over 55 years. Therefore, our study showed the suitability of PPS for prediction of survival in younger age.
In the present study, higher proportion of need of PC was among females (59.2%). This is may be because females have higher life expectancy.
Gómez-Batiste et al. also found a higher proportion of need among females (61.4%).[18]
The results of the current study showed that cardiac diseases were the most frequent cause of admission to the emergency care, followed by infectious diseases, and stroke. This finding was matched with a previous study which found that cardiac conditions and septicemia were top reasons for admission to the ED among adults aged 45 years and older.[19] However, in another previous study identified the most common disease condition in need of PC was old age-related weakness followed by chronic heart disease.[20]
The mean PPS at baseline was 50, and 41.4% were scored ≤40, which was slightly lower than a previous study done in the USA and found that the mean PPS score was 53.78, and 43 cases (43%) were scored 40 or less.[21]
PPS was found to be a good predictor of survival among the emergency adult patients with high sensitivity (89.5%) and specificity (85.2%) and the cutoff value >40. This finding was matched with many previous studies.[1117]
Our Kaplan–Meier analysis displayed different PPS scores with log-rank test comparing the survival time of different scores, and there was a significant difference observed (P = 0.0001). These results were similar to the previous studies and supported that the PPS score was a valid predictor of patients' survival.[222324] Harrold et al. found that the PPS score was more accurate in the prediction of survival among patients with a noncancer diagnosis.[25]
The main strength of our study is its prospective nature, and it is the first study that showed associations between survival and PPS among ED patients in Minia. However, there are limitations in this study. First, the study was performed in one tertiary hospital so study results cannot be generalized to every emergency care unit. Second, we included only limited variables of survival predictors which could influence on the study results. For high-quality evidence, a large-scaled longitudinal study is required.
CONCLUSION AND RECOMMENDATIONS
Our findings indicated that the PPS score was a predictor of survival when applied to the ED patients, and therefore, a useful screen for ED providers. It may have implications in early identification of patients who are at a high risk of death and may benefit from discussions about goals of treatment and alternate care options.
ED physicians faced considerable time pressures to provide the best possible care to patients and families in the last days of life. Therefore, it will be necessary to develop prognostic tools, the PPS that can guide care planning and help to ensure that patients and families will receive the services that they need during short lengths of stay.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank all the participants and ED physicians and nurses for their help.
REFERENCES
- Quality measures for hospice and palliative care: Piloting the PEACE measures. J Palliat Med. 2014;17:769-75.
- [Google Scholar]
- 2014. Global Atlas of Palliative Care at the End-of-Life. London: Worldwide Palliative Care Alliance; Available from: http://www.thewhpca.org/resources/global-atlas-on-end-of-life-care
- The symptom burden of patients with hematological malignancy: A cross-sectional observational study. J Pain Symptom Manage. 2011;42:432-42.
- [Google Scholar]
- 2011. Clinical Practice Guidelines: A Technical Assistance Resource from the IPAL-EM Project. New York: The IPAL-EM Project, Center to Advance Palliative Care; Available from: http://www.ipal.capc.org/downloads/ipal-em-clinical-practice-guidelines.pdf
- 2011. Palliative Care ED Screening Tool: A Technical Assistance Resource from the IPAL-EM Project. New York: The IPAL-EM Project, Center to Advance Palliative Care; Available from: http://www.ipal.capc.org/downloads/ipal-em-palliative-care-ed-screening-tool.pdf
- Palliative care needs of seriously ill, older adults presenting to the emergency department. Acad Emerg Med. 2010;17:1253-7.
- [Google Scholar]
- Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 2008;168:1783-90.
- [Google Scholar]
- Increased satisfaction with care and lower costs: Results of a randomized trial of in-home palliative care. J Am Geriatr Soc. 2007;55:993-1000.
- [Google Scholar]
- Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: Results of a randomized study of early palliative care. J Clin Oncol. 2011;29:2319-26.
- [Google Scholar]
- Use of the Palliative Performance Scale (PPS) for end-of-life prognostication in a palliative medicine consultation service. J Pain Symptom Manage. 2009;37:965-72.
- [Google Scholar]
- Value of the Palliative Performance Scale in the prognostication of advanced cancer patients in a tertiary care setting. J Palliat Med. 2013;16:887-93.
- [Google Scholar]
- Preliminary report of a palliative care and case management project in an emergency department for chronically ill elderly patients. J Urban Health. 2008;85:443-51.
- [Google Scholar]
- Palliative Performance Scale (PPSv2) version 2. In: Medical Care of the Dying (4th ed). ©Victoria Hospice Society; 2006. p. :120.
- [Google Scholar]
- The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29-36.
- [Google Scholar]
- Early integration of palliative care services with standard oncology care for patients with advanced cancer. CA Cancer J Clin. 2013;63:349-63.
- [Google Scholar]
- The Palliative Performance Scale predicts three- and six-month survival in older adult patients admitted to the hospital through the emergency department. J Palliat Med. 2016;19:1087-91.
- [Google Scholar]
- Prevalence and characteristics of patients with advanced chronic conditions in need of palliative care in the general population: A cross-sectional study. Palliat Med. 2014;28:302-11.
- [Google Scholar]
- Estimation of palliative care need in the urban community of Puducherry. Indian J Palliat Care. 2017;23:81-87.
- [Google Scholar]
- Overview of Emergency Department Visits in the United States, 2011. 2014. HCUP Statistical Brief #174. Rockville, MD: Agency for Healthcare Research and Quality; Available from: http://www.hcup.us.ahrq.gov/reports/statbriefs/sb174-Emergency-Department-Visits-Overview.pdf
- [Google Scholar]
- Enhancing provider knowledge and patient screening for palliative care needs in chronic multimorbid patients receiving home-based primary care. Am J Hosp Palliat Care. 2015;32:78-83.
- [Google Scholar]
- Validity of the palliative performance scale from a survival perspective. J Pain Symptom Manage. 1999;18:2-3.
- [Google Scholar]
- Validation of the palliative performance scale for inpatients admitted to a palliative care unit in Sydney, Australia. J Pain Symptom Manage. 2002;23:455-7.
- [Google Scholar]
- Validation of the palliative performance scale in the acute tertiary care hospital setting. J Palliat Med. 2007;10:111-7.
- [Google Scholar]
- Is the Palliative Performance Scale a useful predictor of mortality in a heterogeneous hospice population? J Palliat Med. 2005;8:503-9.
- [Google Scholar]






